Abstract
Background
Laparoscopic techniques in colorectal surgery have been widely utilised due to short-term patient benefits but conversion to open surgery is associated with adverse short- and long-term patient outcomes. The aim of this study was to investigate the influence of dual specialist operating on the conversion rate and patient outcomes following laparoscopic colorectal surgery.
Methods
A prospectively populated colorectal cancer surgery database was reviewed. Cases were grouped into single or dual consultant procedures. Cluster analysis and odds ratio (OR) were used to identify risk factors for conversion. Primary outcome measures were conversion to open and five year overall survival (OS) calculated using the Kaplan–Meier log-rank method.
Results
750 patients underwent laparoscopic colorectal cancer resection between 2002 and 2015 (median age 73, 319 (42.5%) female, 282 (37.6%) rectal malignancies, 135 patients (18%) had two consultants). The single surgeon conversion rate was 20.4% compared to 5.5% for dual operating (OR 4.4, 95% CI 1.87–10.2, p < 0.001). There were no demographic or tumour differences between the laparoscopic/converted and number of surgeon groups. Two-step cluster analysis identified cluster I (lower risk) 406 patients, 8% converted and cluster II (higher risk) 261 patients, conversion rate 30%. Median follow-up was 48 months (range 0–168). Five-year OS was significantly inferior for both converted and single surgeon cases (63% vs. 77%, p < 0.001 and 61% vs. 70%, p = 0.033, respectively).
Conclusion
In selected colorectal cancer patients operated by fully trained laparoscopic surgeons, we observed a reduction in conversion with associated long-term survival benefit from dual operating specialists.


Similar content being viewed by others
References
Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ (2015) Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc 29(12):3443–3453
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003432.pub2
Currie AC, White I, Malietzis G, Moorghen M, Jenkins JT, Kennedy RH (2016) Outcomes following laparoscopic rectal cancer resection by supervised trainees. Br J Surg 103(8):1076–1083
Miskovic D, Ni M, Wyles SM, Tekkis P, Hanna GB (2012) Learning curve and case selection in laparoscopic colorectal surgery: systematic review and international multicenter analysis of 4852 cases. Dis Colon Rectum 55(12):1300–1310
Allaix ME, Furnee EJ, Mistrangelo M, Arezzo A, Morino M (2016) Conversion of laparoscopic colorectal resection for cancer: what is the impact on short-term outcomes and survival? World J Gastroenterol 22(37):8304–8313
Clancy C, O’Leary DP, Burke JP, Redmond HP, Coffey JC, Kerin MJ et al (2015) A meta-analysis to determine the oncological implications of conversion in laparoscopic colorectal cancer surgery. Colorectal Dis 17(6):482–490
Collinson FJ, Jayne DG, Pigazzi A, Tsang C, Barrie JM, Edlin R et al (2012) An international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus standard laparoscopic surgery for the curative treatment of rectal cancer. Int J Colorectal Dis 27(2):233–241
Miskovic D, Wyles SM, Ni M, Darzi AW, Hanna GB (2010) Systematic review on mentoring and simulation in laparoscopic colorectal surgery. Ann Surg 252(6):943–951
Boulind CE, Yeo M, Burkill C, Witt A, James E, Ewings P et al (2012) Factors predicting deviation from an enhanced recovery programme and delayed discharge after laparoscopic colorectal surgery. Colorectal Dis 14(3):e103–e110
King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH et al (2006) Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 93(3):300–308
Smart NJ, White P, Allison AS, Ockrim JB, Kennedy RH, Francis NK (2012) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 14(10):e727–e734
Harrison OJ, Smart NJ, White P, Brigic A, Carlisle ER, Allison AS et al. Operative time and outcome of enhanced recovery after surgery after laparoscopic colorectal surgery. JSLS 2014;18(2):265–72
Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP et al (2014) Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol 32(17):1804–1811
Coleman MG, Hanna GB, Kennedy R (2011) The National Training Programme for Laparoscopic Colorectal Surgery in England: a new training paradigm. Colorectal Dis 13(6):614–616
von EE, Altman, Egger DG, Pocock M, Gotzsche SJ, Vandenbroucke PC (2007) JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4(10):e296
Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J, Brown JM (2008) Patient factors influencing conversion from laparoscopically assisted to open surgery for colorectal cancer. Br J Surg 95(2):199–205
Healthcare Quality Improvement Partnership. UK National Bowel Cancer Audit Annual Report 2016. 2017. NHS Digital. 3-5-2017
Web References
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Jimenez C, Kaspar K, Rivera J, Talone A, Jentsch F (2016) Crew resource management. In: Proceedings of the human factors and ergonomics society annual meeting, vol 59, pp 946–950
Hallbeck MS, Lowndes BR, Bingener J, Abdelrahman AM, Yu D, Bartley A et al (2017) The impact of intraoperative microbreaks with exercises on surgeons: A multi-center cohort study. Appl Ergon 60:334–341
Park AE, Zahiri HR, Hallbeck MS, Augenstein V, Sutton E, Yu D et al (2017) Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg 265(2):340–346
Scheer JK, Hey L, LaGrone M, Daubs M, Ames CP (2016) 343 results of the 2015 SRS survey on single versus two attending surgeon approach for adult spinal deformity surgery. Neurosurgery 63(Suppl 1):201
Mallory MA, Losk K, Camuso K, Caterson S, Nimbkar S, Golshan M (2016) Does “two is better than one” apply to surgeons? Comparing single-surgeon versus co-surgeon bilateral mastectomies. Ann Surg Oncol 23(4):1111–1116
Yamada N, Amano R, Kimura K, Murata A, Yashiro M, Tanaka S et al (2015) Two-surgeon technique for liver transection using precoagulation by a soft-coagulation system and ultrasonic dissection. Hepatogastroenterology 62(138):389–392
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Prof. Francis, Mr. Curtis, Dr. Crilly, Miss. Noble, Dr. Dyke, Mr. Hipkiss, Mr. Dalton, Mr. Allison, Dr. Salib and Mr. Ockrim confirm they have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
464_2018_6097_MOESM1_ESM.tif
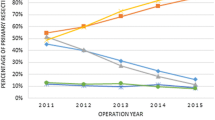
Supplementary material 1 (TIF 1662 KB) Activity and conversion rate across the study timeframe. No significant difference in conversion rate is seen between years (p = 0.109)
464_2018_6097_MOESM2_ESM.tif
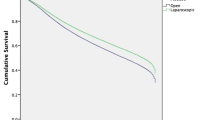
Supplementary material 2 (TIF 1200 KB) Overall survival for the entire cohort displayed by histopathologically determined tumour stage. More advanced tumours are seen to have lower OS (p = 0.062)
464_2018_6097_MOESM3_ESM.tif
Supplementary material 3 (TIF 1191 KB) Overall survival for cases completed laparoscopically displayed by tumour stage. Again, as expected, OS is observed to mirror staging data (p = 0.105)
464_2018_6097_MOESM4_ESM.tif
Supplementary material 4 (TIF 1055 KB) Supplementary Figure 2c - Overall survival for converted cases displayed by tumour stage. Once more long term survival follows tumour staging results (p = 0.105)
Rights and permissions
About this article
Cite this article
Francis, N.K., Curtis, N.J., Crilly, L. et al. Does the number of operating specialists influence the conversion rate and outcomes after laparoscopic colorectal cancer surgery?. Surg Endosc 32, 3652–3658 (2018). https://doi.org/10.1007/s00464-018-6097-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6097-0