Abstract
Background
Acute post-streptococcal glomerulonephritis (APSGN) is an immune-mediated inflammatory respsonse in the kidneys caused by nephritogenic strains of group A β-hemolytic streptococcus (GAS). The present study aimed to present a large patient cohort of APSGN patients to determine the factors that can be used for predicting the prognosis and progression to rapidly progressive glomerulonephritis (RPGN).
Methods
The study included 153 children with APSGN that were seen between January 2010 and January 2022. Inclusion criteria were age 1–18 years and follow-up of ≥ 1 years. Patients with a diagnosis that could not be clearly proven clinically or via biopsy and with prior clinical or histological evidence of underlying kidney disease or chronic kidney disease (CKD) were excluded from the study.
Results
Mean age was 7.36 ± 2.92 years, and 30.7% of the group was female. Among the 153 patients, 19 (12.4%) progressed to RPGN. The complement factor 3 and albumin levels were significantly low in the patients who had RPGN (P = 0.019). Inflammatory parameters, such as C-reactive protein (CRP), platelet-to-lymphocyte ratio, CRP/albumin ratio, and the erythrocyte sedimentation rate level at presentation were significantly higher in the patients with RPGN (P < 0.05). Additionally, there was a significant correlation between nephrotic range proteinuria and the course of RPGN (P = 0.024).
Conclusions
We suggest the possibility that RPGN can be predicted in APSGN with clinical and laboratory findings.
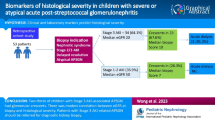
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Rodriguez-Iturbe B, Musser JM (2008) The current state of poststreptococcal glomerulonephritis. J Am Soc Nephrol 19:1855–1864
Rawla P, Padala SA, Ludhwani D (2022) Poststreptococcal Glomerulonephritis. In: StatPearls. StatPearls Publishing, Treasure Island, FL. https://www.ncbi.nlm.nih.gov/books/NBK538255/
Chugh KS, Malhotra HS, Sakhuja V, Bhusnurmath S, Singhal PC, Unni VN, Singh N, Pirzada R, Kapoor MM (1987) Progression to end stage kidney disease in post-streptococcal glomerulonephritis. Int J Artif Organs 10:189–194
Moorani KN, Aziz M, Amanullah F (2022) Rapidly progressive glomerulonephritis in children Pak. J Med Sci 38:417–425
Rodriguez-Iturbe B, Najafian B, Silva AE, Alpers C (2016) Acute postinfectious glomerulonephritis in children. In: Avner ED (ed) Pediatric Nephrology, 7th edn. Springer, London, pp 959–969
Marcdante KJ, Kleigman RM (2006) Nephrology and urology. In: Robert M (ed) Nelson Essentials of Pediatrics, 5th edn. Elsevier, Philadelphia, pp 751–770
Marshall CS, Cheng AC, Markey PG, Towers RJ, Richardson LJ, Fagan PK, Scott L, Krause VL, Currie BJ (2011) Acute poststreptococcal glomerulonephritis in the Northern Territory of Australia: a review of 16 years data and comparison with the literature. Am J Trop Med Hyg 85:703–710
Ong LT (2022) Management and outcomes of acute post-streptococcal glomerulonephritis in children World. J Nephrol 11:139–145
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady AB, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Becquet O, Pasche J, Gatti H, Chenel C, Abély M, Morville P, Pietrementet C (2010) Acute post-streptococcal glomerulonephritis in children of French Polynesia: a 3-year retrospective study. Pediatr Nephrol 25:275–280
Coulthard M, Isaacs D (1991) Retropharyngeal abscess. Arch Dis Child 66:1227–1230
Bingler MA, Ellis D, Moritz ML (2007) Acute post-streptococcal glomerulonephritis in a 14-month-old boy: Why is this uncommon? Pediatr Nephrol 22:448–450
Rodriguez-Iturbe B, Mezzano S (2009) Acute postinfectious glomerulonephritis. In: Avner E (ed) Pediatric Nephrology, 6th edn, Springer, Berlin and Heidelberg, pp 744–55
Eison TM, Ault BH, Jones DP, Chesney RW, Wyattet RJ (2011) Post-streptococcal acute glomerulonephritis in children: clinical features and pathogenesis. Pediatr Nephrol 26:165–180
Wong W, Lennon DR, Crone S, Neutze JM, Reed PW (2013) Prospective population-based study on the burden of disease from post-streptococcal glomerulonephritis of hospitalized children in New Zealand: Epidemiology, clinical features, and complications. J Paediatr Child Health 49:850–855
Roy S III, Stapleton FB (1990) Changing perspectives in children hospitalized with poststreptococcal acute glomerulonephritis. Pediatr Nephrol 4:585–588
Sanjad S, Tolaymat A, Whitworth J, Levin S (1977) Acute glomerulonephritis in children: A review of 153 cases. South Med J 70:1202–1206
Lewis EJ, Carpenter CB, Schur PH (1971) Serum complement component levels in human glomerulonephritis. Ann Intern Med 75:555–560
Cameron JS, Vick RM, Ogg CS, Seymour WM, Chantler C, Turner DR (1973) Plasma C3 and C4 Concentrations in Management of Glomerulonephritis. Br Med J 3:668–672
Wyatt RJ, Forristal J, West CD, Sugimoto S, Curd JG (1988) Complement profiles in acute post-streptococcal glomerulonephritis. Pediatr Nephrol 2:219–223
Ayoob RM, Schwaderer AL (2016) Acute Kidney Injury and Atypical Features during Pediatric Poststreptococcal Glomerulonephritis. Int J Nephrol 2016:5163065
Hart DH, Scheinkestel C, Whitworth JA, Kincaid-Smith P (1985) Acute post streptococcal glomerulonephritis without proteinuria. J R Soc Med 78:842–843
Bircan Z, Tugay S, Usluer H (2005) Poststreptococcal glomerulonephritis with pulmonary edema and microscopic hematuria. Pediatr Nephrol 20:1204
Wong W, Morris MC, Zwi J (2009) Outcome of severe acute post-streptococcal glomerulonephritis in New Zealand children. Pediatr Nephrol 24:1021–1026
Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S (2012) Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med 5:2
Makay B, AltugGucenmez O, Duman M, Unsal E (2014) The relationship of neutrophil-to-lymphocyte ratio with gastrointestinal bleeding in Henoch-Schonlein purpura. Rheumatol Int 34:1323–1327
Toraman A, Neşe N, Özyurt BC, Kürşat S (2019) Association between neutrophil-lymphocyte & platelet lymphocyte ratios with prognosis & mortality in rapidly progressive glomerulonephritis. Indian J Med Res 150:399
Kılıc BD, Kara MA, Buyukcelik M, Balat A (2018) Pediatric post-streptococcal glomerulonephritis: Clinical and laboratory data. Pediatr Int 60:645–650
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD (2019) The Platelet-to-Lymphocyte Ratio as an Inflammatory Marker in Rheumatic Diseases. Ann Lab Med 39:345–357
Fernandes B, Hamaguchi Y (2007) Automated enumeration of immature granulocytes. Am J Clin Pathol 128:454–463
Kim S, McClave SA, Martindale RG, Miller KR, Hurt RT (2017) Hypoalbuminemia and clinical outcomes: What is the mechanism behind the relationship? Am Surg 83:1220–1227
Stetson CA, Rammelkamp CH, Krause RM, Kohen RJ, Perry WD (1995) Epidemic acute nephritis: studies on etiology, natural history and prevention. Medicine 34:431–450
Lasch EE, Frankel V, Vardy PA, Rabinowitz SB, Ofek I, Rabinowitz K (1971) Epidemic glomerulonephritis in Israel. J Infect Dis 124:141–147
Bateman E, Mansour S, Okafor E, Arrington K, Hong BY, Cervantes J (2022) Examining the Efficacy of Antimicrobial Therapy in Preventing the Development of Postinfectious Glomerulonephritis: A Systematic Review and Meta-Analysis. Infect Dis Rep 14:176–183
Ahn SY, Ingulli E (2008) Acute poststreptococcal glomerulonephritis: an update. Curr Opin Pediatr 20:157–162
Kasahara T, Hayakawa H, Okubo S, Okugawa T, Kabuki N, Tomizawa S, Uchiyama M (2001) Prognosis of acute poststreptococcal glomerulonephritis is excellent in children, when adequately diagnosed. Pediatr Int 43:364–367
Sepahi MA, Shajari A, Shakiba M, Shooshtary FK, Salimi MH (2011) Acute Glomerulonephritis: A 7 Year Follow up of Children in Center of Iran. Acta Med Iran 49:375–378
Baikunje S, Vankalakunti M, Nikith A, Srivatsa A, Alva S, Kamath J (2016) Post-infectious glomerulonephritis with crescents in adults: a retrospective study. Clin Kidney J 9:222–226
Blyth CC, Robertson PW, Rosenberg AR (2007) Post-streptococcal glomerulonephritis in Sydney: A 16-year retrospective review. J Paediatr Child Health 43:446–450
Carapetis JR, Steer AC, Mulholland EK, Weber M (2005) The global burden of group A streptococcal diseases. Lancet Infect Dis 5:685–694
Kasiske BL, Wheeler DC (2012) Chapter 9: Infection-releated glomerulonephritis. Kidney Int Suppl 2:200–208
Acknowledgements
The authors gratefully acknowledge Mr. Scott Evans for English language editing.
Author information
Authors and Affiliations
Contributions
Study concept and design: Deniz Karakaya, Evrim Kargın Çakıcı, and Mehmet Bülbül. Analysis and interpretation of data: Deniz Karakaya, Tülin Güngör, Fatma Yazılıtaş, and Sait Can Yücebaş. Drafting of the manuscript: Deniz Karakaya, Tülin Güngör, and Evra Çelikkaya. Critical revision of the manuscript for important intellectual content: Deniz Karakaya and Evrim Kargın Çakıcı.
Corresponding author
Ethics declarations
We confirm that this work is original and has not been published elsewhere, nor is it currently under consideration for publication elsewhere. All authors accept the copyright of the journal.
Ethics approval
The study protocol was approved by the Dr. Sami Ulus Training and Research Hospital Ethics Committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karakaya, D., Güngör, T., Çakıcı, E.K. et al. Predictors of rapidly progressive glomerulonephritis in acute poststreptococcal glomerulonephritis. Pediatr Nephrol 38, 3027–3033 (2023). https://doi.org/10.1007/s00467-023-05935-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05935-9