Abstract
Purpose
To explore the consistency in international expert opinions about palliative sedation.
Methods
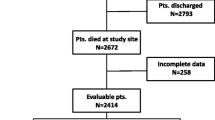
A modified electronic-Delphi procedure was carried out in two rounds. On hundred nine eligible experts were identified from their publications in MEDLINE related with terminal delirium, dyspnea and palliative sedation in the last 3 years. Delphi study included three vignettes of cancer patients and two non-cancer patients, with an estimated survival of days and severe suffering secondary to refractory complications. Experts were asked about whether they would perform continuous sedation and sedation level (described as Richmond Agitation Sedation Scale or defined as patient/family report of symptom relief). Consensus was considered when 70% or more of the experts agreed on a certain topic.
Results
Thirty-four and 27 panellists completed the 2 Delphi rounds, respectively. Participants were from the USA, Canada, Europe, Australia and Asia. One hundred per cent, 97% and 88% of the respondent agreed use of sedatives, continuously or temporary, in cases of refractory delirium, dyspnea secondary to lung cancer and GOLD IV-EPOC. There were discrepancies for cases of dementia and psycho-existential suffering. Expert selection of continuous palliative sedation was 93% for delirium, 41% for cancer dyspnea, 66% for EPOC dyspnea, 22% for agitation/pain in dementia and 19% for existential suffering. Responses about types and levels of sedation did not achieve consensus in any cases.
Conclusions
The Delphi study failed to reach consensus in continuous palliative sedation and sedation levels for patients with refractory symptoms described in hypothetical clinical scenarios.

Similar content being viewed by others
References
Cherny NI, Radbruch L, Board of the European Association for Palliative Care (2009) European Association for Palliative Care (EAPC) recommended framework for the use of sedation in palliative care. Palliat Med 23:581–593
Kirk TW, Mahon MM, Palliative Sedation Task Force of the National Hospice and Palliative Care Organization Ethics Committee (2010) National Hospice and Palliative Care Organization (NHPCO) position statement and commentary on the use of palliative sedation in imminently dying terminally ill patients. J Pain Symptom Manag 39:914–923
Cherny NI, ESMO Guidelines Working Group (2014) ESMO clinical practice guidelines for the management of refractory symptoms at the end of life and the use of palliative sedation. Ann Oncol 25(Suppl 3):143–152
Quill TE, Lo B, Brock DW, Meisel A (2009) Last-resort options for palliative sedation. Ann Intern Med 151:421–424
Maltoni M, Setola E (2015) Palliative sedation in patients with cancer. Cancer Control 22:433–441
Morita T, Imai K, Yokomichi N, Mori M, Kizawa Y, Tsuneto S (2017) Continuous deep sedation: a proposal for performing more rigorous empirical research. J Pain Symptom Manag 53:146–152
Anquinet L, Rietjens JA, Seale C et al (2012) The practice of continuous deep sedation until death in Flanders (Belgium), the Netherlands, and the UK: a comparative study. J Pain Symptom Manag 44:33–43
Swart SJ, Van der Heide A, Van Zuylen L et al (2012) Considerations of physicians about the depth of palliative sedation at the end of life. CMAJ 184:360–366
Seymour J, Rietjens J, Bruinsma S, UNBIASED consortium et al (2015) Using continuous sedation until death for cancer patients: a qualitative interview study of physicians’ and nurses’ practice in three European countries. Palliat Med 29:48–59
Materstvedt LJ, Bosshard G (2009) Deep and continuous palliative sedation (terminal sedation): clinical-ethical and philosophical aspects. Lancet Oncol 10:622–627
Sykes N, Thorns A (2003) Sedative use in the last week of life and the implications for end-of-life decision making. Arch Intern Med 163:341–344
Twycross R (2017) Regarding palliative sedation. J Pain Symptom Manag 53:e13–e15
Juth N, Lindblad A, Lynöe N, Sjöstrand M, Helgesson G (2010) European Association for Palliative Care (EAPC) framework for palliative sedation: an ethical discussion. BMC Palliat Care 9:20–25
Billings JA, Churchill LR (2012) Monolithic moral frameworks: how are the ethics of palliative sedation discussed in the clinical literature? J Palliat Med 15:709–713
Berger JT (2014) The proportionate value of proportionality in palliative sedation. J Clin Ethics 25:219–221
Claessens P, Menten J, Schotsmans P, Broeckaert B (2008) Palliative sedation: a review of the research literature. J Pain Symptom Manag 36:310–333
Schildmann E, Schildmann J (2014) Palliative sedation therapy: a systematic literature review and critical appraisal of available guidance on indication and decision making. J Palliat Med 17:601–611
Abarshi E, Rietjens J (2017) Robijn L, et al; EURO IMPACT international variations in clinical practice guidelines for palliative sedation: a systematic review. BMJ Support Palliat Care 7:223–229
Hamano J, Morita T, Ikenaga M, Abo H, Kizawa Y, Tunetou S (2018) A nationwide survey about palliative sedation involving Japanese palliative care specialists: intentions and key factors used to determine sedation as proportionally appropriate. J Pain Symptom Manag 55:785–791
Putman MS, Yoon JD, Rasinski KA, Curlin FA (2013) Intentional sedation to unconsciousness at the end of life: findings from a national physician survey. J Pain Symptom Manag 46:326–334
McMillan SS, King M, Tully MP (2016) How to use the nominal group and Delphi techniques. Int J Clin Pharm 38(3):655–662
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67:401–409
Rys S, Deschepper R, Mortier F, Deliens L, Bilsen J (2014) Continuous sedation until death with or without the intention to hasten death—a nationwide study in nursing homes in Flanders, Belgium. J Am Med Dir Assoc 15:570–575
Beller EM, van Driel ML, McGregor L, Truong S, Mitchell G (2015) Palliative pharmacological sedation for terminally ill adults. Cochrane Database Syst Rev 1:CD010206
Schildmann EK, Schildmann J, Kiesewetter I (2015) Medication and monitoring in palliative sedation therapy: a systematic review and quality assessment of published guidelines. J Pain Symptom Manag 49:734–746
Arevalo JJ, Brinkkemper T, van der Heide A, AMROSE Site Study Group et al (2012) Palliative sedation: reliability and validity of sedation scales. J Pain Symptom Manag 44:704–714
Fainsinger RL, Waller A, Bercovici M, Bengtson K, Landman W, Hosking M, Nunez-Olarte JM, deMoissac D (2000) A multicentre international study of sedation for uncontrolled symptoms in terminally ill patients. Palliat Med 14:257–265
Chiu TY, Hu WY, Lue BH, Cheng SY, Chen CY (2001) Sedation for refractory symptoms of terminal cancer patients in Taiwan. J Pain Symptom Manag 21:467–472
Morita T, Chinone Y, Ikenaga M, Japan Pain, Palliative Medicine, Rehabilitation, and Psycho-Oncology Study Group et al (2005) Efficacy and safety of palliative sedation therapy: a multicenter, prospective, observational study conducted on specialized palliative care units in Japan. J Pain Symptom Manag 30:320–328
Imai K, Morita T, Yokomichi N et al (2017) Efficacy of two types of palliative sedation therapy defined using intervention protocols: proportional vs. deep sedation. Support Care Cancer. https://doi.org/10.1007/s00520-017-4011-2
Acknowledgments
We thank our expert, F. Asís González Garcia-Estrada, for its valuable work in the e-survey. We would especially like to acknowledge experts for their contributions to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Human Research Ethics Committee of Hospital Universitario La Candelaria. For this type of study formal consent is not required.
Informed consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Appendices
Appendix 1. Vignettes
1. Seventy-four-year-old woman with end-stage pancreatic cancer and liver failure, irreversible hyperactive delirium with significant psychomotor agitation and no response to levomepromazine 300 mg/day combined with intermittent use of benzodiazepines. Oligoanuria, impaired intake. PPS 10. Twenty-four breaths per minute, 105 beats per minute, oxygen saturation of 85%, death rattle in both lung fields. The estimated survival of the patient is “days” according to the Prognosis in Palliative Care Study predictor model-A. She has previously stated to agree to receive pharmacological agents to reduce consciousness in order to relieve the suffering in the last days of her life. Her family has agreed to respect her decision.
2. Forty-four-year-old male with end-stage lung cancer, bedridden and dependent for all basic activities of daily living due to severe respiratory failure with continuous dyspnoea at rest refractory to all treatments, including parenteral opioids and oxygen. The patient is alert and not depressed. No delirium. Presence of premortem wheezing with an oxygen saturation of 89% and a breathing rate of 28 breaths/min. PPS 10%. Using the Prognosis in Palliative Care Study predictor model-A, the estimated survival of the patient is days. He has explicitly stated to his physician, “I want to die right without any suffering. I agree to sleep until I die if it is necessary”. His family has agreed to respect his decision.
3. Sixty-four-year-old male with end-stage GOLD IV COPD. Bedridden and dependent for all basic activities of daily living due to severe respiratory failure with continuous dyspnoea at rest (impaired oral intake and communication) refractory to all treatments, including antibiotic, opioids and NIMV. The patient is alert and not depressed. No delirium. Twenty-eight breaths per minute, oxygen saturation of 86% despite of adequate oxygen therapy, 110 beats per minute. Presence of death rattle. Estimated survival of less than 3–4 days. The patient has been informed of his diagnosis, conditions of his illness, and prognosis. He has explicitly and repeatedly stated to his physician, “I want you to help die right without suffering by my inability to get enough air, if possible. If you can’t do that, then I want to be unconscious until I die”.
4. Eighty-six-year-old patient with end-stage of Alzheimer’s disease (stage 7f on the Reisberg scale). Eyes remain open. Presents with foetal position and interrupted whimpers when moving, which make the staff caring for him doubt whether he is suffering, in spite of increasing the dosage of morphine to 60 mg/day. Estimated survival of 2–4 days, presence of oligoanuria, premortem wheezing, 28 breaths per minute, oxygen saturation of 84%, 102 beats per minute. His family feels that he is suffering.
5. Thirty-six-year-old patient with end-stage cervical cancer. Presents with symptoms of irreversible complete intestinal obstruction, which has lasted for 20 days. Controlled vomiting and pain; abscessified tumour implant in the abdominal wall with enterocutaneous fistula. In addition, rectovaginal fistula, with fecaloid vaginal discharge. Irreversible coagulopathy with a high risk of massive bleeding. Bedridden due to neoplastic asthenia with a score of 8/10 on the VAS and requires help for all basic ADLs. Palliative Performance Scale 20%. She is alert; no sign of delirium. The estimated survival of the patient is days according to the Prognosis in Palliative Care Study predictor model-A. When informed of the diagnosis and the prognosis of days, the patient expresses a desire to end her life due to spiritual distress. She feels like she is a burden and expresses profound despair. As a result, she requests to be asleep during the final days of her life, in mutual agreement with her family. She does not recognise the presence of emotional disturbance, and her score on the hospital scale of anxiety and depression is 10 points.
Appendix 2. Questions regarding clinical scenarios
Question 1. Faced with the clinical situation, your treatment plan would be:
-
Perform continuous sedation (CPS), a state of decreased or absent awareness in different levels (proportional, light, moderate or deep sedation), until death
-
Perform only transitory/intermittent sedation (transitory state of decreased or absent awareness) in situations of exacerbations of severe dyspnoea, but not continuous sedation
-
None of the above options, I would select other treatments
Question 2. If you decide to perform continuous sedation until death, you would do so in the following manner…
-
I would initiate continuous sedation quickly in order to decrease awareness within 30–60 min
-
I would initiate sedation slowly and progressively to decrease awareness in a few hours
-
Using repeated dosing of a sedative, I would titrate sedation to a level where that patient indicated they have adequate relief, and then maintain the level with a continual infusion titrated to patient report of adequacy
-
I would not perform sedation (I would not reduce patient’s consciousness level), I would select other treatments
Question 3. If you perform continuous sedation until death, the level/depth of sedation, which you consider appropriate for the patient, would be…
-
Complete sedation (the patient does not respond to any stimuli: RASS -5 or level 6 on the Ramsay sedation scale)
-
Deep sedation (the patient responds to tactile stimuli with eye opening or body movements: RASS-4 or level 5 on the Ramsay sedation scale)
-
Moderate sedation (the patient responds to verbal stimuli with eye opening or body movements: RASS-3 or level 4 on the Ramsay sedation scale)
-
Mild sedation (the patient responds to verbal stimuli with eye contact: RASS-2 or level 3 on the Ramsay sedation scale)
-
Using repeated dosing of a sedative, I would titrate sedation to a level where that patient indicated they have adequate relief, and then maintain the level with a continual infusion titrated to patient report of adequacy
-
None of the above options
-
I would not perform palliative sedation (I would not reduce patient’s consciousness level), I would select other treatments
Rights and permissions
About this article
Cite this article
Benítez-Rosario, M.A., Morita, T. Palliative sedation in clinical scenarios: results of a modified Delphi study. Support Care Cancer 27, 1647–1654 (2019). https://doi.org/10.1007/s00520-018-4409-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4409-5