Abstract
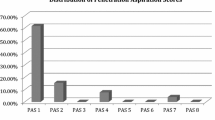
The aim of this study was to examine the impact of gabapentin (neurontin) on swallowing and feeding tube use during chemoradiation (CRT) for oropharyngeal squamous cell carcinoma (OPSCC), and physiologic swallowing outcomes following completion of treatment. A total of 23 patients treated for OPSCC with concurrent CRT and prophylactically treated for pain using gabapentin were assessed. Historical controls were matched for T stage and primary site of disease. Timing of PEG use and removal were recorded. Video fluoroscopic swallowing studies were completed post-treatment to assess physiologic outcomes as well as penetration–aspiration scores (PAS). Functional oral intake scale (FOIS) scores were determined at the time of swallowing evaluation to assess diet level. Patients treated with gabapentin began using their PEG tubes later (3.7 vs. 2.29 weeks; P = 0.013) and had their PEG tubes removed earlier (7.29 vs. 32.56 weeks; P = 0.039) than the historical controls. A number of physiologic parameters were found to be less impacted in the gabapentin group, including oral bolus control (P = 0.01), epiglottic tilt (P = 0.0007), laryngeal elevation (P = 0.0017), and pharyngeal constriction (P = 0.002). PAS scores were significantly lower in the group treated with gabapentin (1.89 vs. 4; P = 0.0052). Patients receiving gabapentin had more advanced diet levels at the time of the initial swallowing study as evidenced by their FOIS scores (5.4 vs. 3.21; P = 0.0003). We conclude that patients using gabapentin for pain management during CRT appears to do well maintaining swallow function during treatment and have favorable post-treatment physiologic swallowing outcomes. Prospective evaluation is warranted.






Similar content being viewed by others
References
Department of Veterans Affairs Laryngeal Cancer Study Group. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med. 1991;324(24):1685–90.
Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349(22):2091–8.
Gillespie M, Brodsky MB, Day TA, Sharma AK, Lee F, Martin-Harris B. Laryngeal penetration and aspiration during swallowing after the treatment of advanced oropharyngeal cancer. Arch Otorhinolaryngol Head Neck Surg. 2005;131:615–9.
Elting LS, Keefe DM, Sonis ST, et al. Patient-reported measurements of oral mucositis in head and neck cancer patients treated with radiotherapy with or without chemotherapy: demonstration of increased frequency, severity, resistance to palliation, and impact on quality of life. Cancer. 2008;113(10):2704–13.
Trotti A, Bellm LA, Epstein JB, et al. Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systematic literature review. Radiother Oncol. 2003;66(3):253–62.
Murphy BA, Beaumont JL, Isitt J, et al. Mucositis-related morbidity and resource utilization in head and neck cancer patients receiving radiation therapy with or without chemotherapy. J Pain Symptom Manage. 2009;38(4):522–32.
Langmore S, Krisciunas GP, Miloro KV, et al. Does PEG use cause dysphagia in head and neck cancer patients? Dysphagia. 2012;27(2):251–9.
Kotz T, Costello R, Li Y, Posner MR. Swallowing dysfunction after chemoradiation for advanced squamous cell carcinoma of the head and neck. Head Neck. 2004;26(4):365–72.
Graner DE, Foote RL, Kasperbauer JL, et al. Swallow function in patients before and after intra-arterial chemoradiation. Laryngoscope. 2003;113(3):573–9.
Lazarus C. Tongue strength and exercise in healthy individuals and head and neck cancer patients. Semin Speech Lang. 2006;27(4):260–7.
Starmer H, Gourin C, Lua LL, Burkhead L. Pretreatment swallowing assessment in head and neck cancer patients. Laryngoscope. 2011;121(6):1208–11.
Maneuf YP, Luo ZD, Lee K. α2δ and the mechanism of action of gabapentin in the treatment of pain. Semin Cell Dev Biol. 2006;17:565–70.
Luo ZD, Chaplan SR, Higuera ES, et al. Upregulation of dorsal root ganglion α2δ calcium channel subunit and its correlation with allodynia in spinal nerve-injured rats. J Neurosci. 2001;21:1868–75.
Li CY, Song YH, Higuera ES, et al. Spinal dorsal horn calcium channel α2δ-1 subunit upregulation contributes to peripheral nerve injury-induced tactile allodynia. J Neurosci. 2004;24:8494–9.
Boroujerdi A, Kim HK, Lyu YS, et al. Injury discharges regulate calcium channel alpha-2-delta-1 subunit upregulation in the dorsal horn that contributes to initiation of neuropathic pain. Pain. 2008;139:358–66.
Luo Z, Calcutt N, Higuera E, et al. Injury type-specific calcium channel alpha 2 delta-1 subunit up-regulation in rat neuropathic pain models correlates with antiallodynic effects of gabapentin. J Pharmacol Exp Ther. 2002;303:1199–205.
Bar Ad V, Weinstein G, Dutta PR, et al. Gabapentin for the treatment of pain related to radiation-induced mucositis in patients with head and neck tumors treated with intensity-modulated radiation therapy. Head Neck. 2010;32:173–7.
Bar Ad V, Weinstein G, Dutta PR, et al. Gabapentin for the treatment of pain syndrome related to radiation-induced mucositis in patients with head and neck cancer treated with concurrent chemoradiotherapy. Cancer. 2010;116:4206–13.
Rosenbek J, Robbins J, Roecker E, Coyle J, Wood J. A penetration aspiration scale. Dysphagia. 1996;11(2):93–8.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20.
Epstein JB, Wilkie DJ, Fisher DJ, et al. Neuropathic and nociceptive pain in head and neck cancer patients receiving radiation therapy. Head Neck Oncol. 2009;1:26.
Carnaby-Mann G, Crary MA, Schmalfuss I, Amdur R. “Pharyngocise”: randomized controlled trial of preventative exercises to maintain muscle structure and swallowing function during head and neck chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83(1):210–9.
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Starmer, H.M., Yang, W., Raval, R. et al. Effect of Gabapentin on Swallowing During and After Chemoradiation for Oropharyngeal Squamous Cell Cancer. Dysphagia 29, 396–402 (2014). https://doi.org/10.1007/s00455-014-9521-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-014-9521-1