Abstract
Background
While some studies have reported improvement in gastro-esophageal reflux disease (GERD) symptoms after sleeve gastrectomy (SG), others have reported higher incidence of de-novo GERD, worsening of prior GERD symptoms and erosive esophagitis post SG. Furthermore, GERD unresponsive to medical management is one of the most common indications for conversion of SG to Roux-en-Y gastric bypass (RYGB). Real-world data on safety of primary SG, primary RYGB and SG to RYGB conversion for obese patients with GERD would be helpful for informing surgeons and patient procedure selection. We sought to evaluate the trends in utilization and safety of primary RYGB and primary SG for patients with GERD requiring medications, and compare the peri-operative outcomes between primary RYGB and conversion surgery from SG to RYGB for GERD using the MBSAQIP database.
Methods
A comparative analysis of post-operative outcomes within 30 days was performed for primary RYGB and primary SG after 1:1 nearest neighbor propensity score matching for patient demographics and preoperative comorbidities using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) registry from 2015 to 2021. This was followed by comparison of peri-operative outcomes between conversion surgery from SG to RYGB for GERD and primary RYGB using MBSAQIP 2020–2021 data.
Results
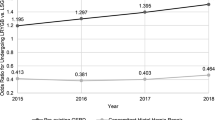
Utilization of primary RYGB increased from 38% in 2015 to 45% in 2021, while primary SG decreased from 62% in 2015 to 55% in 2021 for bariatric patients with GERD. Post-operative outcomes including reoperation, reintervention, readmission, major complications, and death within 30 days were significantly higher for patients undergoing primary RYGB compared to primary SG. Increased readmissions and ED visits were seen with conversion surgery. However, there was no difference in rates of reoperation, reintervention, major complications, or death between primary RYGB and SG conversion to RYGB cohorts.
Conclusions
This data suggests that a strategy of performing a primary SG and subsequent SG-RYGB conversion for those with recalcitrant GERD symptoms is not riskier than a primary RYGB. Thus, it may be reasonable to perform SG in patients who are well informed of the risk of worsening GERD requiring additional surgical interventions. However, the impact of such staged approach (SG followed by conversion to RYGB) on long-term outcomes remains unknown.
Graphical abstract



Similar content being viewed by others
References
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J (2003) Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA 290(1):66–72. https://doi.org/10.1001/jama.290.1.66
Nocon M, Labenz J, Willich SN (2006) Lifestyle factors and symptoms of gastro-oesophageal reflux—a population-based study. Aliment Pharmacol Ther 23(1):169–174. https://doi.org/10.1111/j.1365-2036.2006.02727.x
El-Hadi M, Birch DW, Gill RS, Karmali S (2014) The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg 57(2):139–144. https://doi.org/10.1503/cjs.030612
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832. https://doi.org/10.1007/s11695-015-1657-z
Frezza EE, Ikramuddin S, Gourash W et al (2002) Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 16(7):1027–1031. https://doi.org/10.1007/s00464-001-8313-5
Perry Y, Courcoulas AP, Fernando HC, Buenaventura PO, McCaughan JS, Luketich JD (2004) Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS 8(1):19–23
Peterli R, Borbély Y, Kern B et al (2013) Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg 258(5):690–694; discussion 695. https://doi.org/10.1097/SLA.0b013e3182a67426
Ashrafi D, Osland E, Memon MA (2020) Bariatric surgery and gastroesophageal reflux disease. Ann Transl Med 8(Suppl 1):S11. https://doi.org/10.21037/atm.2019.09.15
Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L (2020) Changes in utilization of bariatric surgery in the United States from 1993 to 2016. Ann Surg 271(2):201–209. https://doi.org/10.1097/SLA.0000000000003554
Weiner RA, Weiner S, Pomhoff I, Jacobi C, Makarewicz W, Weigand G (2007) Laparoscopic sleeve gastrectomy—influence of sleeve size and resected gastric volume. Obes Surg 17(10):1297–1305. https://doi.org/10.1007/s11695-007-9232-x
Moon Han S, Kim WW, Oh JH (2005) Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg 15(10):1469–1475. https://doi.org/10.1381/096089205774859227
Cottam D, Qureshi FG, Mattar SG et al (2006) Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc 20(6):859–863. https://doi.org/10.1007/s00464-005-0134-5
Howard DD, Caban AM, Cendan JC, Ben-David K (2011) Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis 7(6):709–713. https://doi.org/10.1016/j.soard.2011.08.003
Lakdawala MA, Bhasker A, Mulchandani D, Goel S, Jain S (2010) Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg 20(1):1–6. https://doi.org/10.1007/s11695-009-9981-9
Genco A, Soricelli E, Casella G et al (2017) Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis 13(4):568–574. https://doi.org/10.1016/j.soard.2016.11.029
Salminen P, Grönroos S, Helmiö M et al (2022) Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg 157(8):656–666. https://doi.org/10.1001/jamasurg.2022.2229
Parmar CD, Mahawar KK, Boyle M, Schroeder N, Balupuri S, Small PK (2017) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass is effective for gastro-oesophageal reflux disease but not for further weight loss. Obes Surg 27(7):1651–1658. https://doi.org/10.1007/s11695-017-2542-8
Clapp B, Wynn M, Martyn C, Foster C, O’Dell M, Tyroch A (2018) Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis 14(6):741–747. https://doi.org/10.1016/j.soard.2018.02.027
Rawlins L, Rawlins MP, Brown CC, Schumacher DL (2013) Sleeve gastrectomy: 5-year outcomes of a single institution. Surg Obes Relat Dis 9(1):21–25. https://doi.org/10.1016/j.soard.2012.08.014
Casella G, Soricelli E, Giannotti D et al (2016) Long-term results after laparoscopic sleeve gastrectomy in a large monocentric series. Surg Obes Relat Dis 12(4):757–762. https://doi.org/10.1016/j.soard.2015.09.028
Ali M, El Chaar M, Ghiassi S, Rogers AM, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2017) American Society for Metabolic and Bariatric Surgery updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis 13(10):1652–1657. https://doi.org/10.1016/j.soard.2017.08.007
Dang JT, Vaughan T, Mocanu V et al (2023) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: indications, prevalence, and safety. Obes Surg 33(5):1486–1493. https://doi.org/10.1007/s11695-023-06546-x
Strauss AL, Triggs JR, Tewksbury CM et al (2023) Conversion to Roux-en-Y gastric bypass: a successful means of mitigating reflux after laparoscopic sleeve gastrectomy. Surg Endosc. https://doi.org/10.1007/s00464-023-10024-x
Castagneto-Gissey L, Gualtieri L, Diddoro A, Genco A, Casella G (2023) Conversion from sleeve gastrectomy to Roux-en-Y gastric bypass for refractory GERD and Barrett’s esophagus. J Gastrointest Surg. https://doi.org/10.1007/s11605-023-05678-w
Kermansaravi M, Parmar C, Chiappetta S et al (2023) Best practice approach for redo-surgeries after sleeve gastrectomy, an expert’s modified Delphi consensus. Surg Endosc 37(3):1617–1628. https://doi.org/10.1007/s00464-023-09879-x
R Core Team (2021) R: a language and environment for statistical computing. https://www.R-project.org/
Peterli R, Wölnerhanssen BK, Peters T et al (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA 319(3):255–265. https://doi.org/10.1001/jama.2017.20897
Daes J, Jimenez ME, Said N, Daza JC, Dennis R (2012) Laparoscopic sleeve gastrectomy: symptoms of gastroesophageal reflux can be reduced by changes in surgical technique. Obes Surg 22(12):1874–1879. https://doi.org/10.1007/s11695-012-0746-5
Vanetta C, Dreifuss NH, Schlottmann F, Baz C, Masrur MA (2022) Bariatric surgery conversions in MBSAQIP centers: current indications and outcomes. Obes Surg 32(10):3248–3256. https://doi.org/10.1007/s11695-022-06229-z
Chiappetta S, Lainas P, Kassir R, Valizadeh R, Bosco A, Kermansaravi M (2022) Gastroesophageal reflux disease as an indication of revisional bariatric surgery-indication and results—a systematic review and metanalysis. Obes Surg 32(9):3156–3171. https://doi.org/10.1007/s11695-022-06183-w
Anderson B, Zhan T, Swaszek L et al (2023) Increased incidence of marginal ulceration following conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: a multi-institutional experience. Surg Endosc 37(5):3974–3981. https://doi.org/10.1007/s00464-022-09430-4
Guzman-Pruneda FA, Brethauer SA (2021) Gastroesophageal reflux after sleeve gastrectomy. J Gastrointest Surg 25(2):542–550. https://doi.org/10.1007/s11605-020-04786-1
Acknowledgements
None applicable.
Funding
None to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Tina Bharani, Ali Tavakkoli, Thomas Tsai, David Spector, Talar Tatarian, Malcolm Robinson and Eric Sheu have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bharani, T., Tavakkoli, A., Tsai, T. et al. National trends in utilization and safety of gastric bypass, sleeve gastrectomy and conversion surgery in patients with GERD. Surg Endosc 38, 1249–1256 (2024). https://doi.org/10.1007/s00464-023-10622-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10622-9