Summary
Objectives
To investigate the prognostic significance of lymph node characteristics (total number of resected lymph nodes, metastatic lymph node ratio, and metastatic lymph nodes site) on survival in patients with esophageal squamous cell carcinoma.
Methods
Patients who underwent esophagectomy at Huashan Hospital, Fudan University, between October 1, 2003, and December 31, 2008, were reviewed. Survival data and clinicopathological characteristics were collected.
Results
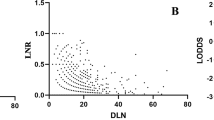
Among 205 patients, the median overall survival time was 48.0 months and the overall 5-year survival rate was 44.7 %. The independent risk factors for disease-free survival were the metastatic lymph node ratio (P < 0.001) and the number of positive lymph nodes (P < 0.001) and not the total number of resected lymph nodes (Χ 2 = 3.063, P = 0.216). There was no difference in survival between patients with extrathoracic and intrathoracic lymph node metastasis (Χ 2 = 0.295, P = 0.587). No significant relation was found between tumor location and the site of metastatic lymph nodes (rs = 0.125, P = 0.245).
Conclusions
Our finding revealed that the ratio and the number, but not the site, of metastatic lymph nodes were independent prognostic risk factors in esophageal squamous cell carcinomas. We suggest taking these factors into consideration for better estimation of prognosis.
Zusammenfassung
Ziel
Untersuchung der prognostischen Bedeutung der Lymphknoten-Charakteristika (Quotient der Gesamtzahl der resezierten Lymphknoten zu den metastasierten Lymphknoten, Lokalisation der Lymphknoten) auf das Überleben von Patienten mit einem Plattenepithelkarzinom des Ösophagus.
Methodik
Es wurden die Überlebensraten und klinisch-pathologischen Charakteristika von Patienten, die von 1.10.2003 bis 31.12.2008 am Huashan Spital der Fudan Universität ösophagektomiert wurden, gesammelt und ausgewertet.
Ergebnisse
Die mediane Gesamtüberlebenszeit der 205 Patientenbetrug 48 Monate. Die Gesamt 5-Jahre Überlebensrate lag bei 44,7 %. Die Gesamtzahl der resezierten Lymphknoten war kein unabhängiger Risikofaktor (Χ 2 = 3,063; P = 0,216). Unabhängige Risikofaktoren waren der Quotient der metastasierten Lymphknoten (P < 0,001) und die Zahl der positiven Lymphknoten (P < 0,001). Es bestand kein Unterschied in den Überlebensraten der Patienten mit intrathorakalen Lymphknotenmetastasen im Vergleich zu denen mit extrathorakalen Lymphknotenmetastasen (Χ 2 = 0,295; P = 0,587). Es wurde keine signifikante Korrelation zwischen der Tumorlokalisation und der Lokalisation der Lymphknotenmetastasen gefunden (rs = 0,125; P = 0,245).
Schlussfolgerungen
Unsere Ergebnisse zeigen, dass der Quotient und die Zahl, nicht aber die Lage der befallenen Lymphknoten unabhängige Risikofaktoren beim Plattenepithelkarzinom des Ösohagus sind. Wir empfehlen daher, diese Faktoren zur besseren Prognoseabschätzung in Erwägung zu ziehen.





Similar content being viewed by others
References
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24(14):2137–50.
Ajani JA, Barthel JS, Bentrem DJ, D’Amico TA, Das P, Denlinger CS, et al. Esophageal and esophagogastric junction cancers. J Natl Compr Canc Netw. 2011;9(8):830–87.
Edge SB. American Joint Committee on Cancer: AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Li B, Chen H, Xiang J, Zhang Y, Li C, Hu H, et al. Pattern of lymphatic spread in thoracic esophageal squamous cell carcinoma: a single-institution experience. J Thorac Cardiovasc Surg. 2012;144(4):778–86.
Tanaka H, Ohira M, Kubo N, Muguruma K, Yamashita Y, Sawada T, et al. Association of location of lymph node metastases with postoperative recurrence of esophageal squamous cell carcinoma. Anticancer Res. 2012;32(8):3421–6.
Shimada H, Okazumi S, Matsubara H, Nabeya Y, Shiratori T, Shimizu T, et al. Impact of the number and extent of positive lymph nodes in 200 patients with thoracic esophageal squamous cell carcinoma after three-field lymph node dissection. World J Surg. 2006;30(8):1441–9.
Shimada H, Okazumi S, Matsubara H, Nabeya Y, Shiratori T, Shuto K, et al. Location and clinical impact of solitary lymph node metastasis in patients with thoracic esophageal carcinoma. Am J Surg. 2006;192(3):306–10.
Kunisaki C, Makino H, Kimura J, Oshima T, Fujii S, Takagawa R, et al. Impact of lymph-node metastasis site in patients with thoracic esophageal cancer. J Surg Oncol. 2010;101(1):36–42.
Igaki H, Tachimori Y, Kato H. Improved survival for patients with upper and/or middle mediastinal lymph node metastasis of squamous cell carcinoma of the lower thoracic esophagus treated with 3-field dissection. Ann Surg. 2004;239(4):483–90.
Martin DJ, Church NG, Kennedy CW, Falk GL. Does systematic 2-field lymphadenectomy for esophageal malignancy offer a survival advantage? Results from 178 consecutive patients. Dis Esophagus. 2008;21(7):612–8.
Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg. 1998;175(1):47–51.
Baba Y, Watanabe M, Shigaki H, Iwagami S, Ishimoto T, Iwatsuki M, et al. Negative lymph-node count is associated with survival in patients with resected esophageal squamous cell carcinoma. Surgery. 2012. doi:10.1016/S0039-60 60(12) 00442-4.
Greenstein AJ, Litle VR, Swanson SJ, Divino CM, Packer S, Wisnivesky JP. Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer. Cancer. 2008;112(6):1239–46.
Peyre CG, Hagen JA, DeMeester SR, Altorki NK, Ancona E, Griffin SM, et al. The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. Ann Surg. 2008;248(4):549–56.
Hsu WH, Hsu PK, Hsieh CC, Huang CS, Wu YC. The metastatic lymph node number and ratio are independent prognostic factors in esophageal cancer. J Gastrointest Surg. 2009;13(11):1913–20.
Chao YK, Liu HP, Hsieh MJ, Wu YC, Liu YH, Yeh CH, et al. Impact of the number of lymph nodes sampled on outcome in ypT0N0 esophageal squamous cell carcinoma patients. J Surg Oncol. 2012;106(4):436–40.
Bogoevski D, Onken F, Koenig A, Kaifi JT, Schurr P, Sauter G, et al. Is it time for a new TNM classification in esophageal carcinoma? Ann Surg. 2008;247(4):633–41.
Groth SS, Virnig BA, Whitson BA, DeFor TE, Li ZZ, Tuttle TM, et al. Determination of the minimum number of lymph nodes to examine to maximize survival in patients with esophageal carcinoma: data from the Surveillance Epidemiology and End Results database. J Thorac Cardiovasc Surg. 2010;139(3):612–20.
Yang HX, Xu Y, Fu JH, Wang JY, Lin P, Rong TH. An evaluation of the number of lymph nodes examined and survival for node-negative esophageal carcinoma: data from China. Ann Surg Oncol. 2010;17(7):1901–11.
Liu YP, Ma L, Wang SJ, Chen YN, Wu GX, Han M, et al. Prognostic value of lymph node metastases and lymph node ratio in esophageal squamous cell carcinoma. Eur J Surg Oncol. 2010;36(2):155–9
Kelty CJ, Kennedy CW, Falk GL. Ratio of metastatic lymph nodes to total number of nodes resected is prognostic for survival in esophageal carcinoma. J Thorac Oncol. 2010;5(9):1467–71.
Wu J, Chen QX, Zhou XM, Mao WM, Krasna MJ, Teng LS. Prognostic significance of solitary lymph node metastasis in patients with squamous cell carcinoma of middlethoracic esophagus. World J Surg Oncol. 2012;10(1):210.
Kunisaki C, Makino H, Kimura J, Oshima T, Fujii S, Takagawa R, et al. Therapeutic strategy for esophageal cancer based on solitary lymph node metastasis. Hepatogastroenterology. 2011;58(110–111):1561–5.
Sakai M, Suzuki S, Sano A, Tanaka N, Inose T, Sohda M, et al. Significance of lymph node capsular invasion in esophageal squamous cell carcinoma. Ann Surg Oncol. 2012;19(6):1911–7.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, N., Chen, Z., Pang, L. et al. Prognostic significance of lymph node characteristics on survival in esophageal squamous cell carcinomas. Wien Klin Wochenschr 125, 26–33 (2013). https://doi.org/10.1007/s00508-012-0310-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0310-2