Abstract
Background
Anastomotic leakage presents the most feared complication after low anterior resection (LAR). A proximal diversion of the gastrointestinal tract is recommended to avoid septic complications of anastomotic leakage. The aim of the present study was to evaluate the benefits and risks of diverting ileostomy (DI) created during laparoscopic LAR because of low rectal cancer.
Methods
This was a retrospective clinical cohort study conducted to assess outcomes of laparoscopic LAR with/without DI in a single institution within a 6-year period.
Results
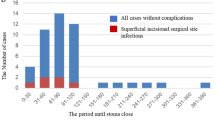
In total, 151 patients were enrolled in the study (73 patients without DI, 78 patients with DI). There were no significant differences between both groups regarding demographic and clinical features. Overall 30-day morbidity rates were significantly lower in patients without DI (23.3 vs. 42.3 %, P = 0.013). Symptomatic anastomotic leakage occurred more frequently in patients without DI (9.6 vs. 2.5 %, P = 0.090); surgical intervention was needed in 6.8 % of patients without DI. Post-operative hospital stay was significantly longer in the group of patients with DI (11.3 ± 8.5 vs. 8.1 ± 6.9 days, P = 0.013). Stoma-related complications occurred in 42 of 78 (53.8 %) patients with DI; some patients had more than one complication. Acute surgery was needed in 9 patients (11.5 %) because of DI-related complications. Small bowel obstruction due to DI semi-rotation around its longitudinal axis was seen in 3 patients (3.8 %) and presents a distinct complication of DI laparoscopic construction. The mean interval between LAR and DI reversal was more than 8 months; only 19.2 % of patients were reversed without delay (≤4 months). Morbidity after DI reversal was 16.6 %; re-laparotomy was necessary in 2.5 % of patients.
Conclusions
The present study indicates that DI protects low rectal anastomosis from septic complications at a cost of many stoma-related complications, substantial risk of acute surgery necessity and long stoma periods coupled with decreased quality of life.
Similar content being viewed by others
References
How P, Shihab O, Tekkis P, Brown G, Quirke P, Heald R, Moran B (2011) A systematic review of cancer related patient outcomes after anterior resection and abdominoperineal excision for rectal cancer in the total mesorectal excision era. Surg Oncol 20:149–155
Herzog T, Belyaev O, Chromik AM, Weyhe D, Mueller CA, Munding J, Tannapfel A, Uhl W, Seelig MH (2010) TME quality in rectal cancer surgery. Eur J Med Res 15:292–296
Ihnát P, Delongová P, Horáček J, Ihnát Rudinská L, Vávra P, Zonča P (2015) The impact of standard protocol implementation on the quality of colorectal cancer pathology reporting. World J Surg 39(1):259–265
Paun BC, Cassie S, MacLean AR, Dixon E, Buie D (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251:807–818
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak. Ann Surg 253:890–899
Matthiessen P, Hallbook O, Andersson M, Rutegård J, Sjödahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Color Dis 6:462–469
Marusch F, Koch A, Schmidt U, Geibetaler S, Dralle H, Saeger HD, Wolff S, Nestler G, Pross M, Gastinger I, Lippert H (2002) Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum 45:1164–1171
Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H (2005) Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg 92:1137–1142
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev. doi:10.1002/14651858
Hűser N, Michalski CW, Erkan M, Schuster T, Rosengerg R, Kleeff J, Friess H (2008) Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 248:52–60
Jafari MD, Halabi WJ, Jafari F, Nguyen VQ, Stamos MJ, Carmichael JC, Mills SD (2013) Morbidity of diverting ileostomy for rectal cancer: analysis of the American College of Surgeons National Surgical Quality Improvement Program. Ann Surg 79(10):1034–1039
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: When is it necessary? Langengecks Arch Surg 400:145–152
Nastro P, Knowles CH, McGrath A, Heyman B, Porrett TRC, Lunniss PJ (2010) Complications of intestinal stomas. Br J Surg 97:1885–1889
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91:1111–1124
Janson M, Lindholm E, Anderberg B, Haglind E (2007) Randomized trial of health-related quality of life after open and laparoscopic surgery for colon cancer. Surg Endosc 21:747–753
Ihnát P, Martínek L, Mitták M, Vávra P, Ihnát Rudinská L, Zonča P (2014) Quality of life after laparoscopic and open resection of colorectal cancer. Dig Surg 31(3):161–168
Wong NY, Eu KW (2005) A defunctioning ileostomy does not prevent clinical anastomotic leak after a low anterior resection: a prospective, comparative study. Dis Colon Rectum 48:2076–2079
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tier E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351
Floodeen H, Linggren R, Matthiessen P (2013) When are defunctioning stomas in rectal cancer surgery really reversed? Results from a population-based single center experience. Scand J Surg 102(4):246–250
Seo SI, Yu CS, Kim GS, Lee JL, Yoon YS, Kim CW, Lim SB, Kim JC (2013) The role of diverting stoma after an ultra-low anterior resection for rectal cancer. Ann Coloproctol 29(2):66–71
Poon RT, Chu KW, Ho JW, Chan CW, Law WL, Wong J (1999) Prospective evaluation of selective defunctioning stoma for low anterior resection with total mesorectal excision. World J Surg 23:463–467
Nurkin S, Kakarla VR, Ruiz DE, Cance WG, Tiszenkel HI (2013) The role of faecal diversion in low rectal cancer: a review of 1791 patients having rectal resection with anastomosis for cancer, with and without a proximal stoma. Color Dis 15(6):e309–e316
Leester B, Asztalos I, Polnyib C (2002) Septic complications after low anterior rectal resection—Is diverting stoma still justified? Acta Chir Iugosl 49:67–71
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85:355–358
Snijders HS, van Leersum NJ, Henneman D, de Vries AC, Tollenaar RA, Stiggelbout AM, Wouters MW, Dekker JW (2015) Optimal treatment strategy in rectal cancer surgery: Should we be cowboys or chickens? Ann Surg Oncol 22:3582–3589
Shellito PC (1998) Complications of abdominal stoma surgery. Dis Colon Rectum 41:1562–1572
Harris DA, Egbeare D, Jones S, Benjamin H, Woodward A, Foster ME (2005) Complications and mortality following stoma formation. Ann R Coll Surg Engl 87(6):427–431
Gessler B, Haglind E, Angenete E (2012) Loop ileostomies in colorectal cancer patients—morbidity and risk factors for nonreversal. J Surg Res 178(2):708–714
Åkesson O, Syk I, Lindmark G, Buchwald P (2012) Morbidity related to defunctioning loop ileostomy in low anterior resection. Int J Colorectal Dis 27(12):1619–1623
Robertson I, Leung E, Hughes D, Spiers M, Donnelly L, Mackenzie I, Macdonald A (2005) Prospective analysis of soma-related complications. Color Dis 7(3):279–285
Waterland P, Goonetilleke K, Naumann DN, Sutcliff M, Soliman F (2015) Defunctioning ileostomy reversal rates and reasons for delayed reversal: Does delay impact on complications of ileostomy reversal? A study of 170 defunctioning ileostomies. J Clin Med Res 7(9):685–689
Sier MF, van Gelder L, Ubbink DT, Bemelman WA, Oostenbroek RJ (2015) Factors affecting timing of closure and non-reversal of temporary ileostomies. Int J Colorectal Dis 30:1185–1192
Phatak UR, Kao LS, You YN, Rodriguez-Bigas MA, Skibber JM, Feig BW, Nguyen S, Chang GJ (2014) The impact of ileostomy-related complications on the multidisciplinary treatment of rectal cancer. Ann Surg Oncol 21(2):507–512
Chow A, Tilnea HS, Paraskeve P, Jeyarajah S, Zacharakis E, Purkayastha S (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6107 cases. Int J Colorectal Dis 24:711–723
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Peter Ihnát, Petra Guňková, Matúš Peteja, Petr Vávra, Anton Pelikán and Pavel Zonča have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ihnát, P., Guňková, P., Peteja, M. et al. Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30, 4809–4816 (2016). https://doi.org/10.1007/s00464-016-4811-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4811-3