Summary
Introduction
The impact of asthma and chronic obstructive pulmonary disease (COPD) in the setting of severe acute respiratory syndrome coronavirus 2 (SARS-CoV‑2) infection is not clearly defined. Blood eosinophil count is a standard diagnostic test which, according to the previously published literature, might have a potential prognostic role on mortality in patients with SARS-CoV‑2 infection.
Aim
To investigate the potential prognostic value of peripheral blood eosinophil count on all-cause mortality of patients hospitalized with SARS-CoV‑2 infection, as well as to assess the impact of asthma or COPD premorbidity on all-cause mortality.
Material and methods
We conducted a retrospective registry-based cohort study. Survival analysis was performed by employing the Cox proportional hazards regression model at 30 days of follow-up. Prognostic value of eosinophil count on all-cause mortality was assessed using receiver-operating characteristic (ROC) curve analysis.
Results
A total of 5653 participants were included in the study. Our model did not reveal that pre-existing asthma or COPD is a statistically significant covariate for all-cause mortality but, indicated that higher eosinophil count at admission might have a protective effect (hazard ratio, HR 0.13 (95% confidence interval, CI 0.06–0.27), p = 0.0001). ROC curve analysis indicates cut-off value of 20 cells/mm3 (81% specificity; 30.9% sensitivity).
Conclusion
Our results indicate that eosinophil count at hospital admission might have a potential prognostic role for all-cause mortality at 30 days of follow-up; however this was not demonstrated for pre-existing obstructive lung diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Obstructive pulmonary diseases are a group of disorders boasting a key feature of expiratory airflow limitation, which can either be fixed or variable. The most important obstructive lung diseases are asthma and chronic obstructive pulmonary disease (COPD) [1]. Asthma is, as defined by the Global Initiative for Asthma (GINA), a heterogeneous disease characterized by chronic airway inflammation and defined by respiratory symptoms (wheezing, shortness of breath, chest tightness and cough), which are variable in time and intensity, and by expiratory airflow limitation [2]. Asthma is a common disease, with a broad estimate that 1–18% of the world population suffer from it. Furthermore, asthma prevalence is increasing in both pediatric and adult populations [2,3,4]. COPD is a disease characterized by persistent respiratory symptoms and airflow limitation which are due to airway/alveolar abnormalities caused by exposure to noxious stimuli and facilitated by host factors [5], a major risk factor for its development is tobacco smoking [6]. COPD is the third leading cause of death worldwide. In addition, people suffering from COPD often have multiple other comorbidities [7,8,9,10]. It is worth mentioning that asthma and COPD might coexist: asthma/COPD overlap (ACO) is a descriptor term for patients with clinical features of both diseases. ACO is not considered a single disease entity, but rather a common term for a plethora of overlapping phenotypes [2, 11, 12]. (Previously used term asthma and COPD overlap syndrome (ACOS) has been abolished by GOLD and GINA; however, as already mentioned GINA still uses ACO for concomitant asthma and COPD [2, 13].) Asthma and COPD have been implicated as potential risk factors for worse outcomes in those suffering from COVID-19; however, there is conflicting evidence regarding the subject [14,15,16,17,18].
Eosinophils are blood granulocytes that normally make less than 5% of circulating leukocytes. Eosinophil count is a routinely performed investigation, as part of the differential blood count. In clinical practice, eosinophilia is most commonly associated with atopy and parasitic infections; however, a plethora of other causes for eosinophilia have been identified [19, 20]. Furthermore, eosinophilia (as a marker of underlying eosinophilic inflammation) has a prominent diagnostic and phenotyping role in asthma, and an emerging role in COPD management [2, 5, 21,22,23,24]. Since the beginning of the SARS-CoV‑2 pandemic, several studies recognized the potential role of eosinophil count in disease prognosis, mostly associating eosinopenia with poor outcomes [25,26,27,28]. Additionally, eosinopenia has also been associated with poor outcomes in patients with bacterial infections [29, 30].
We aimed to investigate the potential role of common obstructive lung diseases (asthma and COPD) on all-cause mortality in patients with SARS-CoV‑2 infection, as well as to assess the prognostic role of eosinophil count at admission. Therefore, we conducted a retrospective cohort study based on our registry that has included consecutive patients hospitalized with SARS-CoV‑2 positive test since the beginning of the pandemic in our tertiary and leading national COVID-19 center. We hypothesized that asthma, COPD and eosinopenia might be potential contributors of all-cause mortality.
Material and methods
This study was approved by the Ethics Committee of the University Hospital Dubrava (No. 2021/2503–04). This study was designed as a single center retrospective cohort study based on the Registry of Hospitalized Patients in University Hospital Dubrava Respiratory Center (ClinicalTrials.gov Identifier: NCT05151094), which included consecutive patients hospitalized with SARS-CoV‑2 positivity in the University Hospital Dubrava, a tertiary center, which has been designated shortly after the beginning of the pandemic as the principal and largest COVID-19 center in Croatia [31, 32].
Consecutive patients who were admitted to the University Hospital Dubrava from 24 March 2020 to 8 June 2021 were screened for the following eligibility criteria: the inclusion criteria included: a) patients that are 18 years of age or older at admission, b) SARS-CoV‑2 positive patients, c) first hospitalization with SARS-CoV‑2 positive test. The exclusion criteria were a) missing data regarding obstructive disease information or eosinophil count at admission, b) missing data regarding hospitalization outcome. Study participants were analyzed as a cohort and then divided into four subgroups, participants with a) no known obstructive lung disease (NOD), b) pre-existing asthma, c) pre-existing COPD and d) pre-existing ACO.
Statistical analyses were performed in MedCalc® Statistical Software version 20.106 (MedCalc Software Ltd, Ostend, Belgium) and JAMOVI 2020 (The jamovi project, Sydney, Australia) [33, 34]. Type one error (α) was set to 0.05. For presenting descriptive statistics, quantitative parametric variables are presented as mean ± standard deviation (SD), non-parametric variables are presented as median (1st–3rd quartile, Q1–Q3). Data normality was tested both informally by plotting histograms and distribution curves, as well as formally using Kolmogorov-Smirnov test. Categorical variables are presented as number and as percentage. Participants were followed in time and assessed at 30 days after admission (~1 month). Measure of follow-up was set as person-days. Differences in eosinophil counts at admission between participants who survived and those with fatal outcome were formally assessed using the Kruskal Wallis (one way non-parametric analysis of variance) test. The same test was employed for formally comparing unadjusted mortality rates per subgroups.
Eosinophil count as a prognostic marker for all-cause mortality at 30 days of follow-up was assessed using receiver-operating characteristic (ROC) curve analyses. Cut-off values for eosinophil counts were determined for optimal sensitivity and specificity. Area under curve (AUC) values were reported, along with p values for ROC curves. Besides sensitivity and specificity, Youden index J was also reported as a summarized measure of test performance. ROC curve analysis was not performed for ACO patients due to the small number of observations.
Survival analysis was performed using Kaplan-Meier curves, as well as by employing Cox proportional hazards regression model, which allowed adjustments for sex, age and comorbidities as well as for inclusion of obstructive diseases and eosinophil count as variables (covariates). Model assumptions were tested using proportionality test. The model was created using the following parameters: “time to event” was time from admission to the 30th day census; “event” was fatal outcome. Covariances were participants’ age at admission, sex, Charlson comorbidity index, eosinophil count and obstructive disease (no known obstructing disease, asthma, COPD, ACO). Hazard ratios (HR) with 95% confidence intervals (95% CI) were reported, along with the accompanying slope, Wald statistic and p values. Even though COPD is one of the variables used for calculating the Charlson comorbidity index, it was employed as a joint measurement of comorbidity burden because of its longstanding validity in the previous literature in both COVID-19 and other clinical settings [35,36,37,38].
This manuscript was structured according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist and guidelines for reporting cohort studies in order to achieve the highest possible transparency [39]. For simplicity, the abbreviation ACO was used throughout this manuscript in order to denote concomitant asthma and COPD diagnoses (as mentioned above ACO is not a single disease entity). The severity of COVID-19 was assessed based on the World Health Organization recommendations (WHO) [40, 41].
Results
Out of N = 6083 registry entries, N = 5959 met the inclusion criteria, while N = 124 failed to meet them due to the fact that these entries did not represent first, but subsequent hospitalization(s) with SARS-CoV‑2 positivity. A total of N = 306 participants were excluded from the study because they did not have information regarding eosinophil count at admission. A flowchart representing the selection process is depicted in Fig. 1. A total of N = 5653 participants were included in this study, whose summarized characteristics are presented in Table 1. Of the cohort 43.8% were female and median age at admission was 72 (62–81) years. The majority of patients (87.4%) had severe or critical COVID-19 disease at admission, 85.3% required oxygen therapy at admission (Table 1), 78.5% of patients were treated with systemic corticosteroids during hospital stay. Details regarding corticosteroid treatment, as well as regards oral corticosteroid therapy (regardless of indications) prior to admission are presented in Table 1. Most participants (90.6%) had no known obstructive disease prior to hospital admission, 2.61% had a history of asthma and 6.58% a history of COPD. A total of N = 14 (0.25% of the analyzed cohort) had concomitant asthma and COPD in their medical documentation.
Fatal outcome at 30 days of follow-up was observed in 33.2% of the entire cohort. Fatal outcomes per subgroups (unadjusted for confounders) were as follows: 32.8% for participants without obstructive disease premorbidity; 28.6% for asthma subgroup; 35.7% for ACO subgroup and 41.7% for participants with COPD; χ2 = 5.7; p = 0.033; details presented in Table 1. Kaplan-Meier curve analyses for 30 days postadmission, for the entire cohort and for subgroups are presented in Fig. 2. Overall Cox proportional hazards regression model fit for 30-day mortality analysis was statistically significant (χ2 = 947.6; df = 7; p < 0.0001); survival probability curves from the plotted model are presented in Fig. 3. Covariates with respective hazard ratios are presented in Table 2. Asthma, COPD or ACO in comparison to the absence of obstructive disease were not significant covariates in the plotted model. Conversely, the plotted model indicated the protective effect of female sex (HR: 0.71, 95% CI: 0.65–0.79, p < 0.0001) and eosinophil count at admission (HR: 0.13, 95% CI: 0.06–0.29, p < 0.0001) on 30 days survival when analyzed for the entire cohort. Furthermore, higher Charlson’s comorbidity index (HR 1.04, 95% CI: 1.04–1.05; p < 0.0001) and age in years (HR: 1.11, 95% CI: 1.09–1.13, p < 0.0001) are implicated to have a harmful effect on participants’ survival at 30 days of follow-up.
Survival probability extrapolated from the plotted Cox proportional hazards regression model plotted for 30 days of follow-up. a Survival at mean of covariates; b survival for each subgroup. ACO concomitant asthma and chronic obstructive pulmonary disease; COPD chronic obstructive disease; NOD no obstructive disease
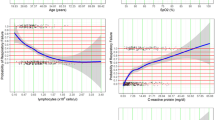
Median eosinophil count at admission for the entire cohort was 0.01 (0–0.03) × 109 cells per L. For participants who survived at 30 days of follow-up, eosinophil count was 0.01 (0–0.04) × 109 cells per L, whereas for those with fatal outcome, eosinophil count was 0 (0–0.02) × 109 cells per L (χ2 = 63.2; p < 0.000001). Data regarding eosinophil counts (expressed as cells/mm3) are presented in Table 3. ROC curve analysis was performed in order to assess the prognostic ability of eosinophil count at admission on all-cause mortality at 30 days of follow-up. AUC was 0.567. Optimal cut-off value was ≤ 0.02 × 109 cells per L (i.e. 20 cells per mm3) with a specificity of 80.8% and sensitivity of 30.6% for all-cause mortality at 30 days of follow-up. The analysis was statistically significant (p < 0.001). Results of ROC curve analyses for the entire cohort and additionally for asthma and COPD are presented in Table 4. ROC curve for the entire cohort is depicted in Fig. 4.
Discussion
Our retrospective registry-based study aimed to identify potential influence asthma, COPD and eosinophil count at admission might play on all-cause mortality. Cox proportional hazards regression model at 30 days of follow-up indicated that higher eosinophil count is associated with a reduction in all-cause mortality: HR 0.13 (95% CI: 0.06–0.29), mathematically suggesting that for an increase of 1000 eosinophils per mm3 (1 × 109 cells/L) in peripheral blood, an 87% mortality reduction would be observed. This finding goes in hand with the majority of previously published studies, which associated eosinopenia with worse outcomes [25, 27].
Furthermore, ROC curve analysis (p < 0.001), detailed in Table 4, revealed that low eosinophil counts at admission are prognostic markers of all-cause mortality which are fairly sensitive (~80–85%), but have low specificity (~25–30%); with low Youden J index, suggesting fairly poor test performance. Even though prognostic value was detected, test performance characteristics imply that eosinophil count at admission would probably not be a feasible test for mortality assessment. Results derived from our registry are comparable to those reported by Xuan et al. who investigated eosinophil count as a marker of ICU admission and mortality [42]. Besides SARS-CoV‑2, eosinopenia has previously been associated with respiratory syncytial virus and influenza A infections, but the causal relationship still remains unclear [27, 43,44,45]. Additionally, our research identified different cut-off eosinophil values for patients with asthma and COPD at 30 days of follow-up: Interestingly, the cut-off (with similar sensitivity and specificity) is lower for asthma (≤ 10 cells/mm3, p = 0.027) but higher for COPD (≤ 30 cells/mm3; p = 0.058, statistical significance not achieved), in comparison to the cut-off for the entire cohort (≤ 20 cells/mm3). Although robustly researched, the precise role eosinophils play in (acute) inflammation still remains largely uncovered [43, 44, 46, 47]. Novel evidence suggests that eosinophils promote acute inflammation resolution by blocking further tissue infiltration of polymorphonuclear leukocytes and by modulating macrophage phenotype to resolution phase macrophages [46, 48,49,50]. Moreover, eosinophils are well-recognized companions (and markers) of type 2 inflammation, in which type 2‑related cytokines are known to induce the chemotaxis and extravasation of eosinophils, with subsequent tissue infiltration [51]. In addition, during respiratory viral infections, an increased level of airway tissue eosinophilia has been noted [51]. Eosinophilic inflammation is most commonly associated with asthma, i.e. T2-high asthma phenotypes [2, 51, 52]; however, elements of eosinophilic inflammation have also been observed in COPD patients, and especially in those with concomitant asthma and COPD. Currently, peripheral eosinophilia guides escalation strategy of inhalation therapy in COPD patients in whom a tighter exacerbation control is indicated [5, 21, 24]. Eosinophils are likely a vitally important knot in a complex web connecting viral infections, atopy and chronic inflammation, resulting in clinical phenotypes recognized as different obstructive lung diseases.
Without correcting for age, sex and comorbidities, there was a statistically significant difference among research subgroups for all-cause mortality at 30 days of follow-up, the highest mortality observed in patients with COPD; however, after adjusting for these confounders, our regression model did not show that either pre-existing COPD, asthma or ACO has a significant impact on overall all-cause mortality at 30 days of follow-up. The discrepancy between preadjustment and postadjustment, at least in part, likely lies in the fact that patients with COPD are often burdened with other diseases, such as those affecting the cardiovascular system which have previously been linked with worse outcomes in patients with COVID-19 [53, 54]. Findings based on our model (suggesting that COPD, asthma or ACO do not significantly impact mortality) is in accordance with several large studies [55,56,57,58]; however, it is important to note that there are studies which have found a possible connection [59, 60].
It is also noteworthy to mention that based on our model, female sex seems to have a protective effect (HR: 0.71, 95% CI: 0.65–0.79), implicating a 29% risk reduction during the 30 days follow-up period. Conversely, increased age and comorbidities expressed as Charlston’s comorbidity index, had a harmful effect on all-cause mortality: HR of 1.04 (95% CI: 1.039–1.049) for age suggests a 4% all-cause mortality risk increase for every year of age; whereas HR of 1.12 (95% CI: 1.10–1.14) for Charlston’s comorbidity index denotes a 12% risk increase for each additional index point.
Another point that needs to be made is the relatively high mortality rate of 33.2% of patients at 30 days of follow-up. This is due to the fact that our tertiary hospital was designated as a primary respiratory center for COVID-19 for the entire region, which meant that it admitted patients in poor clinical condition who were referred from other smaller hospitals. This is also reflected in the fact that the majority of patients (87.4%) had severe or critical COVID-19 disease at admission to our hospital. Furthermore, the observed mortality is comparable to other tertiary centers [61, 62].
Our study has several limitations which should be accounted: our study is a retrospective (historical) cohort study by design and it is, therefore, susceptible to standard sources of bias inherent to retrospective cohorts. Selection bias is present due to the fact that our study did not distinguish between different indications for (or adverse events during) hospitalization and possible different patient management strategies. For example, the use of antiretroviral or systemic corticosteroid treatment was not included in the analysis. Additionally, as sequencing was not routinely performed on every sample, it is impossible to distinguish between different strains of SARS-CoV‑2. Moreover, vaccination status was not included in the registry. Furthermore, based on the retrospective data, it was impossible to stratify for COPD or asthma phenotype differences or their severity—namely, as these diseases were not the primary focus of the registry, their existence (or absence) was merely noted based on the prior medical documentation and patient history and asthma/COPD characteristics were not further investigated. In addition, our study solely investigated all-cause mortality and not specific causes of fatal outcomes. Furthermore, the use of oral corticosteroid treatment prior to hospital admission (available in Table 1) was not accounted for in this analysis. This was due to the fact that our main goal was to observe all-cause mortality and eosinophil trends in all patients (without exclusion for specific forms of treatment) because at the time of study design, we believed that given our retrospective data such interferences for specific pre-existing treatment might contribute to selection bias.
In spite of the above stated limitations, the strength of our study lies in the fact that it included consecutive patients from the beginning of the pandemic to mid-2021, resulting in a fairly large cohort of patients and it represents thus far the largest dataset covering Croatian population hospitalized with SARS-CoV‑2 infection.
Our results do not encourage the premise that obstructive lung disease may be important predictors of all-cause mortality at 30 days of follow-up; however, they indicate the potential prognostic role eosinophil count at admission might have on all-cause mortality. Notably, even though a prognostic role is detected, based on the test performance metrics employed, eosinophil count is not a promising biomarker for SARS-CoV‑2 survival assessment. Our results suggest potential presence of the underlying biological role eosinophils in the peripheral blood might play in SARS-CoV‑2 infection resolution, which should be further investigated. In future analyses, it would also be interesting to observe eosinophil count trends in SARS-CoV-2 patients after initialization of corticosteroid treatment.
It is important to take into account the abovementioned limitations when drawing conclusions from this study; therefore, further focused investigations (ideally prospective studies and further meta-analyses) are required to validate or dismiss our findings.
References
Drummond MB. Obstructive airway disease in urban populations. Curr Opin Pulm Med. 2014;20:180–5.
Global Initiative for Asthma. Global strategy for asthma management and prevention. 2022.
Loftus PA, Wise SK. Epidemiology and economic burden of asthma. Int Forum Allergy Rhinol. 2015;5:S7–S10. https://doi.org/10.1002/alr.21547.
Loftus PA, Wise SK. Epidemiology of asthma. Curr Opin Otolaryngol Head Neck Surg. 2016;24:245–9.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2022.
Bartal M. COPD and tobacco smoke. Monaldi Arch Chest Dis. 2005; https://doi.org/10.4081/monaldi.2005.623.
Carmona-Pírez J, Poblador-Plou B, Ioakeim-Skoufa I, et al. Multimorbidity clusters in patients with chronic obstructive airway diseases in the EpiChron Cohort. Sci Rep. 2021;11:4784.
Lindberg A, Lindberg L, Sawalha S, et al. Large underreporting of COPD as cause of death-results from a population-based cohort study. Respir Med. 2021;186:106518.
Quaderi SA, Hurst JR. The unmet global burden of COPD. Glob Health Epidemiol Genomics. 2018;3:e4.
Holland AE, Harrison SL, Brooks D. Multimorbidity, frailty and chronic obstructive pulmonary disease. Chron Respir Dis. 2016;13:372–82. https://doi.org/10.1177/1479972316670104.
Boulet L‑P, Hanania NA. The many faces of asthma-chronic obstructive pulmonary disease overlap. Curr Opin Pulm Med. 2019;25:1–10.
Mekov E, Nuñez A, Sin DD, et al. Update on Asthma–COPD Overlap (ACO): A narrative review. Int J Chron Obstruct Pulmon Dis. 2021;16:1783–99.
King Han M, Wenzel S. Asthma and COPD overlap (ACO). UpToDate. 2022. https://www.uptodate.com/contents/asthma-and-copd-overlap-aco. Accessed 22 Jan 2023.
Howell D, Verma H, Ho KS, et al. Asthma and COVID-19: lessons learned and questions that remain. Expert Rev Respir Med. 2021;15:1377–86. https://doi.org/10.1080/17476348.2021.1985763.
Schwartz J, Birnbaum B, Ballenberger M, et al. COVID-19 and obstructive lung disease: are COPD and asthma risk factors for severe COVID-19? Evaluating the data from the largest health system in New York State. In: Am. Thorac. Soc. Int. Conf. 2021. p. 2021. Abstract A1276.
Terry PD, Heidel RE, Dhand R. Asthma in adult patients with COVID-19. Prevalence and risk of severe disease. Am J Respir Crit Care Med. 2021;203:893–905. https://doi.org/10.1164/rccm.202008-3266OC.
Lacedonia D, Scioscia G, Santomasi C, et al. Impact of smoking, COPD and comorbidities on the mortality of COVID-19 patients. Sci Rep. 2021;11:19251.
Izquierdo JL, Almonacid C, González Y, et al. The impact of COVID-19 on patients with asthma. Eur Respir J. 2021;57:2003142. https://doi.org/10.1183/13993003.03142-2020.
Kumar V, Abbas AK, Fausto N, Robbins SL, RSC. Robbins and Cotran pathologic basis of disease. Philadelphia: Elsevier Saunders; 2005.
Kanuru S, Sapra A. Eosinophilia. StatPearls. 2021. https://www.ncbi.nlm.nih.gov/books/NBK560929/. Access date: May 1, 2022
Singh D, Kolsum U, Brightling CE, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44:1697–700. https://doi.org/10.1183/09031936.00162414.
Hartl S, Breyer-Kohansal R, Breyer MK, et al. Blood eosinophils and obstructive lung diseases—results from the population-based Austrian LEAD Study. Epidemiology. Eur Respir Soc. 2017; https://doi.org/10.1183/1393003.congress-2017.PA2631.
Annangi S, Nutalapati S, Sturgill J, et al. Eosinophilia and fractional exhaled nitric oxide levels in chronic obstructive lung disease. Thorax. 2022;77:351.
David B, Bafadhel M, Koenderman L, et al. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax. 2021;76:188–95. https://doi.org/10.1136/thoraxjnl-2020-215167.
Outh R, Boutin C, Gueudet P, et al. Eosinopenia <100/μL as a marker of active COVID-19: An observational prospective study. J Microbiol Immunol Infect. 2021;54:61–8.
Yan B, Yang J, Xie Y, et al. Relationship between blood eosinophil levels and COVID-19 mortality. World Allergy Organ J. 2021;14:100521.
Roca E, Ventura L, Zattra CM, et al. EOSINOPENIA: an early, effective and relevant COVID-19 biomarker? QJM. 2021;114:68–9.
Ferchichi M, Khalfallah I, Louhaichi S, et al. Eosinophils and COVID-19 prognosis. Mech lung Inj repair. Eur Respir Soc. 2021; https://doi.org/10.1183/13993003.congress-2021.PA3621.
Hirosawa T, Harada Y, Morinaga K, et al. Eosinopenia as a diagnostic marker of bloodstream infection in a general internal medicine setting: a cohort study. BMC Infect Dis. 2020;20:85. https://doi.org/10.1186/s12879-020-4814-5.
Partouche B, Pepin M, de Farcy PM, et al. Persistent eosinopenia is associated with in-hospital mortality among older patients: unexpected prognostic value of a revisited biomarker. BMC Geriatr. 2021;21:557. https://doi.org/10.1186/s12877-021-02515-0.
ClinicalTrials.gov. Registry of hospitalized patients in university hospital Dubrava respiratory center (COVID-19). https://clinicaltrials.gov/ct2/show/study/NCT05151094. Access date: May 1, 2022
Lucijanic M, Demaria M, Gnjidic J, et al. Higher ferritin levels in COVID-19 patients are associated with hyperinflammation, worse prognosis, and more bacterial infections without pronounced features of hemophagocytosis. Ann Hematol. 2022;101:1119–21. https://doi.org/10.1007/s00277-022-04813-y.
JAMOVI. The-jamovi-project. 2020. https://www.jamovi.org. Access date: May 1, 2022
MedCalc Software. MedCalc® Statistical software. 2022. https://www.medcalc.org. Access date: May 1, 2022
Comoglu S, Kant A. Does the Charlson comorbidity index help predict the risk of death in COVID-19 patients? North Clin Istanbul. 2022;9:117–21.
Charlson ME, Carrozzino D, Guidi J, et al. Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom. 2022;91:8–35.
Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51.
Ahmed J, Avendaño Capriles CA, Avendaño Capriles NM, et al. The impact of Charlson comorbidity index on mortality from SARS-CoV‑2 virus infection. Cureus. 2021;13:e19937.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Lucijanić M, Stojić J, Atić A, et al. Clinical and prognostic significance of C‑reactive protein to albumin ratio in hospitalized coronavirus disease 2019 (COVID-19) patients. Wien Klin Wochenschr. 2022;134:377–84. https://doi.org/10.1007/s00508-021-01999-5.
World Health Organization. Clinical management of COVID-19: interim guidance. 2020. https://apps.who.int/iris/handle/10665/332196. Access date: May 1, 2022
Xuan W, Jiang X, Huang L, et al. Predictive value of eosinophil count on COVID-19 disease progression and outcomes, a retrospective study of Leishenshan hospital in Wuhan, China. J Intensive Care Med. 2022;37:359–65. https://doi.org/10.1177/08850666211037326.
Klion AD, Ackerman SJ, Bochner BS. Contributions of Eosinophils to human health and disease. Annu Rev Pathol Mech Dis. 2020;15:179–209. https://doi.org/10.1146/annurev-pathmechdis-012419-032756.
Rosenberg HF, Dyer KD, Domachowske JB. Eosinophils and their interactions with respiratory virus pathogens. Immunol Res. 2009;43:128–37. https://doi.org/10.1007/s12026-008-8058-5.
Callaway Z, Kim CK. Respiratory viruses, Eosinophilia and their roles in childhood asthma. Int Arch Allergy Immunol. 2011;155:1–11.
Isobe Y, Kato T, Arita M. Emerging roles of eosinophils and eosinophil-derived lipid mediators in the resolution of inflammation. Front Immunol. 2012; https://doi.org/10.3389/fimmu.2012.00270.
Sampson AP. The role of eosinophils and neutrophils in inflammation. Clin Exp Allergy. 2000;30:22–7.
Yamada T, Tani Y, Nakanishi H, et al. Eosinophils promote resolution of acute peritonitis by producing proresolving mediators in mice. FASEB J. 2011;25:561–8. https://doi.org/10.1096/fj.10-170027.
Wu D, Molofsky AB, Liang H‑E, et al. Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science. 2011;332:243–7. https://doi.org/10.1126/science.1201475.
Tani Y, Isobe Y, Imoto Y, et al. Eosinophils control the resolution of inflammation and draining lymph node hypertrophy through the proresolving mediators and CXCL13 pathway in mice. FASEB J. 2014;28:4036–43. https://doi.org/10.1096/fj.14-251132.
Nagata M, Nakagome K, Soma T. Mechanisms of eosinophilic inflammation. Asia Pac Allergy. 2020;10:1–10.
Lugogo N, Que LG, Carr TF, et al. Asthma: diagnosis and management. In: Broaddus VC, editor. Murray Nadel’s Textb Respir Med. 7th ed. Vol. 1. 2021. pp. 831–49.
Decramer M, Janssens W. Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med. 2013;1:73–83.
Mishra P, Parveen R, Bajpai R, et al. Impact of cardiovascular diseases on severity of COVID-19 patients: A systematic review. Ann Acad Med Singapore. 2021;50:52–60.
Jeong JS, Kim JS, You YS, et al. COPD is a risk factor for COVID-19, but does not confer increased severity of the disease. Respir Med. 2021. https://doi.org/10.1016/j.rmed.2021.106640
Dolby T, Nafilyan V, Morgan A, et al. Relationship between asthma and severe COVID-19: a national cohort study. Thorax. 2022; https://doi.org/10.1136/thoraxjnl-2021-218629.
Sunjaya AP, Allida SM, Di Tanna GL, et al. Asthma and COVID-19 risk: a systematic review and meta-analysis. Eur Respir J. 2022;59:2101209.
Zhang J, Dong X, Liu G, et al. Risk and protective factors for COVID-19 morbidity , severity , and mortality. Clin Rev Allergy Immunol. 2022; https://doi.org/10.1007/s12016-022-08921-5.
Gerayeli FV, Milne S, Cheung C, et al. COPD and the risk of poor outcomes in COVID-19 : A systematic review and meta-analysis. EClinicalMedicine. 2021;33:100789. https://doi.org/10.1016/j.eclinm.2021.100789.
Soriano JB, Arroyo-espliguero R, Signes-costa J, et al. Prevalence and 30-day mortality in hospitalized patients with Covid-19 and prior lung. Diseases. 2021;57:13–20.
Culqui DR, Ortega Segura J, Da Costa-Venancio E, et al. Risk factors associated with the mortality of COVID-19 patients aged ≥60 years neither Intubated nor treated with mechanical ventilation: a multicentre retrospective cohort study during the first wave in Spain. BioMed. 2022;2:341–58.
Ferroni E, Giorgi Rossi P, Spila Alegiani S, et al. Survival of hospitalized COVID-19 patients in northern Italy: a population-based cohort study by the ITA-COVID-19 network. Clin Epidemiol. 2020;12:1337–46. https://doi.org/10.2147/CLEP.S271763.
Acknowledgements
This article is a part of the project “Registar hospitalno liječenih bolesnika u Respiracijskom centru Kliničke bolnice Dubrava (COVID-19)” (Registry of Hospitalized Patients in University Hospital Dubrava Respiratory Center (COVID-19)) (ClinicalTrials.gov Identifier: NCT05151094). We thank Nevenka Piskač-Živković for her contribution to the Registry. We thank all volunteers who contributed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G. Salai, H. Vrazic, I. Kovacevic, L.M. Janes, I. Marasovic, D. Ranilovic, D. Vukoja, M. Zelenika Margeta, I. Huljev–Sipos, K. Lalic, M. Spoljaric, J. Tekavec-Trkanjec, M. Vergles, M. Lucijanic, I. Luksic and D. Ljubicic declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salai, G., Vrazic, H., Kovacevic, I. et al. Investigating the role of obstructive pulmonary diseases and eosinophil count at admission on all-cause mortality in SARS-CoV-2 patients. Wien Klin Wochenschr 135, 235–243 (2023). https://doi.org/10.1007/s00508-023-02180-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-023-02180-w