Abstract
Background
Surgical video recording provides the opportunity to acquire intraoperative data that can subsequently be used for a variety of quality improvement, research, and educational applications. Various recording devices are available for standard operating room camera systems. Some allow for collateral data acquisition including activities of the OR staff, kinematic measurements (motion of surgical instruments), and recording of the endoscopic video streams. Additional analysis through computer vision (CV), which allows software to understand and perform predictive tasks on images, can allow for automatic phase segmentation, instrument tracking, and derivative performance-geared metrics. With this survey, we summarize available surgical video acquisition technologies and associated performance analysis platforms.
Methods
In an effort promoted by the SAGES Artificial Intelligence Task Force, we surveyed the available video recording technology companies. Of thirteen companies approached, nine were interviewed, each over an hour-long video conference. A standard set of 17 questions was administered. Questions spanned from data acquisition capacity, quality, and synchronization of video with other data, availability of analytic tools, privacy, and access.
Results
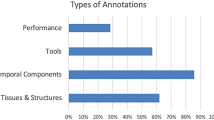
Most platforms (89%) store video in full-HD (1080p) resolution at a frame rate of 30 fps. Most (67%) of available platforms store data in a Cloud-based databank as opposed to institutional hard drives. CV powered analysis is featured in some platforms: phase segmentation in 44% platforms, out of body blurring or tool tracking in 33%, and suture time in 11%. Kinematic data are provided by 22% and perfusion imaging in one device.
Conclusion
Video acquisition platforms on the market allow for in depth performance analysis through manual and automated review. Most of these devices will be integrated in upcoming robotic surgical platforms. Platform analytic supplementation, including CV, may allow for more refined performance analysis to surgeons and trainees. Most current AI features are related to phase segmentation, instrument tracking, and video blurring.

Similar content being viewed by others
References
Spaner SJ, Warnock GL (1997) A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech 7:369–373
LaRose D, Taylor RH, Funda J, Eldridge B, Gomory S, Talamini MA, Kavoussi L, Anderson J, Gruben K (1995) A telerobotic assistant for laparoscopic surgery. IEEE Engin in Med and Biol Mag 14:279–288. https://doi.org/10.1109/51.391776
Talamini MA (2001) Surgery of the 21st century. Ann Surg 234:8–9
Filicori F, Addison P (2021) Intellectual property and data ownership in the age of video recording in the operating room. Surg Endosc. https://doi.org/10.1007/s00464-021-08692-8
Hashimoto DA, Rosman G, Witkowski ER, Stafford C, Navarette-Welton AJ, Rattner DW, Lillemoe KD, Rus DL, Meireles OR (2019) Computer vision analysis of intraoperative video: automated recognition of operative steps in laparoscopic sleeve gastrectomy. Ann Surg 270:414–421. https://doi.org/10.1097/SLA.0000000000003460
Mascagni P, Fiorillo C, Urade T, Emre T, Yu T, Wakabayashi T, Felli E, Perretta S, Swanstrom L, Mutter D, Marescaux J, Pessaux P, Costamagna G, Padoy N, Dallemagne B (2020) Formalizing video documentation of the critical view of safety in laparoscopic cholecystectomy: a step towards artificial intelligence assistance to improve surgical safety. Surg Endosc 34:2709–2714. https://doi.org/10.1007/s00464-019-07149-3
Mascagni P, Vardazaryan A, Alapatt D, Urade T, Emre T, Fiorillo C, Pessaux P, Marescaux J, Costamagna G, Dallemagne B, Padoy N (2020) Artificial intelligence for surgical safety automatic assessment of the critical view of safety in laparoscopic cholecystectomy using deep learning. Ann Surg. https://doi.org/10.1097/SLA.0000000000004351
Mascagni P, Alapatt D, Urade T, Vardazaryan A, Mutter D, Marescaux J, Costamagna G, Dallemagne B, Padoy N (2021) A computer vision platform to automatically locate critical events in surgical videos: documenting safety in laparoscopic cholecystectomy. Ann Surg 274:e93–e95. https://doi.org/10.1097/SLA.0000000000004736
Mascagni P, Alapatt D, Laracca GG, Guerriero L, Spota A, Fiorillo C, Vardazaryan A, Quero G, Alfieri S, Baldari L, Cassinotti E, Boni L, Cuccurullo D, Costamagno G, Dallemagne B, Padoy N (2022) Multicentric validation of endodigest: a computer vision platform for video documentation of the critical view of safety in laparoscopic cholecystectomy. Surg Endosc. https://doi.org/10.1007/s00464-022-09112-1
Ward TM, Mascagni P, Madani A, Padoy N, Perretta S, Hashimoto DA (2021) Surgical data science and artificial intelligence for surgical education. J Surg Oncol 124:221–230. https://doi.org/10.1002/jso.26496
al Abbas AI, Jung JP, Rice MJK, Zureikat AH, Zeh HJ, Hogg ME, (2019) Methodology for developing an educational and research video library in minimally invasive surgery. J Surg Edu 76:745–755. https://doi.org/10.1016/j.jsurg.2018.10.011
Ibrahim AM, Varban OA, Dimick JB (2016) Novel uses of video to accelerate the surgical learning curve. J Laparoendosc Adv Surg Tech 26:240–242. https://doi.org/10.1089/lap.2016.0100
Mazer L, Varban O, Montgomery JR, Awad MM, Schulman A (2021) Video is better: why aren’t we using it ? A mixed-methods study of the barriers to routine procedural video recording and case review. Surg Endosc. https://doi.org/10.1007/s00464-021-08375-4
Pernar LIM, Robertson FC, Tavakkoli A, Sheu EG, Brooks DC, Smink DS (2017) An appraisal of the learning curve in robotic general surgery. Surg Endosc 31:4583–4596. https://doi.org/10.1007/s00464-017-5520-2
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJO (2013) Surgical skill and complication rates after bariatric surgery. New Eng J Med 369:1434–1442. https://doi.org/10.1056/nejmsa1300625
Stulberg JJ, Stulberg JJ, Huang R, Kreutzer L, Ban K, Champagne BJ, Steele SR, Johnson JK, Holl JL, Greenberg CC, Bilimoria KY (2020) Association between surgeon technical skills and patient outcomes. JAMA Surg 155:960–968. https://doi.org/10.1001/jamasurg.2020.3007
Varban OA, Thumma JR, Finks JF, Carlin AM, Ghaferi AA, Dimick JB (2021) Evaluating the effect of surgical skill on outcomes for laparoscopic sleeve gastrectomy: a video-based study. Ann Surg 273:766–771. https://doi.org/10.1097/SLA.0000000000003385
Idrees JJ, Rosinski BF, Chen Q, Bagante F, Merath K, White S, Pawlik TM (2018) Variation in medicare payments and reimbursement rates for hepatopancreatic surgery based on quality: is there a financial incentive for high-quality hospitals? J Am Coll of Surg 227:212–222. https://doi.org/10.1016/j.jamcollsurg.2018.04.005
Steastedt KP, Schwab P, O’Brien Z, Wakida E, Herrera K, Marcelo PGF, Agha-Mir-Salim L, Frigola XB, Ndulue EB, Marcelo A, Celi LA (2022) Global healthcare fairness: we should be sharing more, not less, data. PLOS Digit Health 1(10):e0000102. https://doi.org/10.1371/journal.pdig.0000102
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
FF is a consultant for Boston Scientific and Activ Surgical, DAH is a consultant for Johnson and Johnson Institute, and previously Activ Surgical and Verily Life Sciences. AM is a consultant for Activ Surgical. DPB is a consultant for Deep Surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Filicori, F., Bitner, D.P., Fuchs, H.F. et al. SAGES video acquisition framework—analysis of available OR recording technologies by the SAGES AI task force. Surg Endosc 37, 4321–4327 (2023). https://doi.org/10.1007/s00464-022-09825-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09825-3