Abstract
Background
There are an estimated 100,000 cases of abdominal injury (ABI) in the USA, annually resulting in over $12 billion in direct medical cost and $18 billion in lost productivity. This study assesses the timeliness, safety, and efficacy of the surgical management of abdominal injuries (ABIs), hollow viscus injuries (HVIs), and colonic injuries (CIs) for patients residing in New York State (NYS).
Methods
Using data from NYS’s Statewide Planning and Research Cooperative System (SPARCS), we identified all trauma patients with ABI admitted between 2006 and 2015. We subdivided ABI into HVI and CI using diagnosis and procedure codes and examined processes of care and outcomes adjusting for patient characteristics, injury severity score, structural, and process indicators.
Results
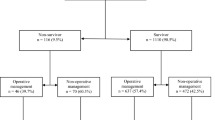
We identified 31,043 hospitalized patients with ABI, 71% were incurred from blunt forces. Most patients with ABI (72%) were treated at a Level I/II trauma center (TC) and 7% patients were transferred to Level I/II TC. Failure to be treated at Level I/II TC was associated with 16% increased hazard of death. HVI was diagnosed in 23% of ABI patients (n = 7294); 18% experienced delayed hollow viscus repair (dHVR); dHVR was associated with a 76% increased hazard of death. CI was diagnosed in 9% of ABI patients (n = 2921) and 18% experienced dHVR. Seventy-five percent of CI were repaired primarily (n = 1354). Less than 37% of stomas were reversed by 4 years of index trauma.
Conclusion
Most abdominal trauma in NYS was caused by motor vehicle accidents, falls, and assault. dHVR and not being treated at Level I/II TC were associated with worse outcomes. More research is needed to reduce under-triage and delays in the operative treatment of blunt abdominal trauma.


Similar content being viewed by others
References
Web-based Injury Statistics Query and Reporting System (WISQARSTM): Cost of Injury Reports (2014) Estimated number of nonfatal emergency department visits, and average and total lifetime costs, United States, 2010., Centers for disease control and prevention, National center for injury prevention and control, Atlanta, GA
Web-based Injury Statistics Query and Reporting System (WISQARSTM): Cost of Injury Reports (2014) Number of deaths and estimated average and total lifetime costs, United States, 2010. Centers for disease control and prevention, National center for injury prevention and control, Atlanta, GA
Trauma Quality Imporovement Program Committee (2016) National trauma data bank annual report 2016. American College of Surgeons, Chicago, IL
Adesanya AA, Ekanem EE (2004) A ten-year study of penetrating injuries of the colon. Dis Colon Rectum 47:2169–2177
Harmston C, Ward JBM, Patel A (2018) Clinical outcomes and effect of delayed intervention in patients with hollow viscus injury due to blunt abdominal trauma: a systematic review. Eur J Trauma Emerg Surg 44:369–376
Watts DD, Fakhry SM, Group EM-IHVIR (2003) Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the east multi-institutional trial. J Trauma 54:289–294
Neeki MM, Hendy D, Dong F, Toy J, Jones K, Kuhnen K, Yuen HW, Lux P, Sin A, Kwong E, Wong D (2017) Correlating abdominal pain and intra-abdominal injury in patients with blunt abdominal trauma. Trauma Surg Acute Care Open 2:e000109
National Quality Forum (2019) Population-Based Trauma Outcomes. National Quality Forum, Washington, DC. https://www.qualityforum.org/Publications/2019/05/Trauma_Outcomes_Final_Report.aspx
Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE (2010) Quality indicators for evaluating trauma care: a scoping review. Arch Surg 145:286–295
Moore L, Lavoie A, Sirois MJ, Amini R, Belcaid A, Sampalis JS (2013) Evaluating trauma center process performance in an integrated trauma system with registry data. J Emerg Trauma Shock 6:95–105
Gruen RL, Gabbe BJ, Stelfox HT, Cameron PA (2012) Indicators of the quality of trauma care and the performance of trauma systems. Br J Surg 99(Suppl 1):97–104
Bergen GS, Chen L-H, Warner M (2008) Injury in the United States: 2007 chartbook. National Center for Health Statistics, Hyattsville, MD
Web-based Injury Statistics Query and Reporting System (WISQARSTM): Injury Center (2018) Matrix of E-code groupings. Centers for Disease Control and Prevention, Atlanta, GA
Tian D (2019) Injury severity score. Accessed August 25, 2021 from https://github.com/dajuntian/InjurySeverityScore
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Haas B, Stukel TA, Gomez D, Zagorski B, De Mestral C, Sharma SV, Rubenfeld GD, Nathens AB (2012) The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. J Trauma Acute Care Surg 72:1510–1515 (discussion 1515–1517)
Choi J, Carlos G, Nassar AK, Knowlton LM, Spain DA (2021) The impact of trauma systems on patient outcomes. Curr Probl Surg 58:100840
Committee on Trauma American College of Surgeons (2014) Resources for optimal care of the injured patient. https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx. Accessed August 28, 2021
Krug EG, Sharma GK, Lozano R (2000) The global burden of injuries. Am J Public Health 90:523–526
Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, Najarian MP, Valenziano CP, Eastern Asociation for the Surgery of T (2002) Practice management guidelines for the evaluation of blunt abdominal trauma: the east practice management guidelines work group. J Trauma 53:602–615
Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF (2006) Usefulness of multidetector computed tomography for the initial assessment of blunt abdominal trauma patients. World J Surg 30:176–182
Ricciardi R, Paterson CA, Islam S, Sweeney WB, Baker SP, Counihan TC (2004) Independent predictors of morbidity and mortality in blunt colon trauma. Am Surg 70:75–79
Sharpe JP, Magnotti LJ, Weinberg JA, Shahan CP, Cullinan DR, Fabian TC, Croce MA (2013) Applicability of an established management algorithm for colon injuries following blunt trauma. J Trauma Acute Care Surg 74:419–424 (discussion 424–415)
Funding
This manuscript was funded by the New York State Empire Clinical Research Investigator Program (ECRIP) at Buffalo General Hospital and the Department of Surgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Schwaitzberg is a paid consultant for Nu View Surgical, Acuity Bio, Activ Surgical, Human Extensions, Levitra Magnetics, Amsel Surgical, and Arch Therapeutics (not related to the study). Dr. Hoffman proctored for Standard Bariatrics, Inc. and received compensation for food and travel from Intuitive Surgical, Inc. for training purposes. Drs. Simmonds, Myneni, Gray, Jordan, and Noyes and Ms. Towle-Miller do not have any conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Simmonds, I., Towle-Miller, L.M., Myneni, A.A. et al. Is New York State good at managing hollow viscus injury?. Surg Endosc 36, 6789–6800 (2022). https://doi.org/10.1007/s00464-021-08964-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08964-3