Abstract
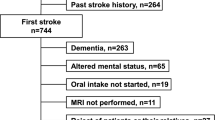
Dysphagia affects up to half of stroke patients and increases the risk of pneumonia and fatal outcomes. In order to assess swallowing difficulty, videofluoroscopic swallowing study (VFSS) has traditionally been the gold standard. The purpose of this study was to compare the patterns of post-stroke swallowing difficulties according to the vascular territories involved in the stroke. One hundred and three patients who were diagnosed with first ischemic stroke by brain magnetic resonance imaging and had swallowing difficulty were included in this study. Location of the stroke was classified into three groups: territorial anterior infarcts (TAI) (n = 62), territorial posterior infarcts (TPI) (n = 19) and white matter disease (WMD) (n = 22). Oral cavity residue existed significantly in the TAI group more than in any other groups (P = 0.017). The WMD group showed more residue in the valleculae (P = 0.002) and the TPI group showed more residue in the pyriform sinuses (P = 0.001). The oral transit time, pharyngeal delay time and pharyngeal transit time did not show significant differences among the groups with swallowing of both thick and thin liquids. Penetration and aspiration were more frequent in the TPI group (P < 0.05) with swallowing of both thick and thin liquids. The results suggest that TAI is more related to oral phase dysfunction and TPI is more related to pharyngeal dysfunction. In ischemic stroke, patterns of swallowing difficulty may differ according to the vascular territory involved and this should be considered in the management of post-stroke dysphagia.
Similar content being viewed by others
References
Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383–91.
Holas M, Depippo K, Reding M. Aspiration and relative risk of medical complications following stroke. Arch Neurol. 1994;51:1051–3.
Kidd D, Lawson J, Nesbitt R. The natural history and clinical consequences of aspiration in acute stroke. QJM. 1995;88:409–13.
Katzan I, Cebul R, Husak S, Dawson N, Baker D. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60:620–5.
Smithard D, O’Neill P, Park C, Morris J. Complications and outcome after acute stroke: does dysphagia matter? Stroke. 1996;27:1200–4.
Han T, Paik N, Park J. The functional dysphagia scale using videofluoroscopic swallowing study in stroke patients. J Korean Acad Rehab Med. 1999;23:1118–26.
Horner J, Massey E. Silent aspiration following stroke. Neurology. 1988;38:317–9.
Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, Silvestrelli G, Parlmerini F, Parnetti L, Gallai V. Dysphagia following stroke. Eur Neurol. 2004;51:162–7.
Terre R, Mearin F. Oropharyngeal dysphagia after the acute phase of stroke: predictors of aspiration. Neurogastroenterol Motil. 2006;18:200–5.
Robbins J, Levine R, Maser A, Rosenbek J, Kempster G. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74:1295–300.
Daniels S, Brailey K, Foundas A. Lingual discoordination and dysphagia following acute stroke: analyses of lesion localization. Dysphagia. 1999;14:85–92.
Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009;40:1903–6.
Rovira A, Grive E, Rovira A, Alvarez S. Distribution territories and causative mechanisms of ischemic stroke. Eur Radiol. 2005;15:416–26.
Logemann J. Evaluation and treatment of swallowing disorders. 2nd ed. Texas: PRO-ED; 1998.
Jang Y, Lee S, Jeon J, Lee S. Analysis of videofluoroscopic swallowing study in patients with vocal cord paralysis. Dysphagia. 2012;27:185–90.
Kim M, Lee S, Kim T, Seo D, Hyun J, Kim J. The influence of laterality of pharyngeal bolus passage on dysphagia in hemiplegic stroke patients. Ann Rehabil Med. 2012;36:696–701.
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337:1521–6.
Adams H, Bendixen B, Kappelle L, Biller J, Love B, Gordon D, March E. Classification of subtype of acute ischemic stroke. Stroke. 1993;24:35–41.
Lee C, Kim J. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehab Med. 2001;25:193–201.
Han D, Chang Y, Lu C, Wang T. Comparison of disordered swallowing patterns in patients with recurrent cortical/subcortical stroke and first-time brainstem stroke. J Rehabil Med. 2005;37:189–91.
Moon H, Pyun S, Kwon H. Correlation between location of brain lesion and cognitive function and findings of videofluoroscopic swallowing study. Ann Rehabil Med. 2012;36:347–55.
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–35.
Sundar U, Pahuja V, Dwivedi N, Yeolekar M. Dysphagia in acute stroke: correlation with stroke subtype, vascular territory and in-hospital respiratory morbidity and mortality. Neurol India. 2008;56:463–70.
Alberts M, Horner J, Gray L, Brazer S. Aspiration after stroke: lesion analysis by brain MRI. Dysphagia. 1992;7:170–3.
Mohr J, Scharler J. Meddle cerebral artery territory syndromes. In: Caplan L, Gijn J, editors. Stroke syndromes. 3rd ed. New York: Cambridge; 2012. p. 334.
Acknowledgments
The present research was conducted by the research fund of Dankook University in 2012.
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.Y., Kim, T.U., Hyun, J.K. et al. Differences in Videofluoroscopic Swallowing Study (VFSS) Findings According to the Vascular Territory Involved in Stroke. Dysphagia 29, 444–449 (2014). https://doi.org/10.1007/s00455-014-9525-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-014-9525-x