Abstract
Background and aim
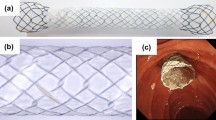
Partially covered self-expanding metal stents (PCMS) have been extensively used for palliation of malignant distal biliary stricture. Many centers have been using them as a bridge to surgery (BTS) regardless of resectability with or without eventual neoadjuvant therapy. We analyzed the outcome of all patients receiving PCMS and subsequently referred for surgery in our institution.
Methods
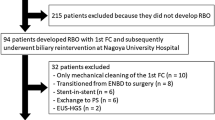
Our prospectively established pancreaticobiliary database was retrospectively analyzed to retrieve all patients with malignant biliary stricture who underwent PCMS placement and subsequently went for curative surgical attempt at our institution. Cancer type and staging, adverse events related to stent placement or surgery, type of surgery performed, time between stenting and surgery, length of postoperative hospitalization, and postoperative follow-up were recorded.
Results
27 patients (21 men; median age 66 years, range 39–82 years) received PCMS. Indications for placement included biliary stricture related to pancreatic cancer (n = 23) or other malignancies (n = 4). Median time between stenting and surgery was 32 days (range 6–569 days). Median time of hospitalization post surgery was 7 days (1–40 days). All patients underwent exploratory laparoscopy, followed in 9 (33.3%) by Whipple procedure with uneventful removal of the PCMS. Eighteen patients (66.6%) had their attempted curative resection terminated early due to intraoperative evidence of metastatic spread, with 8 (30%) patients undergoing peritoneal or liver metastasis biopsy. PCMS were left in place in those 18 patients. Complications related to PCMS in the bridge-to-surgery period included migration (n = 2, 7.4%) and tissue overgrowth (n = 1, 3.4%), all of them managed by endoscopic removal and replacement with PCMS. Median follow-up post surgery was 210 days (range 9–1,642 days).
Conclusion
PCMS are an appropriate BTS option. For resectable patients, PCMS results in biliary drainage and allows for neoadjuvant treatment without portending subsequent curative resection (Whipple). For unresectable patients, long-term biliary drainage is provided by PCMS.
Similar content being viewed by others
References
Warshaw AL, Fernandez-del Castillo C (1992) Pancreatic carcinoma. N Engl J Med 326:455–465
Smith AC, Dowsett JF, Russell RC. Hatfield AR, Cotton PB (1994) Randomized trial of endoscopic stenting versus surgical bypass in malignant low bile duct obstruction. Lancet 344:1655–1660
Sheperd HA, Royle G, Ross AP, Diba A, Arthur M, Colin-Jones D (1988) Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg 75:1166–1168
Andersen JR, Sorensen SM, Kruse A, Rokkjaer M, Matzen P (1989) Randomized trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut 30:1132–1135
Prat F, Chapat O, Ducot B, Ponchon T, Pelletier G, Fritsch J, Choury AD, Buffet C (1998) A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. Gastrointest Endosc 47:1–7
Arguedas MR, Heudebert GH, Stinnett AA, Wilcox CM (2002) Biliary stents in malignant obstructive jaundice due to pancreatic carcinoma: a cost-effectiveness analysis. Am J Gastroenterol 97:898–904
Mullen JT, Lee JH, Gomez HF, Ross WA, Fukami N, Wolf RA, Abdalla EK, Vauthey JN, Lee JE, Pisters PWT, Evans DB (2005) Pancreaticoduodenectomy after placement of endobiliary metal stents. J Gastroenterol Hepatol 3:1229–1237
Wasan SM, Ross WA, Staerkel GA, Lee JH (2005) Use of expandable metallic biliary stents in resectable pancreatic cancer. Am J Gastroenterol 100:2056–2061
Van der Gaag NA, Rauws EAJ, van Eijck CHJ, Bruno MJ, van der Harst E, Kubben FJGM, Gerritsen JJGM, Greve JW, Gerhards MF, de Hingh IHJT, Klinkenbijl JH, Nio CY, de Castro SMM, Busch ORC, van Gulik TM, Bossuyt PMM, Gouma DJ (2010) Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 362:129
Kahaleh M, Tokar J, Conaway MR, Brock A, Le T, Adams RB, Yeaton P (2005) Efficacy and complications of covered WallStents in malignant distal biliary obstruction. Gastrointest Endosc 61:528–533
Barkin JS, Goldstein JA (1999) Diagnostic approach to pancreatic cancer. Gastroenterol Clin North Am 28:709–722 xi
Flamm CR, Mark DH, Aronson N (2002) Evidence based assessment of ERCP approaches to managing pancreaticobiliary malignancies. Gastrointest Endosc 56(6):218–225
Sewnath ME, Karsten TM, Prins M, Rauws EJ, Obertop H, Gouma DJ (2002) A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice. Ann Surg 236:17–27
Povoski SP, Karpeh MS Jr, Conlon KC, Blumgart LH, Brennan MF (1999) Preoperative biliary drainage: impact on intraoperative bile cultures and infectious morbidity and mortality after pancreaticoduodenectomy. J Gastrointest Surg 3:496
Jagannath P, Dhir V, Shrikhande S, Shah RC, Mullerpatan P, Mohandas KM (2005) Effect of preoperative biliary stenting on immediate outcome after pancreaticoduodenectomy. Br J Surg 92:356–361
Pisters PW, Hudec WA, Lee JE, Raijman I, Lahoti S, Janjan NA, Rich TA, Crane CH, Lenzi R, Wolff RA, Abbruzzese JL, Evans DB (2000) Preoperative chemoradiation for patients with pancreatic cancer: toxicity of endobiliary stents. J Clin Oncol 18:860–867
Vauthey JN, Dixon E (2009) AHPBA/SSO/SSAT Consensus conference on resectable and borderline resectable pancreatic cancer: rationale and overview of the conference. Ann Surg Oncol 16(7):1725–1726. Epub 2009 Apr 24
Disclosures
Authors Pop, Richter, Sauer, Ho, Adams, Phillips, and Rehan have no conflicts of interest or financial ties to disclose. Dr. Bauer has received honoraria for lectures from IMER (Institute for Medical Education and Research). Dr. Shami is a consultant for Olympus. Dr. Kahaleh has received grant support from Boston Scientific, Olympus, Alveolus, Conmed, and Cook Medical, and honoraria for lectures from Boston Scientific, Olympus, and Axcan Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pop, G.H., Richter, J.A., Sauer, B. et al. Bridge to surgery using partially covered self-expandable metal stents (PCMS) in malignant biliary stricture: an acceptable paradigm?. Surg Endosc 25, 613–618 (2011). https://doi.org/10.1007/s00464-010-1231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1231-7