Abstract
Background
The purpose of this study was to develop a new objective assessment system for the suture ligature method employed in the laparoscopic intestinal anastomosis model. Suturing skills were evaluated objectively using this system.
Methods
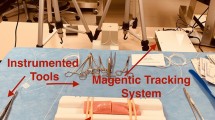
This study compared 17 expert surgeons, each of whom had performed >500 laparoscopic procedures, with 36 novice surgeons, each of whom had performed <15 laparoscopic procedures. Each examinee performed a specific skill assessment task using an artificial model that mimics living tissue, which is linked with the Suture Simulator Instruction Evaluation Unit. The model used internal air pressure measurements and image processing to evaluate suturing skills. Five criteria were used to evaluate the skills of participants.
Results
The volumes of air pressure leak in the expert and novice groups were 21.13 ± 6.68 and 8.51 ± 8.60 kPa, respectively. The numbers of full-thickness sutures in the expert and novice groups were 2.94 ± 0.24 pairs and 2.47 ± 0.77 pairs, respectively. Suture tensions in the expert and novice groups were 60.99 ± 11.81 and 80.90 ± 16.63 %, respectively. The areas of wound-opening in the expert and novice groups were 1.76 ± 2.17 and 11.06 ± 15.37 mm2, respectively. The performance times in the expert and novice groups were 349 ± 120 and 750 ± 269 s, respectively. Significant differences between the expert and novice groups for each criterion were observed. The acceptable range of values for each criterion except for the number of full-thickness sutures was statistically defined by the performance of the expert group.
Conclusions
Our system is useful for the quantitative assessment of suturing skill in laparoscopic surgery. We believe that this system is a useful tool for training and assessment of laparoscopic surgeons.




Similar content being viewed by others
References
Verdaasdonk EGG, Dankelman J, Lange JF, Stassen LPS (2008) Transfer validity of laparoscopic knot-tying training on a VR simulator to a realistic environment: a randomized controlled trial. Surg Endosc 22:1636–1642
Hofstad EF, Våpenstad C, Chmarra MK et al (2013) A study of psychomotor skills in minimally invasive surgery: what differentiates expert and nonexpert performance. Surg Endosc 27:854–863
Uemura M, Tomikawa M, Nagao Y et al (2014) Significance of metacognitive skills in laparoscopic surgery assessed by essential task simulation. Minim Invasive Ther Allied Technol 23:165–72
Uemura M, Tomikawa M, Kumashiro R et al (2014) Analysis of hand motion differentiates expert and novice surgeons. J Surg Res 188:8–13
Tanoue K, Ieiri S, Konishi K et al (2008) Effectiveness of endoscopic surgery training for medical students using a virtual reality simulator versus a box trainer: a randomized controlled trial. Surg Endosc 22:985–990
Ieiri S, Nakatsuji T, Higashi M et al (2010) Effectiveness of basic endoscopic surgical skill training for pediatric surgeons. Pediatr Surg Int 26:947–954
Ieiri S, Ishii H, Souzaki R et al (2013) Development of an objective endoscopic surgical skill assessment system for pediatric surgeons: suture ligature model of the crura of the diaphragm in infant fundoplication. Pediatr Surg Int. doi:10.1007/s00383-013-3276-x
Uemura M, Tomikawa M, Kumashiro R et al (2014) Analysis of hand motion differentiates expert and novice surgeons. J Surg Res 188:8–13
Yamaguchi S, Yoshida D, Kenmotsu H et al (2011) Objective assessment of laparoscopic suturing skills using a motion-tracking system. Surg Endosc 25:771–775
Aggarwal R, Grantcharov TP, Eriksen JR et al (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244:310–314
Wilson M, McGrath J, Vine S et al (2010) Psychomotor control in a virtual laparoscopic surgery training environment: gaze control parameters differentiate novices from experts. Surg Endosc 24:2458–2464
Bell AK, Zhou M, Schwaitzberg SD, Cao CGL (2009) Using a dynamic training environment to acquire laparoscopic surgery skill. Surg Endosc 23:2356–2363
Lauretta A, Bellomo RE, Galanti F, Tonizzo CA, Infantino A (2012) Laparoscopic low ventral rectocolpopexy (LLVR) for rectal and rectogenital prolapse: surgical technique and functional results. Tech Coloproctol 16:477–483
Hemming K, Pinkney T, Futaba K et al (2013) A systematic review of systematic reviews and panoramic meta-analysis: staples versus sutures for surgical procedures. PLoS ONE 8:e75132
Fumagalli Romario U, Ceolin M, Porta M, Rosati R (2012) Laparoscopic repair of epiphrenic diverticulum. Semin Thorac Cardiovasc Surg 24:213–217
Zimmitti G, Vauthey J-N, Shindoh J et al (2013) Systematic use of an intraoperative air leak test at the time of major liver resection reduces the rate of postoperative biliary complications. J Am Coll Surg 217:1028–1037
Dehabadi M, Fernando B, Berlingieri P (2014) The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg 12:258–268
Botden SMBI, de Hingh IHJT, Jakimowicz JJ (2009) Suturing training in augmented reality: gaining proficiency in suturing skills faster. Surg Endosc 23:2131–2137
Horeman T, Blikkendaal MD, Feng D et al (2014) Visual force feedback improves knot-tying security. J Surg Educ 71:133–141
Morse BC, Simpson JP, Jones YR et al (2013) Determination of independent predictive factors for anastomotic leak: analysis of 682 intestinal anastomoses. Am J Surg 206:950–955 (discussion 955–956)
Cui Y, Chen H (2003) The effect of tension on esophagogastric anastomotic wound healing in rats. J Cardiovasc Surg (Torino) 44:775–778
Waninger J, Kauffmann GW, Shah IA, Farthmann EH (1992) Influence of the distance between interrupted sutures and the tension of sutures on the healing of experimental colonic anastomoses. Am J Surg 163:319–323
Oguma J, Ozawa S, Morikawa Y et al (2007) Knot-tying force during suturing and wound healing in the gastrointestinal tract. J Surg Res 140:129–134
Forestier G, Lalys F, Riffaud L, Trelhu B, Jannin P (2012) Classification of surgical processes using dynamic time warping. J Biomed Inform 45:255–264
Neumuth T, Jannin P, Strauss G, Meixensberger J, Burgert O (2009) Validation of knowledge acquisition for surgical process models. J Am Med Inform Assoc 16:72–80
Disclosures
Drs. Uemura, Yamashita, Tomikawa, Obata, Souzaki, Ieiri, Ohuchida, Matsuoka, Katayama, and Hashizume have no conflict of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uemura, M., Yamashita, M., Tomikawa, M. et al. Objective assessment of the suture ligature method for the laparoscopic intestinal anastomosis model using a new computerized system. Surg Endosc 29, 444–452 (2015). https://doi.org/10.1007/s00464-014-3681-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3681-9