Abstract
Background
Stent placement in the distal duodenum or proximal jejunum with a therapeutic gastroscope can be difficult, because of the reach of the endoscope, loop formation in the stomach, and flexibility of the gastroscope. The use of a colonoscope may overcome these problems.
Objective
To report our experience with distal duodenal stent placement in 16 patients using a colonoscope.
Methods
Multicenter, retrospective series of patients with a malignant obstruction at the level of the distal duodenum and proximal jejunum and treated by stent placement using a colonoscope. Main outcome measurements are technical success, ability to eat, complications, and survival.
Results
Stent placement was technically feasible in 93% (15/16) of patients. Food intake improved from a median gastric outlet obstruction scoring system (GOOSS) score of 1 (no oral intake) to 3 (soft solids) (p = 0.001). Severe complications were not observed. One patient had persistent obstructive symptoms presumably due to motility problems. Recurrent obstructive symptoms were caused by tissue/tumor ingrowth through the stent mesh [n = 6 (38%)] and stent occlusion by debris [n = 1 (6%)]. Reinterventions included additional stent placement [n = 5 (31%)], gastrojejunostomy [n = 2 (12%)], and endoscopic stent cleansing [n = 1 (6%)]. Median survival was 153 days.
Conclusion
Duodenal stent placement can effectively and safely be performed using a colonoscope in patients with an obstruction at the level of the distal duodenum or proximal jejunum. A colonoscope has the advantage that it is long enough and offers good endoscopic stiffness, which avoids looping in the stomach.
Similar content being viewed by others
Patients with gastrointestinal malignancies may develop an obstruction at the level of the duodenum. The largest group consists of patients with pancreatic cancer, who develop in 10–20% of cases a gastric outlet obstruction (GOO) [1–3]. Other causes of GOO include periampullary carcinoma, lymphoma, primary duodenal carcinoma as well as metastases to the duodenum [4–6]. Palliative treatment of GOO is mandatory as it is associated with a rapid deterioration of the clinical status due to vomiting, dehydration, and malnutrition [2].
Stent placement is a commonly used palliative treatment, because this modality is less invasive compared with a surgically performed gastrojejunostomy. In addition, results of small randomized trials concluded that stent placement was superior to gastrojejunostomy [7, 8]. Stent placement in patients with a malignant obstruction at the level of the distal stomach or proximal duodenum (superior, descending and first half of the horizontal part) is routinely performed with a therapeutic gastroscope. However, stent placement in the distal part of the duodenum (second half of the horizontal part and ascending part of the duodenum) or proximal jejunum with a therapeutic gastroscope can be difficult. The main factors limiting the use of a gastroscope for distal duodenal stenting are the relatively short endoscope length, and shaft flexibility, which may cause looping of the scope into the stomach. The use of a colonoscope may potentially overcome these problems [6, 9–11].
In this series, we report our experience with distal duodenal stent placement in 16 patients using a colonoscope.
Patients and methods
Patients
All patients with a malignant obstruction at the level of the distal duodenum and proximal jejunum and treated by stent placement using a colonoscope at the Erasmus MC-University Medical Center Rotterdam, The Netherlands, the University Medical Center Utrecht, The Netherlands and Istituto Clinico Humanitas, Milan, Italy in the period 2001–2006 were included. Data were obtained from the clinical records and endoscopy report databases at both centers, and by telephone interviews with patients and/or their treating physicians or general practitioners. Information that was collected included demographic information, procedural characteristics, and follow-up information on complications, persistent and recurrent obstructive symptoms, reinterventions, and survival.
Endoscopic procedure
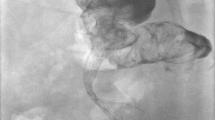
All stents were placed using a colonoscope after an intravenous dose of midazolam (Roche, Basel, Switzerland) or propofol (AstraZeneca, Zoetermeer, The Netherlands). The length of the stricture was determined using contrast fluoroscopy of the duodenum during the procedure. A guide wire was then introduced through the stricture and the stent was advanced over the wire. Stent length was chosen to aim at a length of 1–2 cm more than the stricture. Endoscopy and fluoroscopy were used to follow stent deployment. Immediately after the procedure, an upright abdominal X-ray was performed to assess that no perforation had occurred during the procedure.
Follow-up information
Food intake was measured by the standardized gastric outlet obstruction scoring system (GOOSS score), with 1 = no oral intake, 2 = liquids only, 3 = soft solids, and 4 = full diet [2]. The GOOSS score was measured before and 1 week after stent placement. Based on this score, clinical success was defined as relief of symptoms and improvement of oral intake until at least soft solids (GOOSS = 3) 1 week after the procedure. Technical success of stent placement was defined as adequate positioning and deployment of the stent with complete bridging of the stenosis.
Complications included life-threatening or severe complications, for example, perforation and stent migration. Persistent obstructive symptoms were defined as continuing obstructive symptoms occurring within 2 weeks after the intervention, whereas recurrent obstructive symptoms were defined as symptoms occurring more than 2 weeks after treatment. A reintervention was defined as a treatment for a complication, or persistent or recurrent obstructive symptoms.
Statistics
The GOOSS score before and 1 week after stent placement was compared with the Wilcoxon rank sum test. Survival was calculated by Kaplan–Meier analysis. Calculations were performed with SPSS 12.0. A two-sided p-value < 0.05 was considered statistically significant.
Results
Patient characteristics
In the period 2001–2006, enteral Wallstents (Boston Scientific, Natick, MA) (n = 12) or Wallflex stents (Boston Scientific) (n = 4) were placed using a colonoscope in 16 patients (11 men, 5 women). Table 1 shows the baseline characteristics of these patients (mean age: 70.1 ± 9.4 years). Obstruction was caused by pancreatic cancer (n = 8), duodenal cancer (n = 2), colorectal cancer (n = 2), lymphoma (n = 1), and metastases from renal cell (n = 1), lung (n = 1), and liver cancer (n = 1). Sites of obstruction were the second half of the horizontal and ascending part of the duodenum (n = 10), duodenojejunal flexure (n = 5), and proximal jejunum (n = 1). Main study outcomes are shown in Table 2.
Technical success
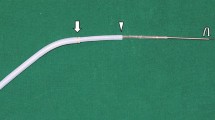
In nine patients, initial stent placement using a gastroscope was unsuccessful. In all these patients a GIF-1T145 gastroscope (Olympus America Inc., Center Valley, PA, USA) had been used. Therefore, this endoscope was changed for a colonoscope (CF0165 or CF0180 colonoscope (Olympus Japan Inc.). In the following seven patients, we primarily used a colonoscope (CF0165 or CF0180 colonoscope (Olympus Japan Inc.). Stent placement with a colonoscope was technically feasible in 93% (15/16) of patients (Fig. 1; video). In one patient, persistent obstructive symptoms were present after the procedure. It was found that the primary stent had not completely bridged the tumor. In this patient, a second stent was placed 1 day later.
Food intake
Food intake improved in all patients [improvement of median GOOSS score from 1 (before stent placement) to 3 (1 week after) (p = 0.001)]. One patient was only able to drink liquids 1 week after stent placement (GOOSS score: 2). Clinical success was therefore considered to be 94% (15/16).
Complications
Severe complications were not observed during the follow-up period. Recurrent obstructive symptoms occurred in seven patients after a median of 240 days (range 13 to 270 days) due to tissue/tumor ingrowth (n = 7) and stent occlusion by debris (n = 1). One patient suffered tumor ingrowth twice, 92 days and 242 days after initial stent placement.
Persistence of obstructive symptoms occurred in one patient with motility problems. This patient refused additional treatment and died 18 days after stent placement from progressive tumor growth.
Reinterventions were only performed for recurrent obstructive symptoms and included stent placement (n = 5), gastrojejunostomy (n = 2), and endoscopic cleansing of the stent (n = 1). Subsequent gastrojejunostomy was performed in two patients with tumor overgrowth because a second stent could not be placed.
Survival
The 30-day mortality rate was 25% (4/16). Median survival was 153 days, with four patients still being alive at the end of our follow-up period (January 1, 2007).
Discussion
The results of this study show that distal duodenal/proximal jejunal stent placement using a colonoscope is safe and effective. It was demonstrated that a colonoscope was a good alternative for a gastroscope in this situation.
In the first nine patients, stent placement was initially performed with a gastroscope. However, stent placement failed because of looping of the gastroscope in the stomach resulting in inability of the endoscope to reach the malignant stricture. For that reason, the gastroscope was changed for a colonoscope.
In our experience, when a therapeutic gastroscope is used for stent placement in the distal part of the duodenum or proximal jejunum, three potential problems may occur. First, the length of the gastroscope may be insufficient because of looping in the stomach. Looping is more likely to occur if the stomach and proximal duodenum are dilated particularly if the stricture in the duodenum/jejunum has existed for a prolonged period of time. Second, when looping occurs, the resulting friction between the stent and the working channel of the endoscope may prevent the stent from being advanced out of the endoscope. Third, even when the stent can be advanced close to an often angulated stricture, the ability to maintain the gastroscope in a stationary position in the duodenum is reduced. The resistance offered by an angulated stricture may result in a retrograde force pushing the gastroscope back into the stomach, even if a super-stiff guidewire is advanced through the endoscope. The colonoscope is obviously longer, provides more stiffness in these cases, and avoids looping in the stomach, resulting in a stable position close to a stricture distal in the duodenum and proximal jejunum. In addition, Ross et al. reported the use of double balloon enteroscopy in combination with a colonoscope. The technical advantages of this technique may allow endoscopic stent placement in patients with a single point of obstruction that is beyond the reach of conventional endoscopes and existing stent delivery systems [12]. In our opinion, a newly designed endoscope with specifications for duodenal stent placement should provide the following features: (1) a large working channel, which makes stent placement over the guidewire possible, (2) adequate stiffness of the endoscope without increasing the diameter, and (3) sufficient length of the endoscope to reach distal strictures.
To the best of our knowledge, stent placement for obstructions in the distal duodenum or proximal jejunum using a colonoscope has not previously been reported, although Baron et al. already mentioned the usefulness of this technique [13]. We compared our results with those summarized in a recent systematic review summarizing stent placement for malignant strictures in the distal stomach or proximal duodenum [14]. Results on food intake, technical success, complications, and persistent symptoms were not different. However, mean survival after stent placement was longer in our study population (184 versus 85 days). This difference may result from differences in clinical condition. Unfortunately, this was not clearly stated in the medical records and is therefore unknown. In addition, recurrent obstructive symptoms appeared to have occurred more frequently in our patient population (44% versus 22%), most often due to tissue/tumor ingrowth. This can probably be explained by the fact that Dormann et al. included results of both uncovered and covered stents [14]. Remarkably, 13% (80/606) patients in this review were treated with a covered esophageal stent placed in the distal stomach/proximal jejunum. A clear drawback of uncovered stents in the duodenum is the occurrence of hyperplastic tissue or tumor growth through the mesh of the stent [15–17]. In the present study, we only used uncovered stents, whereas a second uncovered stent for tissue or tumor ingrowth was performed for six occluded stents in five patients. The use of covered stents in the duodenum may overcome this problem of tissue/tumor ingrowth. The evidence for the safe use of covered stents in the duodenum is however conflicting in that, on the one hand, this design may prevent tissue or tumor ingrowth, but, on the other hand, covered stents are more likely to migrate than uncovered stents [6, 18]. In addition, the longer survival in our patient series compared to that in the review by Dorman et al. may also have resulted in a higher incidence of recurrent obstructive symptoms. In this regard, it is important to emphasize that patients with a good prognosis could potentially gain more benefit from a laparoscopic gastrojejunostomy as this palliative treatment has been suggested to be associated with a lower incidence of recurrent obstructive symptoms compared to stent placement [19]. If one has to decide on the most optimal treatment option, it could well be that patients with a poor clinical condition may gain more benefit from stent placement, whereas gastrojejunostomy should be reserved for those with an expected longer survival. Nevertheless, a large randomized trial has not been performed yet.
Finally, stent placement in the distal duodenum has the advantage that malignant biliary obstruction occurring after duodenal stent placement is not precluding the possibility to perform biliary drainage by endoscopic retrograde cholangiopancreatography (ERCP) at a later time point. Biliary obstruction occurs in 2–8 % of patients after stent placement in the proximal duodenum [1, 2, 20, 21]. It is often difficult or even impossible to cannulate the papilla through the mesh of an uncovered stent. Therefore, in many centers, prior to stent placement in the proximal duodenum, a stent is placed in the common bile duct [22].
Our results indicate that duodenal stent placement can effectively and safely be performed using a colonoscope in patients with an obstruction at the level of the distal duodenum or proximal jejunum. A colonoscope has the advantage that it is long enough and offers good endoscopic stiffness, which avoids looping in the stomach.
References
Espinel J, Vivas S, Munoz F, Jorquera F, Olcoz JL (2001) Palliative treatment of malignant obstruction of gastric outlet using an endoscopically placed enteral Wallstent. Dig Dis Sci 46:2322–2324
Adler DG, Baron TH (2002) Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol 97:72–78
Lopera JE, Brazzini A, Gonzales A, Castaneda-Zuniga WR (2004) Gastroduodenal stent placement: current status. Radiographics 24:1561–1573
Del Piano M, Ballare M, Montino F, Todesco A, Orsello M, Magnani C, Garello E (2005) Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc 61:421–426
Pinto PI, Diaz LP, Ruiz De Adana JC, Lopez HJ (2001) Gastric and duodenal stents: follow-up and complications. Cardiovasc Intervent Radiol 24:147–153
Park KB, Do YS, Kang WK, Choo SW, Han YH, Suh SW, Lee SJ, Park KS, Choo IW (2001) Malignant obstruction of gastric outlet and duodenum: palliation with flexible covered metallic stents. Radiology 219:679–683
Mehta S, Hindmarsh A, Cheong E, Cockburn J, Saada J, Tighe R, Lewis MP, Rhodes M (2006) Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg Endosc 20:239–242
Fiori E, Lamazza A, Volpino P, Burza A, Paparelli C, Cavallaro G, Schillaci A, Cangemi V (2004) Palliative management of malignant antro-pyloric strictures. Gastroenterostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res 24:269–271
Yates MR III, Morgan DE, Baron TH (1998) Palliation of malignant gastric and small intestinal strictures with self-expandable metal stents. Endoscopy 30:266–272
Song HY, Shin JH, Yoon CJ, Lee GH, Kim TW, Lee SK, Yook JH, Kim BS (2004) A dual expandable nitinol stent: experience in 102 patients with malignant gastroduodenal strictures. J Vasc Interv Radiol 15:1443–1449
Lee JM, Han YM, Lee SY, Kim CS, Yang DH, Lee SO (2001) Palliation of postoperative gastrointestinal anastomotic malignant strictures with flexible covered metallic stents: preliminary results. Cardiovasc Intervent Radiol 24:25–30
Ross AS, Semrad C, Waxman I, Dye C (2006) Enteral stent placement by double balloon enteroscopy for palliation of malignant small bowel obstruction. Gastrointest Endosc 64:835–837
Baron TH, Harewood GC (2003) Enteral self-expandable stents. Gastrointest Endosc 58:421–433
Dormann A, Meisner S, Verin N, Wenk LA (2004) Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy 36:543–550
Kim GH, Kang DH, Lee DH, Heo J, Song GA, Cho M, Yang US (2004) Which types of stent, uncovered or covered, should be used in gastric outlet obstructions? Scand J Gastroenterol 39:1010–1014
Nevitt AW, Vida F, Kozarek RA, Traverso LW, Raltz SL (1998) Expandable metallic prostheses for malignant obstructions of gastric outlet and proximal small bowel. Gastrointest Endosc 47:271–276
Bethge N, Breitkreutz C, Vakil N (1998) Metal stents for the palliation of inoperable upper gastrointestinal stenoses. Am J Gastroenterol 93:643–645
Jung GS, Song HY, Kang SG, Huh JD, Park SJ, Koo JY, Cho YD (2000) Malignant gastroduodenal obstructions: treatment by means of a covered expandable metallic stent-initial experience. Radiology 216:758–763
Jeurnink SM, Steyerberg EW, Hof G, van Eijck CH, Kuipers EJ, Siersema PD (2007) Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol 96:389–396
Maetani I, Akatsuka S, Ikeda M, Tada T, Ukita T, Nakamura Y, Nagao J, Sakai Y (2005) Self-expandable metallic stent placement for palliation in gastric outlet obstructions caused by gastric cancer: a comparison with surgical gastrojejunostomy. J Gastroenterol 40:932–937
Telford JJ, Carr-Locke DL, Baron TH, Tringali A, Parsons WG, Gabbrielli A, Costamagna G (2004) Palliation of patients with malignant gastric outlet obstruction with the enteral Wallstent: outcomes from a multicenter study. Gastrointest Endosc 60:916–920
Laasch HU, Martin DF, Maetani I (2005) Enteral stents in the gastric outlet and duodenum. Endoscopy 37:74–81
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jeurnink, S.M., Repici, A., Luigiano, C. et al. Use of a colonoscope for distal duodenal stent placement in patients with malignant obstruction. Surg Endosc 23, 562–567 (2009). https://doi.org/10.1007/s00464-008-9880-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9880-5