Abstract
Background
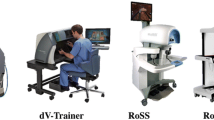
The da Vinci skills simulation curriculum has been validated in the literature. The updated simulator, SimNow, features restructured exercises that have not been formally validated. The purpose of this study is to validate the SimNow resident robotic basic simulation curriculum. This study also consists of a qualitative assessment that gives greater insight into the learner’s experience completing the robotic curriculum.
Methods
There were 18 participants in this study: 6 novices, 6 competent surgeons, and 6 expert surgeons. The curriculum comprised 5 exercises; participants completed three consecutive scored trials. Computer-derived performance metrics were recorded. The NASA Task Load Index survey was used to assess subjective mental workload. Subjects were asked a series of open-ended questions regarding their experience that were recorded and transcribed. Codes were identified using an inductive method, and themes were generated.
Results
Performance metrics were significantly different between novice versus competent and expert surgeons. There was no significant difference in any score metric between competent and expert surgeons. On average, overall score percentages for competent and expert surgeons were between 90.4 and 92.8% versus 70.5% for novices (p = 0.02 and p = 0.01). Expert surgeons perceived a higher level of performance completing the exercises than novice surgeons (15.8 vs. 45.8, p = 0.02). Participants noted a similar robotic experience, utilizing efficiency of motion and visual field skills. Participants agreed on exercise strengths, exercise weaknesses, and software limitations. Competent and expert surgeons were better able to assess the exercises’ clinical application.
Conclusions
The SimNow curriculum is a valid simulation training as part of a general surgery resident robotic curriculum. The curriculum distinguishes between novices compared to competent and expert surgeons, but not between competent and expert surgeons. Clinical training level does not affect the experience and mental workload using the robotic simulator, except for competent and expert surgeons’ ability to better assess clinical application.
Graphical abstract






Similar content being viewed by others
References
Azadi S, Green IC, Arnold A, Truong M, Potts J, Martino MA (2021) Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasive Gynecol 28(3):490–495. https://doi.org/10.1016/j.jmig.2020.12.001
Kneebone RL (2009) Practice, rehearsal, and performance. JAMA 302(12):1336. https://doi.org/10.1001/jama.2009.1392
Bric JD, Lumbard DC, Frelich MJ, Gould JC (2015) Current state of virtual reality simulation in robotic surgery training: a review. Surg Endosc 30(6):2169–2178. https://doi.org/10.1007/s00464-015-4517-y
Gavazzi A, Bahsoun AN, Van Haute W et al (2011) Face, content and construct validity of a virtual reality simulator for robotic surgery (SEP Robot). Ann R Coll Surg Engl 93(2):152–156. https://doi.org/10.1308/003588411X12851639108358
Alzahrani T, Haddad R, Alkhayal A et al (2013) Validation of the da Vinci Surgical Skill Simulator across three surgical disciplines: a pilot study. Can Urol Assoc J 7(7–8):E520–E529. https://doi.org/10.5489/cuaj.419
Shamim Khan M, Ahmed K, Gavazzi A et al (2013) Development and implementation of centralized simulation training: evaluation of feasibility, acceptability and construct validity. BJU Int 111(3):518–523. https://doi.org/10.1111/j.1464-410X.2012.11204.x
Culligan P, Gurshumov E, Lewis C, Priestley J, Komar J, Salamon C (2014) Predictive validity of a training protocol using a robotic surgery simulator. Female Pelvic Med Reconstr Surg 20:48–51
Hung AJ, Patil MB, Zehnder P, Cai J, Ng CK, Aron M, Gill IS, Desai MM (2012) Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. J Urol 187:630–637
Connolly M, Seligman J, Kastenmeier A, Goldblatt M, Gould JC (2014) Validation of a virtual reality-based robotic surgical skills curriculum. Surg Endosc 28(5):1691–1694. https://doi.org/10.1007/s00464-013-3373-x
Radi I, Tellez JC, Alterio RE et al (2022) Feasibility, effectiveness and transferability of a novel mastery-based virtual reality robotic training platform for general surgery residents. Surg Endosc. https://doi.org/10.1007/s00464-022-09106-z
Zhao B, Lam J, Hollandsworth HM, Lee AM, Lopez NE, Abbadessa B, Eisenstein S, Cosman BC, Ramamoorthy SL, Parry LA (2020) General surgery training in the era of robotic surgery: a qualitative analysis of perceptions from resident and attending surgeons. Surg Endosc 34(4):1712–1721. https://doi.org/10.1007/s00464-019-06954-0
Dreyfus SE (2004) The five-stage model of adult skill acquisition. Bull Sci Technol Soc 24(3):177–181. https://doi.org/10.1177/0270467604264992
Thornblade LW, Fong Y (2021) Simulation-based training in robotic surgery: contemporary and future methods. J Laparoendosc Adv Surg Tech A 31(5):556–560. https://doi.org/10.1089/lap.2021.0082
Bhakhri K, Harrison-Phipps K, Harling L, Routledge T (2021) Should robotic surgery simulation be introduced in the core surgical training curriculum? Front Surg 8:595203. https://doi.org/10.3389/fsurg.2021.595203
Mandava SH, Liu J, Maddox MM, Woodson B, Thomas R, Lee BR (2015) Stratification of expert vs novice laparoscopists using the basic laparoscopic urologic surgery (BLUS) curriculum at a single institution. J Surg Educ 72(5):964–968. https://doi.org/10.1016/j.jsurg.2015.03.006
Kelly DC, Margules AC, Kundavaram CR, Narins H, Gomella LG, Trabulsi EJ, Lallas CD (2012) Face, content, and construct validation of the da Vinci Skills Simulator. Urology 79(5):1068–1072. https://doi.org/10.1016/j.urology.2012.01.028
Sytek L, Inglehart MR, Ramaswamy V, Aronovich S, Edwards S, Kim-Berman H (2021) Comparisons of orthodontic residents’ performance and attitudes using 2D, 3D, and virtual reality surgical simulation methods. J Dent Educ 85(8):1415–1426. https://doi.org/10.1002/jdd.12598
Korzeniowski P, Chacon CS, Russell VR, Clarke SA, Bello F (2021) Virtual reality simulator for pediatric laparoscopic inguinal hernia repair. J Laparoendosc Adv Surg Tech A 31(11):1322–1330. https://doi.org/10.1089/lap.2020.0423
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jon C. Gould is a consultant for Ethicon, W.L. Gore, and BD. Matthew I. Goldblatt has the following disclosures: Speaking and consulting for W.L. Gore; Speaking, consulting, and research for Medtronic; and Research for Bard. Rana M. Higgins is a speaker for W.L. Gore and Intuitive Surgical. Mia S. Turbati has no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turbati, M.S., Goldblatt, M.I., Gould, J.C. et al. Robotic simulation: validation and qualitative assessment of a general surgery resident training curriculum. Surg Endosc 37, 2304–2315 (2023). https://doi.org/10.1007/s00464-022-09558-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09558-3