Abstract
Objectives
To evaluate the existing body of evidence to determine the current state of knowledge regarding the perspectives of the following groups: (1) children with cancer, (2) family caregivers, and (3) healthcare professionals, about symptoms, as well as factors that may influence the symptom reports.
Methods
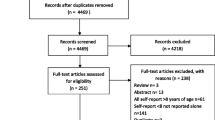
A systematic search was performed for all types of studies that included the perspectives of at least two groups of participants’ symptom reports. Children included anyone younger than 19 years of age who was diagnosed with any type of cancer. Electronic searches were conducted in five English databases and four Chinese databases. The appraisal of methodological quality was conducted using the GRADE criteria. Data were extracted into matrix tables.
Results
Thirty-three studies were included. The pediatric oncology symptoms reported by children, family caregivers, and healthcare professionals were synthesized. Findings suggested that family caregivers’ symptom reports were more closely aligned with children’s reports than with the healthcare professionals’ reports. Influencing factors on the different symptom reports included the children’s diagnosis, symptom characteristics, social-demographic factors, and family caregivers’ psychosocial status.
Conclusions
Children with cancer should be the primary reporters for their symptoms. When there are reporters other than the children, the potential discrepancy between the different perspectives needs to be carefully considered.

Similar content being viewed by others
References
Zhukovsky DS, Rozmus CL, Robert RS, Bruera E, Wells RJ, Chisholm GB, Allo JA, Cohen MZ (2015) Symptom profiles in children with advanced cancer: patient, family caregiver, and oncologist ratings. Cancer 121(22):4080–4087. https://doi.org/10.1002/cncr.29597
Baggott C, Dodd M, Kennedy C, Marina N, Miaskowski C (2009) Multiple symptoms in pediatric oncology patients: a systematic review. J Pediatr Oncol Nurs : Off J Assoc Pediatr Oncol Nurses 26(6):325–239. https://doi.org/10.1177/1043454209340324
Varni JW, Limbers C, Burwinkle TM (2007) Literature review: health-related quality of life measurement in pediatric oncology: hearing the voices of the children. J Pediatr Psychol 32(9):1151–1163. https://doi.org/10.1093/jpepsy/jsm008
Linder LA (2008) Developmental diversity in symptom research involving children and adolescents with cancer. J Pediatr Nurs 23(4):296–309. https://doi.org/10.1016/j.pedn.2007.10.003
Baggott C, Cooper BA, Marina N, Matthay KK, Miaskowski C (2014) Symptom assessment in pediatric oncology: how should concordance between children’s and parents’ reports be evaluated? Cancer Nurs 37(4):252–262. https://doi.org/10.1097/ncc.0000000000000111
Hinds PS, Menard JC, Jacobs SS (2012) The child’s voice in pediatric palliative and end-of-life care. Progress Palliative Care 20(6):337–342. https://doi.org/10.1179/1743291X12Y.0000000035
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (London, England) 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Andrews J, Guyatt G, Oxman AD, Alderson P, Dahm P, Falck-Ytter Y, Nasser M, Meerpohl J, Post PN, Kunz R, Brozek J, Vist G, Rind D, Akl EA, Schunemann HJ (2013) GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol 66(7):719–725. https://doi.org/10.1016/j.jclinepi.2012.03.013
Matziou V, Vlachioti E, Megapanou E, Ntoumou A, Dionisakopoulou C, Dimitriou V, Tsoumakas K, Matziou T, Perdikaris P (2016) Perceptions of children and their parents about the pain experienced during their hospitalization and its impact on parents’ quality of life. Jpn J Clin Oncol 46(9):862–870. https://doi.org/10.1093/jjco/hyw074
Zernikow B, Meyerhoff U, Michel E, Wiesel T, Hasan C, Janssen G, Kuhn N, Kontny U, Fengler R, Gortitz I, Andler W (2005) Pain in pediatric oncology—children’s and parents’ perspectives. Eur J Pain (London, England) 9(4):395–406. https://doi.org/10.1016/j.ejpain.2004.09.008
Hechler T, Chalkiadis GA, Hasan C, Kosfelder J, Meyerhoff U, Vocks S, Zernikow B (2009) Sex differences in pain intensity in adolescents suffering from cancer: differences in pain memories? J Pain : Off J Am Pain Soc 10(6):586–393. https://doi.org/10.1016/j.jpain.2008.11.011
Collins JJ, Devine TD, Dick GS, Johnson EA, Kilham HA, Pinkerton CR, Stevens MM, Thaler HT, Portenoy RK (2002) The measurement of symptoms in young children with cancer: the validation of the memorial symptom assessment scale in children aged 7-12. J Pain Symptom Manag 23(1):10–16. https://doi.org/10.1016/S0885-3924(01)00375-X
Hinds PS, Gattuso JS, Billups CA, West NK, Wu JR, Rivera C, Quintana J, Villarroel M, Daw NC (2009) Aggressive treatment of non-metastatic osteosarcoma improves health-related quality of life in children and adolescents. Eur J Cancer 45(11):2007–2014. https://doi.org/10.1016/j.ejca.2009.04.020
Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT, Polyak T, Rapkin B, Portenoy RK (2000) The measurement of symptoms in children with cancer. J Pain Symptom Manag 19(5):363–377. https://doi.org/10.1016/S0885-3924(00)00127-5
Sato I, Higuchi A, Yanagisawa T, Mukasa A, Ida K, Sawamura Y, Sugiyama K, Saito N, Kumabe T, Terasaki M, Nishikawa R, Ishida Y, Kamibeppu K (2014) Cancer-specific health-related quality of life in children with brain tumors. Qual Life Res: An Int J Qual Life Asp Treat Care Rehabil 23(4):1059–1068. https://doi.org/10.1007/s11136-013-0555-x
Liossi C, White P, Franck L, Hatira P (2007) Parental pain expectancy as a mediator between child expected and experienced procedure-related pain intensity during painful medical procedures. Clin J Pain 23(5):392–399. https://doi.org/10.1097/AJP.0b013e31804ac00c
Van Cleve L, Munoz CE, Riggs ML, Bava L, Savedra M (2012) Pain experience in children with advanced cancer. J Pediatr Oncol Nurs 29(1):28–36. https://doi.org/10.1177/1043454211432295
Van Cleve L, Munoz CE, Savedra M, Riggs M, Bossert E, Grant M, Adlard K (2012) Symptoms in children with advanced cancer child and nurse reports. Cancer Nurs 35(2):115–125. https://doi.org/10.1097/NCC.0b013e31821aedba
Pu X, Ye Q, Liu K, You L (2015) The application of Chinese version of PedsQLTMMultidimensional fatigue scale in children with leukemia. Chin J Pract Nurs 31(5):323–326
Gerçeker GO, Yilmaz HB (2012) Reliability and validity of Turkish versions of the child, parent and staff cancer fatigue scales. Asian Pac J Cancer Prev: APJCP 13(7):3135–3141. https://doi.org/10.7314/APJCP.2012.13.7.3135
Whitsett SF, Gudmundsdottir M, Davies B, McCarthy P, Friedman D (2008) Chemotherapy-related fatigue in childhood cancer: correlates, consequences, and coping strategies. J Pediatr Oncol Nurs 25(2):86–96. https://doi.org/10.1177/1043454208315546
Hockenberry MJ, Hinds PS, Barrera P, Bryant R, Adams-McNeill J, Hooke C, Rasco-Baggott C, Patterson-Kelly K, Gattuso JS, Manteuffel B (2003) Three instruments to assess fatigue in children with cancer: the child, parent and staff perspectives. J Pain Symptom Manag 25(4):319–328. https://doi.org/10.1016/S0885-3924(02)00680-2
Hinds PS, Hockenberry M, Tong X, Rai SN, Gattuso JS, McCarthy K, Pui CH, Srivastava DK (2007) Validity and reliability of a new instrument to measure cancer-related fatigue in adolescents. J Pain Symptom Manag 34(6):607–618. https://doi.org/10.1016/j.jpainsymman.2007.01.009
Yilmaz HB, Gerçeker GO, Muslu GK (2016) Evaluating the cancer related fatigue by children, mothers, and nurses in Turkish pediatric oncology patients. Eur J Oncol Nurs 23:66–71. https://doi.org/10.1016/j.ejon.2016.05.002
Nascimento LC, Nunes MDR, Rocha EL, Bomfim EO, Floria-Santos M, dos Santos CB, dos Santos D, de Lima RAG (2015) High validity and reliability of the PedsQL (TM) multidimensional fatigue scale for Brazilian children with cancer. J Pediatr Oncol Nurs 32(1):57–64. https://doi.org/10.1177/1043454214554656
Yeh CH, Chiang YC, Lin L, Yang CP, Chien LC, Weaver MA, Chuang HL (2008) Clinical factors associated with fatigue over time in paediatric oncology patients receiving chemotherapy. Br J Cancer 99(1):23–29. https://doi.org/10.1038/sj.bjc.6604434
Hinds PS, Hockenberry-Eaton M, Gilger E, Kline N, Burleson C, Bottomley S, Quargnenti A (1999) Comparing patient, parent, and staff descriptions of fatigue in pediatric oncology patients. Cancer Nurs 22(4):277–289. https://doi.org/10.1097/00002820-199908000-00004
Tyc VL, Mulhern RK, Fairclough D, Ward PM, Relling MV, Longmire W (1993) Chemotherapy induced nausea and emesis in pediatric cancer patients: external validity of child and parent emesis ratings. J Dev Behav Pediatr 14(4):236–241
Lo LH, Hayman LL (1999) Parents associated with children in measuring acute and delayed nausea and vomiting. Nurs Health Sci 1(3):155–161. https://doi.org/10.1046/j.1442-2018.1999.00020.x
Rodgers C, Kollar D, Taylor O, Bryant R, Crockett K, Gregurich MA, Hockenberry M (2012) Nausea and vomiting perspectives among children receiving moderate to highly emetogenic chemotherapy treatment. Cancer Nurs 35(3):203–210. https://doi.org/10.1097/NCC.0b013e3182281493
Walco GA, Conte PM, Labay LE, Engel R, Zeltzer LK (2005) Procedural distress in children with cancer: self-report, behavioral observations, and physiological parameters. Clin J Pain 21(6):484–490
Zhou Y, Lou J, Feng F (2013) The difference in assessment of quality of life between child self-report and parent proxy-report on the pediatric quality of life inventory measurement. Shanghai Nursing 13(1):18–21
Bemis H, Yarboi J, Gerhardt CA, Vannatta K, Desjardins L, Murphy LK, Rodriguez EM, Compas BE (2015) Childhood cancer in context: sociodemographic factors, stress, and psychological distress among mothers and children. J Pediatr Psychol 40(8):733–743. https://doi.org/10.1093/jpepsy/jsv024
Mulhern RK, Fairclough DL, Smith B, Douglas SM (1992) Maternal depression, assessment methods, and physical symptoms affect estimates of depressive symptomatology among children with cancer. J Pediatr Psychol 17(3):313–326. https://doi.org/10.1093/jpepsy/17.3.313
Eiser C, Havermans T, Craft A, Kernahan J (1995) Development of a measure to assess the perceived illness experience after treatment for cancer. Arch Dis Child 72(4):302–307
Varni JW, Seid M, Rode CA (1999) The PedsQL (TM): measurement model for the pediatric quality of life inventory. Med Care 37(2):126–139. https://doi.org/10.1097/00005650-199902000-00003
Levine DR, Mandrell BN, Sykes A, Pritchard M, Gibson D, Symons HJ, Wendler D, Baker JN (2017) Patients’ and parents’ needs, attitudes, and perceptions about early palliative care integration in pediatric oncology. JAMA Oncol 3:1214–1220. https://doi.org/10.1001/jamaoncol.2017.0368
Baggott C, Baird J, Hinds P, Ruland CM, Miaskowski C (2015) Evaluation of Sisom: a computer-based animated tool to elicit symptoms and psychosocial concerns from children with cancer. Eur J Oncol Nurs 19(4):359–369. https://doi.org/10.1016/j.ejon.2015.01.006
Hedström M, Haglund K, Skolin I, von Essen L (2003) Distressing events for children and adolescents with cancer: child, parent, and nurse perceptions. J Pediatr Oncol Nurs 20(3):120–132
O'Sullivan C, Dupuis LL, Gibson P, Johnston DL, Baggott C, Portwine C, Spiegler B, Kuczynski S, Tomlinson D, Tomlinson GA, Sung L (2016) Evaluation of the electronic self-report symptom screening in pediatrics tool (SSPedi). BMJ Support Palliat Care 8:110–116. https://doi.org/10.1136/bmjspcare-2015-001084
Dupuis LL, Johnston DL, Baggott C, Hyslop S, Tomlinson D, Gibson P, Orsey A, Dix D, Price V, Vanan M, Portwine C, Kuczynski S, Spiegler B, Tomlinson GA, Sung L (2017) Validation of the symptom screening in pediatrics tool in children receiving Cancer treatments. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djx250
Ameringer S, Erickson JM, Macpherson CF, Stegenga K, Linder LA (2015) Symptoms and symptom clusters identified by adolescents and young adults with cancer using a symptom heuristics app. Res Nursing Health 38(6):436–448. https://doi.org/10.1002/nur.21697
Vatne TM, Slaugther L, Ruland CM (2010) How children with cancer communicate and think about symptoms. J Pediatr Oncol Nurs : Off J Assoc Pediatr Oncol Nurses 27(1):24–32. https://doi.org/10.1177/1043454209349358
Acknowledgements
The authors would like to thank Jamie Conklin, MSLIS, Prof Library Staff, Medical Center Library and Archives, School of Medicine, Duke University for her invaluable assistance with the literature search strategy and Marion. E. Broome PhD, RN, FAAN, Dean and Ruby F. Wilson Professor of Nursing, School of Nursing, Duke University, for her thoughtful comments and constructive suggestions during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Cheng, L., Wang, L., He, M. et al. Perspectives of children, family caregivers, and health professionals about pediatric oncology symptoms: a systematic review. Support Care Cancer 26, 2957–2971 (2018). https://doi.org/10.1007/s00520-018-4257-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4257-3