Abstract
Background
Endoscopic submucosal dissection (ESD) is one of the main methods of treatments for early gastric cancer. Sarcopenia is a known risk factor for postoperative adverse events; however, the effect of sarcopenia on gastric ESD is unclear. We investigated the impact of sarcopenia on short-term prognosis after gastric ESD.
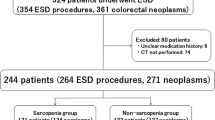
Methods
This was a retrospective cohort study. We reviewed 832 patients who underwent gastric ESD between January 2015 and December 2019 and classified them into two groups: sarcopenia and non-sarcopenia groups. The curative resection rate, adverse events, and lengths of hospital stay were evaluated. We also evaluated risk factors associated with adverse events.
Results
700 patients were analyzed (239 in the sarcopenia group and 461 in the non-sarcopenia group). The curative resection rates were similar in both groups. Common Terminology Criteria for Adverse Events (CTCAE) grade ≥ 2 (17% vs. 10%) were significantly more common, and the length of hospital stay was longer (8 vs. 7 days) in the sarcopenia group. Univariate analysis identified age ≥ 75 years, antithrombotic medication, history of gastric surgery, submucosal (SM) invasion, and sarcopenia as risk factors for CTCAE grade ≥ 2. Multivariate analysis showed that sarcopenia [odds ratio (OR) 1.79, 95% confidence interval (CI) 1.11–2.89, p = 0.016], history of gastric surgery (OR 9.32, 95% CI 1.97–44.05, p = 0.005), and SM invasion (OR 2.14, 95% CI 1.24–3.70, p = 0.006) were significant independent risk factors.
Conclusions
Sarcopenia significantly affected short-term prognosis and is a novel risk factor for gastric ESD.


Similar content being viewed by others
Change history
02 January 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00464-023-10655-0
References
International Agency for Research. CANCER FACT SHEETS. World Health Organization. https://gco.iarc.fr/today/data/factsheets/cancers/7-Stomach-fact-sheet.pdf. Accessed 22 February 2020.
Ono H, Yao K, Fujishiro M, Oda I, Uedo N, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Ichinose M, Matsui T (2021) Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition). Dig Endosc 33(1):4–20
Sumiyama K (2017) Past and current trends in endoscopic diagnosis for early stage gastric cancer in Japan. Gastric Cancer 20(S1):20–27
Hahn KY, Park CH, Lee YK, Chung H, Park JC, Shin SK, Lee YC, Kim HI, Cheong JH, Hyung WJ, Noh SH, Lee SK (2018) Comparative study between endoscopic submucosal dissection and surgery in patients with early gastric cancer. Surg Endosc 32(1):73–86
Tae CH, Shim KN, Kim BW, Kim JH, Hong SJ, Baik GH, Song HJ, Kim YS, Jang SH, Jung HK (2020) Comparison of subjective quality of life after endoscopic submucosal resection or surgery for early gastric cancer. Sci Rep 10(1):6680
Charlson ME, Pompei P, Ales KL, Mackenzie CT (1987) A new method of classifying prognostic in longitudinal studies: development. J Chronic Dis 40(5):373–383
Akasaka T, Nishida T, Tsutsui S, Michida T, Yamada T, Ogiyama H, Kitamura S, Ichiba M, Komori M, Nishiyama O, Nakanishi F, Zushi S, Nishihara A, Iijima H, Tsujii M, Hayashi N (2011) Short-term outcomes of endoscopic submucosal dissection (ESD) for early gastric neoplasm: multicenter survey by Osaka university ESD study group. Dig Endosc 23(1):73–77
Sekiguchi M, Oda I, Suzuki H, Abe S, Nonaka S, Yoshinaga S, Taniguchi H, Sekine S, Saito Y (2017) Clinical outcomes and prognostic factors in gastric cancer patients aged ≥85 years undergoing endoscopic submucosal dissection. Gastrointest Endosc 85(5):963–972
Toya Y, Endo M, Nakamura S, Akasaka R, Yanai S, Kawasaki K, Koeda K, Eizuka M, Fujita Y, Uesugi N, Ishida K, Sugai T, Matsumoto T (2019) Long-term outcomes and prognostic factors with non-curative endoscopic submucosal dissection for gastric cancer in elderly patients aged ≥ 75 years. Gastric Cancer 22(4):838–844
Iwai N, Dohi O, Naito Y, Inada Y, Fukui A, Takayama S, Ogita K, Terasaki K, Nakano T, Ueda T, Okayama T, Yoshida N, Katada K, Kamada K, Uchiyama K, Ishikawa T, Handa O, Takagi T, Konishi H, Yagi N, Itoh Y (2018) Impact of the Charlson comorbidity index and prognostic nutritional index on prognosis in patients with early gastric cancer after endoscopic submucosal dissection. Dig Endosc 30(5):616–623
Beaudart C, Reginster JY, Petermans J, Gillain S, Quabron A, Locquet M, Slomian J, Buckinx F, Bruyère O (2015) Quality of life and physical components linked to sarcopenia: the SarcoPhAge study. Exp Gerontol 69:103–110
Woo J, Leung J, Morley JE (2015) Defining sarcopenia in terms of incident adverse outcomes. J Am Med Dir Assoc 16(3):247–252
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG (2014) Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc 62(2):253–260
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G (2015) Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr 34(4):745–751
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, Kojima T, Kuzuya M, Lee JSW, Lee SY, Lee WJ, Lee Y, Liang CK, Lim JY, Lim WS, Peng LN, Sugimoto K, Tanaka T, Won CW, Yamada M, Zhang T, Akishita M, Arai H (2020) Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21(3):300-307.e2
Kamarajah SK, Bundred J, Tan BHL (2019) Body composition assessment and sarcopenia in patients with gastric cancer: a systematic review and meta-analysis. Gastric Cancer 22(1):10–22
Lee JS, Kim YS, Kim EY, Jin W (2018) Prognostic significance of CT-determined sarcopenia in patients with advanced gastric cancer. PLoS ONE 13(8):1–11
Shachar SS, Williams GR, Muss HB, Nishijima TF (2016) Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer 57:58–67
Kato M, Michida T, Kusakabe A, Sakai A, Hibino C, Kato M, Tokuda Y, Kawai T, Hamano M, Chiba M, Maeda K, Yamamoto K, Naito M, Ito T (2016) Safety and short-term outcomes of endoscopic submucosal dissection for early gastric cancer in elderly patients. Endosc Int Open 4(5):E521–E526
Association JGC (ed) (2017) Japanese Classification of Gastric Carcinoma, 15th edn. Kanehara Shuppan, Tokyo
Onodera T, Goseki N, Kosaki G (1986) Postoperative nutritional assessment in gastric and colorectal cancer. Nihon Geka Gakkai Zasshi 87(8):853–858
Bouillanne O, Morineau G, Dupant C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C (2005) Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 82(4):777–783
Japanese gastric cancer treatment guidelines 2018 (5th edition) (2021) Gastric Cancer 24(1):1–21
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R (1998) Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol 85(1):115–122
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936
Zhuang CL, Huang DD, Pang WY, Zhou CJ, Wang SL, Lou N, Ma LL, Yu Z, Shen X (2016) Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: analysis from a large-scale cohort. Med (United States) 95(13):e3164
Goto S, Arimoto J, Higurashi T, Takahashi K, Ohkubo N, Kawamura N, Tamura T, Tomonari H, Iwasaki A, Taniguchi L, Chiba H, Atsukawa K, Saigusa Y, Nakajima A (2020) Efficacy and safety of colorectal endoscopic submucosal dissection in patients with sarcopenia. Surg Endosc. https://doi.org/10.1007/s00464-020-08041-1
Prado CM, Purcell SA, Alish C, Pereira SL, Deutz NE, Heyland DK, Goodpaster BH, Tappenden KA, Heymsfield SB (2018) Implications of low muscle mass across the continuum of care: a narrative review. Ann Med 50(8):675–693
Shen W, Punyanitya M, Wang ZM, Gallagher D, St-Onge MP, Albu J, Heymsfield SB, Heshka S (2004) Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol 97(6):2333–2338
Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19–21, 1988. Am J Clin Nutr. 1989;50(5 Suppl):1121–1235
Ministry of Health, Labour and Welfare. https://www.mhlw.go.jp/english/database/db-hw/lifetb19/dl/lifetb19-01.pdf. Accessed 22 Feb 2020
Hori M, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H (2015) Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol 45(9):884–891
Nishide N, Ono H, Kakushima N, Takizawa K, Tanaka M, Matsubayashi H, Yamaguchi Y (2012) Clinical outcomes of endoscopic submucosal dissection for early gastric cancer in remnant stomach or gastric tube. Endoscopy 44(6):577–583
Choi CW, Kang DH, Kim HW, Hong JB, Park SB, Kim SJ, Cho M (2015) High dose proton pump inhibitor infusion versus bolus injection for the prevention of bleeding after endoscopic submucosal dissection: prospective randomized controlled study. Dig Dis Sci 60(7):2088–2096
Yamamoto K, Nagatsuma Y, Fukuda Y, Hirao M, Nishikawa K, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T (2017) Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer 20(5):913–918
Author information
Authors and Affiliations
Contributions
HH: Conception and design; patient enrollment and clinical treatment; data submission; analysis and interpretation of the data; drafting of the article. NT: Conception and design; patient enrollment and clinical treatment; data submission; analysis and interpretation of the data; drafting of the article. YT: Conception and design; patient enrollment and clinical treatment; data submission; analysis and interpretation of the data; critical revision of the article for important intellectual content. SN: Patient enrollment and clinical treatment; data submission. KF: Patient enrollment and clinical treatment; data submission. YM: Patient enrollment and clinical treatment; data submission. HM: Patient enrollment and clinical treatment; data submission. DO: Patient enrollment and clinical treatment; data submission. SY: Patient enrollment and clinical treatment; data submission. CM: Patient enrollment and clinical treatment; data submission. YT: Patient enrollment and clinical treatment; data submission. YS: Patient enrollment and clinical treatment; data submission. NY: Patient enrollment and clinical treatment; data submission. MF: Final approval of the article.
Corresponding author
Ethics declarations
Disclosures
Hiroyuki Hisada MD, Naoki Tamura MD, PhD, Yosuke Tsuji MD, PhD, Sayaka Nagao MD, PhD, Kazushi Fukagawa MD, PhD, Yuko Miura MD, PhD, Hiroya Mizutani MD, PhD, Daisuke Ohki MD, PhD, Seiichi Yakabi MD, PhD, Chihiro Minatsuki MD, PhD, Yu Takahashi MD, PhD, Yoshiki Sakaguchi MD, PhD, Nobutake Yamamichi MD, PhD, and Mitsuhiro Fujishiro MD, PhD have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hisada, H., Tamura, N., Tsuji, Y. et al. The impact of sarcopenia on adverse events associated with gastric endoscopic submucosal dissection. Surg Endosc 36, 6387–6395 (2022). https://doi.org/10.1007/s00464-021-08965-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08965-2