Abstract
Background
In laparoscopic hernia repair the use of biocompatible materials is necessary. A prospective, double-blind study was projected to compare three different meshes.
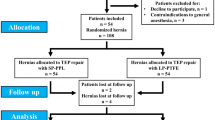
Methods
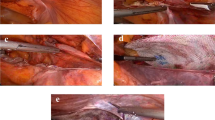
Ninety male patients with primary inguinal hernia undergoing transabdominal preperitoneal (TAPP) implant procedures were included. Three different types of mesh were tested: a monofile, heavy-weight, rigid mesh (group A), a smooth, heavy-weight variant of polypropylene (group B), and a polyglactin/polypropylene compound mesh (group C). Complications, pain development, inability to work, physical conditions, testicular volume, and blood circulation were documented.
Results
Convalescence in group A was slower than in groups B and C: Postoperative values of visual scales for pain development were higher, inability to work was 7.3 days longer, urologic effects were more severe, activities of everyday life were more reduced, and data of the German SF-36 Health Survey Test showed a significant reduction of physical condition (p < 0.05).
Conclusion
The compound mesh did not create more comfort for the patients than the smooth variant of the heavy-weight polypropylene mesh.




Similar content being viewed by others
References
Batorfi J, Kelemen O, Vizsy L, Simon E, Balint A, Posfai G (1997) Transabdominal preperitoneal herniorraphy: technique and results. Acta Chir Hung 36(1–4): 18–21
Bittner R, Leibl B, Kraft K (1997) Laparoscopic hernia repair: prevention and therapy of complications. Langenbecks Arch Chir Suppl Kongressbd 114: 935–938
Bittner R, Leibl B, Kraft K, Daubler P, Schwarz J (1996) Laparoscopic hernioplasty (TAPP)—complications and recurrences in 900 operations. Zentralbl Chir 121(4): 313–319
Bittner R, Schmedt CG, Schwarz J, Kraft K, Leibl BJ (2002) Laparoscopic transperitoneal procedure for routine repair of groin hernia. Br J Surg 89: 1062
Champault G, Barrat C (2004) Inguinal hernia repair with beta glucan-coated mesh: results at two-year follow up. Hernia Dec 16 [Epub ahead of print]
EU Hernia Trialists Collaboration (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg; 87: 854
Felix EL, Habertson N, Vartanian S (1999) Laparoscopic hernioplasty. Significant complications. Surg Endosc 13(4): 328–331
Kingsnorth A (2004). Treating inguinal hernias. Br Med J 328: 59–60
Klinge U, Conze J, Limberg W, Brucker C, Ottinger AP, Schumpelick V (1996) Pathophysiologie der Bauchdecken. Chirurg 67: 229
Klinge U, Junge K, Stumpf M, Öttinger AP, Klosterhalfen B (2002) Functional and morphological evaluation of a low-weight, monofilament polypropylene mesh for hernia repair. J Biomed Mater Res 63: 129–136
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski C, Ottinger AP, Schumpelick V (1998). Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164: 951
Klosterhalfen B, Klinge U, Hermanns B, Schumpelick V (2000) Pathology of traditional surgical nets for hernia repair after long-term implantation in humans. Chirurg 71(1): 43–51
Klosterhalfen B, Klinge U, Schumpelick V (1998) Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials 19(24): 2235–2246
Schardey HM, Schopf S, Rudert W, Knappich P, Hernandez-Richter T (2004) Titanised polypropylene meshes: first clinical experience with the implantation in TAPP technique and the results of a survey in 22 German surgical departments. Zentralbl Chir 129(5): 363–368
Schumpelick V, Klinge U, Welty G, Klosterhalfen B (2000) Meshes in der Bauchwand. Chirurg 70: 876–887
Suzer O, Ozcan H, Kupeli S, Gheiler EL (1997) Color Doppler imaging in the diagnosis of the acute scrotum. Eur Urol 32(4): 457–461
Wantz GE (1996) Experience with the tension-free hernioplasty for primary inguinal hernias in men. J Am Coll Surg 183(4): 351–356
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Langenbach, M.R., Schmidt, J. & Zirngibl, H. Comparison of biomaterials: three meshes and TAPP for inguinal hernia. Surg Endosc 20, 1511–1517 (2006). https://doi.org/10.1007/s00464-005-0078-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0078-9