Abstract
Introduction
The risk of venous thromboembolic (VTE) events is increased in patients undergoing bariatric surgery. Population studies examining VTE rates after bariatric surgery often lack details and uniformity regarding the prophylactic regimens used. The aim of this study was to determine the incidence of VTE in patients undergoing laparoscopic bariatric surgery.
Methods
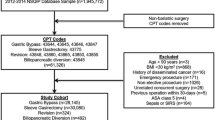
Database searches from Cleveland Clinic bariatric surgery programs in Cleveland, OH, and Weston, FL, were conducted from January 2005 to January 2013. Mechanical and chemical prophylaxes were provided for all patients as per protocol. Data on age, gender, body mass index (BMI), interval between procedure and VTE, inpatient versus outpatient status, anticoagulation prophylaxis, type of surgery and mortality were collected.
Results
A total of 4,293 patients underwent primary or revisional bariatric surgery during this 8-year time period. VTE events were identified in 57 patients (1.3 %). Pulmonary embolism (PE) was identified in 39 patients (0.9 %), and 15 of these patients had negative duplex studies of the lower extremities. Deep venous thrombosis only was identified in 18 patients (0.4 %). VTE rates for gastric bypass (n = 2,945), sleeve gastrectomy (n = 709), gastric banding (n = 467) and revisional procedures (n = 171) were 1.1, 2.9, 0.2 and 6.4 %, respectively. Eight patients had VTE diagnosed during their inpatient stay. The mean time to VTE diagnosis after surgery was 24 days. Seventeen patients who developed VTE had been prescribed extended prophylaxis for 2–4 weeks after discharge. There was only one VTE-related mortality from PE reported in this cohort (0.02 %). Univariate and multivariate analyses revealed age, BMI, open and revisional surgery as predictive of VTE (p < 0.05).
Conclusion
The risk of VTE among morbidly obese patients undergoing bariatric surgery is persistent despite use of laparoscopy and aggressive prophylactic anticoagulation policy. Patients with advanced age, higher BMI and those undergoing open or revisional surgery are at higher risk of postoperative VTE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Brotman DJ, Shihab HM, Prakasa KR et al (2013) Pharmacologic and mechanical strategies for preventing venous thromboembolism after bariatric surgery: a systematic review and meta-analysis. JAMA Surg 148(7):675–686
Borch KH, Braekkan SK, Mathiesen EB et al (2009) Abdominal obesity is essential for the risk of venous thromboembolism in the metabolic syndrome: the tromso study. J Thromb Haemost 7(5):739–745
Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW (2008) Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 117(1):93–102
Finks JF, English WJ, Carlin AM et al (2012) Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan bariatric surgery collaborative. Ann Surg 255(6):1100–1104
Carmody BJ, Sugerman HJ, Kellum JM et al (2006) Pulmonary embolism complicating bariatric surgery: detailed analysis of a single institution’s 24-year experience. J Am Coll Surg 203(6):831–837
Birkmeyer NJ, Finks JF, Carlin AM et al (2012) Comparative effectiveness of unfractionated and low-molecular-weight heparin for prevention of venous thromboembolism following bariatric surgery. Arch Surg 147(11):994–998
Morino M, Toppino M, Forestieri P, Angrisani L, Allaix ME, Scopinaro N (2007) Mortality after bariatric surgery: analysis of 13, 871 morbidly obese patients from a national registry. Ann Surg 246(6):1002–1007 discussion 1007-9
Goldfeder LB, Ren CJ, Gill JR (2006) Fatal complications of bariatric surgery. Obes Surg 16(8):1050–1056
Mechanick JI, Youdim A, Jones DB et al (2013) Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American association of clinical endocrinologists, the obesity society, and American society for metabolic & bariatric surgery. Obesity (Silver Spring) 21(Suppl 1):S1–S27
Stein PD, Matta F (2013) Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg 23(5):663–668
Winegar DA, Sherif B, Pate V, DeMaria EJ (2011) Venous thromboembolism after bariatric surgery performed by bariatric surgery center of excellence participants: analysis of the bariatric outcomes longitudinal database. Surg Obes Relat Dis 7(2):181–188
Birkmeyer NJ, Share D, Baser O et al (2010) Preoperative placement of inferior vena cava filters and outcomes after gastric bypass surgery. Ann Surg 252(2):313–318
Disclosure
Mohammad H. Jamal, Ricard Corcelles, Hideharu Shimizu, Mathew Kroh, Fernando M. Safdie, Raul Rosenthal, Stacy A. Brethauer and Philip R. Schauer have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jamal, M.H., Corcelles, R., Shimizu, H. et al. Thromboembolic events in bariatric surgery: a large multi-institutional referral center experience. Surg Endosc 29, 376–380 (2015). https://doi.org/10.1007/s00464-014-3678-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3678-4