Abstract
Background
There are similarities in hemodialysis (HD) between adults and children and also unique pediatric aspects. In this systematic review, we evaluated the existing HD literature, including vascular access, indications, parameters, and outcomes as a reflection on real-life HD practices.
Methods
Medline, Embase, CINAHL, Web of Science, and Cochrane Library were systematically searched for literature on HD in children (1–20 years). Two reviewers independently assessed the literature and data on indications; vascular access, outcomes, and specific parameters for HD were extracted.
Results
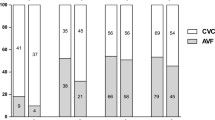
Fifty-four studies (8751 patients) were included in this review. Studies were stratified into age groups 1–5, 6–12, and 13–20 years based on median/mean age reported in the study, as well as era of publication (1990–2000, 2001–2010, and 2011–2019). Across all age groups, both arteriovenous fistulas and central venous catheters were utilized for vascular access. Congenital abnormalities and glomerulopathy were the most common HD indications. HD parameters including HD session duration, dialysate and blood flow rates, urea reduction ratio, and ultrafiltration were characterized for each age group, as well as common complications including catheter dysfunction and intradialytic hypotension. Median mortality rates were 23.3% (3.3), 7.6% (14.5), and 2.0% (3.0) in ages 1–5, 6–12, and 13–20 years, respectively. Median transplantation rates were 41.6% (38.3), 52.0% (32.0), and 21% (25.6) in ages 1–5, 6–12, and 13–20, respectively.
Conclusion
This comprehensive systematic review summarizes available literature on HD in children and young adults, including best vascular access, indications, technical aspects, and outcomes, and reflects on HD practices over the last three decades.


Similar content being viewed by others
Data availability
All data involved in this systematic review can be found within the article and/or in online supplementary material.
References
Müller D, Goldstein SL (2011) Hemodialysis in children with end-stage renal disease. Nat Rev Nephrol 7:650–658. https://doi.org/10.1038/nrneph.2011.124
Fischbach M, Edefonti A, Schröder C, Watson A (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066. https://doi.org/10.1007/s00467-005-1876-y
Walters S, Porter C, Brophy PD (2009) Dialysis and pediatric acute kidney injury: choice of renal support modality. Pediatr Nephrol 24:37–48. https://doi.org/10.1007/s00467-008-0826-x
Kovalski Y, Cleper R, Krause I, Davidovits M (2007) Hemodialysis in children weighing less than 15 kg: a single-center experience. Pediatr Nephrol 22:2105–2110. https://doi.org/10.1007/s00467-007-0614-z
Youssef DM, Neemat-Allah MAA (2013) Hemodialysis in children: eleven years in a single center in Egypt. Iran J Kidney Dis 7:468–474
Kurien R, George J, Jacob CK, Shastry J (1996) Vascular access in pediatric hemodialysis. Indian Pediatr 33:767–770
Fischbach M, Terzic J, Cohen CB, Cousandier E, Hamel G, Battouche D, Geisert J (1998) Glucose-charged dialysate for children on hemodialysis: acute dialytic changes. Pediatr Nephrol 12:60–62. https://doi.org/10.1007/s004670050404
Hari P, Kanitkar M, Mantan M, Bagga A (2002) Hemodialysis in children. Indian Pediatr 39:375–380
Peynircioglu B, Ozkan F, Canyigit M, Pamuk GA, Geyik S, Cil BE, Balkanci F (2007) Radiologically placed tunneled internal jugular catheters in the management of chronic hemodialysis and long-term infusion therapies in the pediatric population. J Vasc Interv Radiol 18:875–881. https://doi.org/10.1016/j.jvir.2007.04.016
Hothi DK, Harvey E, Goia CM, Geary DF (2008) Evaluating methods for improving ultrafiltration in pediatric hemodialysis. Pediatr Nephrol 23:631–638. https://doi.org/10.1007/s00467-007-0716-7
Hothi DK, Harvey E, Goia CM, Geary D (2009) The value of sequential dialysis, mannitol and midodrine in managing children prone to dialysis failure. Pediatr Nephrol 24:1587–1591. https://doi.org/10.1007/s00467-009-1151-8
Ma A, Shroff R, Hothi D, Lopez MM, Veligratli F, Calder F, Rees L (2013) A comparison of arteriovenous fistulas and central venous lines for long-term chronic haemodialysis. Pediatr Nephrol 28:321–326. https://doi.org/10.1007/s00467-012-2318-2
Shin HS, Oh JY, Park SJ, Kim JH, Lee JS, Shin J II (2015) Outcomes of hemodialysis in children: a 35-year experience at Severance Hospital. Yonsei Med J 56:1007–1014. https://doi.org/10.3349/ymj.2015.56.4.1007
Lutkin M, Stronach L, Yadav P, Hothi DK (2018) Dalteparin anticoagulation in paediatric home haemodialysis. Pediatr Nephrol 33:2337–2341. https://doi.org/10.1007/s00467-018-4032-1
Marsenić OD, Pavličić D, Peco-Antić A, Bigović G, Jovanović O (2000) Prediction of equilibrated urea in children on chronic hemodialysis. ASAIO J 46:283–287. https://doi.org/10.1097/00002480-200005000-00008
Kreuzer M, Bonzel K-E, Büscher R, Offner G, Ehrich JHH, Pape L (2010) Regional citrate anticoagulation is safe in intermittent high-flux haemodialysis treatment of children and adolescents with an increased risk of bleeding. Nephrol Dial Transplant 25:3337–3342. https://doi.org/10.1093/ndt/gfq225
Hoppe A, Von Puttkamer C, Linke U, Kahler C, Booß M, Braunauer-Kolberg R, Hofmann K, Joachimsky P, Hirte I, Schley S, Utsch B, Thumfart J, Briese S, Gellermann J, Zimmering M, Querfeld U, Müller D (2011) A hospital-based intermittent nocturnal hemodialysis program for children and adolescents. J Pediatr 158:64–68. e1. https://doi.org/10.1016/j.jpeds.2010.06.036
Rus RR, Novljan G, Buturović-Ponikvar J, Kovač J, Premru V, Ponikvar R (2011) Vascular access in children on chronic hemodialysis: a Slovenian experience. Ther Apher Dial 15:292–297. https://doi.org/10.1111/j.1744-9987.2011.00954.x
Marsenic O, Anderson M, Couloures KG, Hong WS, Kevin Hall E, Dahl N (2016) Effect of the decrease in dialysate sodium in pediatric patients on chronic hemodialysis. Hemodial Int 20:277–285. https://doi.org/10.1111/hdi.12384
Laskin BL, Huang G, King E, Geary DF, Licht C, Metlay JP, Furth SL, Kimball T, Mitsnefes M (2017) Short, frequent, 5-days-per-week, in-center hemodialysis versus 3-days-per week treatment: a randomized crossover pilot trial through the Midwest Pediatric Nephrology Consortium. Pediatr Nephrol 32:1423–1432. https://doi.org/10.1007/s00467-017-3656-x
Boehm M, Bonthuis M, Noordzij M, Harambat J, Groothoff JW, Melgar ÁA, Buturovic J, Dusunsel R, Fila M, Jander A, Koster-Kamphuis L, Novljan G, Ortega PJ, Paglialonga F, Saravo MT, Stefanidis CJ, Aufricht C, Jager KJ, Schaefer F (2019) Hemodialysis vascular access and subsequent transplantation: a report from the ESPN/ERA-EDTA Registry. Pediatr Nephrol 34:713–721. https://doi.org/10.1007/s00467-018-4129-6
Smyet SW, Evans JHC, Will E, Brocklebank JT (1992) Paediatric haemodialysis: estimation of treatment efficiency in the presence of urea rebound. Clin Phys Physiol Meas 13:51–62. https://doi.org/10.1088/0143-0815/13/1/005
Muñoz ET, Moreno CX (2000) Management of temporary haemodialysis catheters in paediatrics. EDTNA-ERCA J 26:16–18. https://doi.org/10.1111/j.1755-6686.2000.tb00085.x
Chand DH, Brier M, Strife CF (2005) Comparison of vascular access type in pediatric hemodialysis patients with respect to urea clearance, anemia management, and serum albumin concentration. Am J Kidney Dis 45:303–308. https://doi.org/10.1053/j.ajkd.2004.10.017
Feinstein S, Rinat C, Becker-Cohen R, Ben-Shalom E, Schwartz SB, Frishberg Y (2007) The outcome of chronic dialysis in infants and toddlers - advantages and drawbacks of haemodialysis. Nephrol Dial Transplant 23:1336–1345. https://doi.org/10.1093/ndt/gfm734
Gotta V, Marsenic O, Pfister M (2018) Age- and weight-based differences in haemodialysis prescription and delivery in children, adolescents and young adults. Nephrol Dial Transplant 33:1649–1660. https://doi.org/10.1111/hdi.12589
Shroff R, Smith C, Ranchin B, Bayazit AK, Stefanidis CJ, Askiti V, Azukaitis K, Canpolat N, Ağbaş A, Aitkenhead H, Anarat A, Aoun B, Aofolaju D, Bakkaloglu SA, Bhowruth D, Borzych-Dużałka D, Bulut IK, Büscher R, Deanfield J, Dempster C, Duzova A, Habbig S, Hayes W, Hegde S, Krid S, Licht C, Litwin M, Mayes M, Mir S, Nemec R, Obrycki L, Paglialonga F, Picca S, Samaille C, Shenoy M, Sinha MD, Spasojevic B, Stronach L, Vidal E, Vondrák K, Yilmaz A, Zaloszyc A, Fischbach M, Schmitt CP, Schaefer F (2019) Effects of hemodiafiltration versus conventional hemodialysis in children with ESKD: the HDF, heart and height study. J Am Soc Nephrol 30:678–691. https://doi.org/10.1681/asn.2018100990
Raina R, Vijayaraghavan P, Kapur G, Sethi SK, Krishnappa V, Kumar D, Bunchman TE, Bolen SD, Chand D (2018) Hemodialysis in neonates and infants: a systematic review. Semin Dial 31:289–299. https://doi.org/10.1111/sdi.12657
Müller D, Zimmering M, Chan CT, McFarlane PA, Pierratos A, Querfeld U (2008) Intensified hemodialysis regimens: neglected treatment options for children and adolescents. Pediatr Nephrol 23:1729–1736. https://doi.org/10.1007/s00467-008-0783-4
Fischbach M, Fothergill H, Zaloszyc A, Menouer S, Terzic J (2011) Intensified daily dialysis: the best chronic dialysis option for children? Semin Dial 24:640–644. https://doi.org/10.1111/j.1525-139X.2011.01020.x
Chand DH, Swartz S, Tuchman S, Valentini RP, Somers MJG (2017) Dialysis in children and adolescents: the pediatric nephrology perspective. Am J Kidney Dis 69:278–286. https://doi.org/10.1053/j.ajkd.2016.09.023
US Renal Data System (2018) 2018 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD
US Renal Data System (2019) US renal data system 2019 annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD
North American Pediatric Renal Trials and Collaborative Studies (2011) NAPRTCS 2011 annual dialysis report. In: North Am. Pediatr. Ren. Trials Collab. Stud. https://naprtcs.org/system/files/2011_Annual_Dialysis_Report.pdf
McTaggart S, Kennedy S, McDonald S, Henning P, Dent H (2009) Paediatric report - ANZDATA Registry 2009 report. Australia and New Zealand Dialysis and Transplant Registry, Adelaide, South Australia
ERA-EDTA Registry (2010) ERA-EDTA registry annual report 2008. Academic Medical Center, Department of Medical Informatics, Amsterdam, The Netherlands
Plumb L, Casula A, Pyart R, Evans KM, Inward C, Medcalf J, Marks SD (2020) The 21st UK Renal Registry annual report: a summary of analyses of paediatric data in 2017. Nephron 144:67–71. https://doi.org/10.1159/000504852
Ardissino G, Daccò V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, Marra G, Edefonti A, Sereni F (2003) Epidemiology of chronic renal failure in children: data from the ItalKid project. Pediatrics 111:e382–e387. https://doi.org/10.1542/peds.111.4.e382
Mong Hiep TT, Ismaili K, Collart F, Van Damme-Lombaerts R, Godefroid N, Ghuysen MS, Van Hoeck K, Raes A, Janssen F, Robert A (2010) Clinical characteristics and outcomes of children with stage 3-5 chronic kidney disease. Pediatr Nephrol 25:935–940. https://doi.org/10.1007/s00467-009-1424-2
Chanchlani R, Nash DM, McArthur E, Zappitelli M, Archer V, Kuwornu JP, Garg AX, Greenberg JH, Goldstein SL, Thabane L, Wald R (2019) Secular trends in incidence, modality, and mortality with dialysis receiving AKI in children in Ontario a population-based cohort study. Clin J Am Soc Nephrol 14:1288–1296. https://doi.org/10.2215/CJN.08250718
Chand DH, Valentini RP (2008) International pediatric fistula first initiative: a call to action. Am J Kidney Dis 51:1016–1024. https://doi.org/10.1053/j.ajkd.2008.02.309
Guzzo I, de Galasso L, Mir S, Bulut IK, Jankauskiene A, Burokiene V, Cvetkovic M, Kostic M, Bayazit AK, Yildizdas D, Schmitt CP, Paglialonga F, Montini G, Yilmaz E, Oh J, Weber L, Taylan C, Hayes W, Shroff R, Vidal E, Murer L, Mencarelli F, Pasini A, Teixeira A, Afonso AC, Drozdz D, Schaefer F, Picca S (2019) Acute dialysis in children: results of a European survey. J Nephrol 32:445–451. https://doi.org/10.1007/s40620-019-00606-1
Palmer S, Rabindranath K, Craig J, Roderick P, Locatelli F, Strippoli G (2012) High-flux versus low-flux haemodialysis membranes for end-stage kidney disease. Cochrane Database Syst Rev:1–102. https://doi.org/10.1002/14651858.CD005016.pub2
Raina R, Krishnappa V (2019) Hemodialysis treatment prescription. In: Critical care pediatric nephrology and dialysis: a practical handbook. Springer, Singapore, pp 95–106
Sethi SK, Bunchman T, Raina R, Kher V (2014) Unique considerations in renal replacement therapy in children: core curriculum 2014. Am J Kidney Dis 63:329–345. https://doi.org/10.1053/j.ajkd.2013.08.018
Basile C, Rossi L, Lomonte C (2016) The choice of dialysate bicarbonate: do different concentrations make a difference? Kidney Int 89:1008–1015. https://doi.org/10.1016/j.kint.2016.01.010
Hayes W, Hothi DK (2011) Intradialytic hypotension. Pediatr Nephrol 26:867–879. https://doi.org/10.1007/s00467-010-1661-4
Mustafa RA, Bdair F, Akl EA, Garg AX, Thiessen-Philbrook H, Salameh H, Kisra S, Nesrallah G, Al-Jaishi A, Patel P, Patel P, Mustafa AA, Schünemann HJ (2016) Effect of lowering the dialysate temperature in chronic hemodialysis: a systematic review and meta-analysis. Clin J Am Soc Nephrol 11:442–457. https://doi.org/10.2215/CJN.04580415
National Kidney Foundation (2006) KDOQI clinical practice guidelines and clinical practice recommendations for 2006 updates: hemodialysis adequacy, peritoneal dialysis adequacy and vascular access. Am J Kidney Dis 48(suppl 1):S1–S322. https://doi.org/10.1053/j.ajkd.2006.04.040
Gabutti L, Salvadé I, Lucchini B, Soldini D, Burnier M (2011) Haemodynamic consequences of changing potassium concentrations in haemodialysis fluids. BMC Nephrol 12:14. https://doi.org/10.1186/1471-2369-12-14
Acknowledgments
Work of CY was supported by the Michael G. DeGroote School of Medicine–McMaster Medical Student Research Excellence Awards.
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript and approved the final version. S. Sanger performed database search; C. Y. and A. F. independently reviewed literature and completed data extraction with assistance from R. Chanchlani. C.Y. and A.F. drafted the initial manuscript; A. T. completed statistical analysis and figure preparation. R. R., R. Chanchlani, R. Chakraborty, S. Sethi, and A. T. provided data interpretation and analysis, figure preparations, manuscript revisions, and critical feedback.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 381 kb)
Rights and permissions
About this article
Cite this article
Chanchlani, R., Young, C., Farooq, A. et al. Evolution and change in paradigm of hemodialysis in children: a systematic review. Pediatr Nephrol 36, 1255–1271 (2021). https://doi.org/10.1007/s00467-020-04821-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04821-y