Abstract
Purpose
The Kirsten rat sarcoma viral oncogene (KRAS) is the most frequently mutated oncogene in human cancers. Significant advancements have been made in targeted therapy and immunotherapy for this gene in recent years, underscoring the importance of comprehensively understanding the genomic landscape of KRAS across various cancer types.
Methods
Using next-generation sequencing (NGS) technology and a panel of 520 genes, KRAS mutations, tumor mutation burden (TMB), and microsatellite instability (MSI-H) status were investigated.
Results
An analysis of 10,820 tumor samples found KRAS mutations in 19.97% of cases. Pancreatic cancer showed the highest prevalence of KRAS mutations at 73.51%, while colorectal at 41.45%, uterine at 21.23%, and lung cancer at 11.24%. KRAS G12D mutation is most common in pancreatic, colorectal, and gastric cancers, while KRAS G12V mutation is predominant in uterine cancer, and KRAS G12C mutation is most frequent in lung cancer. Significant correlations were found between TMB and KRAS G13D/G12V mutations in colorectal cancer. KRAS G13D notably affected TMB in uterus cancer, while KRAS G12C mutation was linked to high TMB in lung cancer. Moreover, statistical analysis revealed a significant association between KRAS G13D/G12V mutations and MSI-H in colorectal cancer.
Conclusions
KRAS mutations were most frequent in cancers of the digestive, female reproductive, and respiratory systems. Specific KRAS mutations are associated with TMB and MSI in various cancer types.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
RAS gene was the first human oncogene identified (Stephen et al. 2014), comprising three principal subtypes: KRAS, HRAS, and NRAS. Research indicates that mutations in the RAS gene are implicated in 30% of all cancers, with KRAS mutations representing 85% of these RAS mutations (Hunter et al. 2015). KRAS functions as a critical downstream signaling molecule within the epidermal growth factor receptor (EGFR) signal transduction pathway. Activating mutations in the KRAS gene are implicated in both tumorigenesis and the aggressive proliferation of tumors. As a result, KRAS is considered the most promising target for cancer therapy. KRAS mutations are notably prevalent in many types of cancers, including pancreatic cancer, colorectal cancer, and non-small cell lung cancer (Cazzanelli et al. 2018). Moreover, mutation subtypes varied widely across different locations and tumor types. The most frequently observed mutation sites in KRAS are predominantly located on exon 2, including G12C, G12V, G12D and other (Kulkarni et al. 2022). However, the differential expression of different KRAS mutant isoforms in pan-cancer of Chinese patients has not yet been reported.
In recent years, targeted drugs for KRAS G12C mutations, such as Sotolasib, have achieved good efficacy in clinical trials (Nakajima et al. 2022). Moreover, G12D mutation has been identified as a clinical candidate. Recent identification of a non-covalent small molecule inhibitor (MRTX1133) with specificity to the KRAS G12D mutant protein has offered an opportunity to evaluate its efficacy directly on KRAS cancer cells (Hallin et al. 2022; Kemp et al. 2023). Consequently, the targeting of KRAS mutations represents a promising strategy for the treatment of various cancer types, with significant implications for the development of new cancer therapies. KRAS mutation also exhibits a broad impact on the tumor microenvironment, and many studies have been carried out investigating the effects of KRAS mutations on immunotherapy (Kim et al. 2017). Nevertheless, there is a paucity of comprehensive and robust data pertaining to the impact of KRAS mutations on the tumor microenvironment and the efficacy of immunotherapy across a range of cancers.
Here, we performed a comprehensive pan-cancer genomic analysis to identify the incidence of KRAS alterations across 16 tumor types in 10,820 Chinese patients. We also analyzed the genomic co-alteration landscapes and immune biomarker profiles associated with various KRAS mutations, focusing on tumor mutational burden (TMB), microsatellite instability (MSI), and mutational signatures. This research delineates the landscape of tumors harboring KRAS mutations, aiming to furnish critical insights for the design and implementation of clinical trials targeting patients with KRAS-mutant tumors in China.
Methods
Patients and data source
The study involved the collection of data from 10,820 patients diagnosed with malignant tumors at the Cancer Hospital Chinese Academy of Medical Sciences (CHCAMS) between 2019 and 2024. The tumor types included those of the digestive system, respiratory system, female reproductive system, head and neck, urinary system, soft tissue, nervous system, and bone system. All patients received hybrid-capture-based next-generation sequencing (NGS) testing after obtaining written informed consent. The NGS data included in this study have been subjected to a rigorous review process by the CHCAMS Ethics Committee, and ethical approval has been granted (NCC2694). The study was conducted in accordance with the ethical principles set forth in the Declaration of Helsinki for research involving human subjects. Prior to participation, all subjects were required to sign an informed consent form, which provided detailed information about the purpose of the experiment, the methods to be employed, the potential risks, the expected benefits, and the subjects’ rights. The Cancer Genome Program (TCGA) of KRAS mutations-related research data is available from the biological portal platform (https://www.cbioportal.org) (Gao et al. 2013).
NGS
All specimens were initially preserved in standard formalin and subsequently embedded in paraffin. Post-pathological assessment, samples demonstrating a tumor cell content exceeding 20% were selected for further analysis. The paraffin-embedded blocks were sectioned, and genomic DNA was extracted using the QIAamp DNA FFPE Tissue Kit from Qiagen. NGS was employed to analyze critical tumor-associated genes through a targeted NGS approach based on hybrid capture. Furthermore, the microsatellite status and TMB of each tumor were evaluated. The experimental protocol for NGS was executed as follows: Initially, genomic DNA was fragmented utilizing an ultrasonic disruptor. Subsequently, both termini of the fragmented DNA were amplified through polymerase chain reaction (PCR). The resulting PCR products underwent purification using 75% ethanol, followed by probe capture and additional purification via PCR to construct sequencing libraries. These labeled libraries were then adjusted to the requisite concentration and combined. Variants exhibiting a mutation abundance exceeding 5% were identified as positive using the NextSeq N550 platform (Illumina, San Diego, CA). TMB was quantified by enumerating the non-driver synonymous and non-synonymous mutations within a genomic region spanning 0.8–1.2 megabases (Mb), incorporating computational filtering for germline status, and expressing the results as mutations per megabase. This approach has been previously validated for accuracy in comparison to whole exome sequencing (Chalmers et al. 2017). MSI was assessed by examining intronic homopolymer repeat loci for length variability, with the data subsequently synthesized into a comprehensive MSI score using principal component analysis (Trabucco et al. 2019).
Statistical analysis
The data were analyzed and processed using SPSS version 22.0 and GraphPad Prism version 6.0 (GraphPad Software, La Jolla, CA, USA). The chi-square (χ2) test was utilized to investigate the association between KRAS gene mutations and the clinical and molecular pathological characteristics of the patients. For binary outcomes, polytomous regression was reduced to binary logistic regression. Statistical significance was determined by a two-sided p-value of less than 0.05.
Results
KRAS mutations in various tumors
In this study, a cohort of 10,820 patients diagnosed with malignant tumors was enrolled, consisting of 6724 male and 4096 female participants, covering malignancies of the colorectal, gastric, pancreatic, esophageal, biliary tract, and pulmonary systems, among others. KRAS mutations were identified in 2161 out of the 10,820 tumor samples analyzed (19.97%). The prevalence of KRAS mutations exhibited variability among different cancer types, with the highest frequency observed in tumors of the digestive system (1477 out of 4255 cases, 34.71%), followed by tumors of the female reproductive system (146 out of 982 cases, 14.87%). Furthermore, the frequency of KRAS mutations was 11.24% (481 out of 4278 cases) in respiratory tumors, 10.99% (20 out of 182 cases) in soft tissue tumors, and 7.87% (7 out of 89 cases) in bone tumors. In urological tumors, the frequency was 4.19% (9 out of 215 cases), while it was 4.04% (4 out of 99 cases) in neurological tumors, 2.57% (17 out of 662 cases) in head and neck tumors, and 0% (0 out of 58 cases) in breast cancer. The prevalence of KRAS mutations varies among different tumor types, with the highest incidence observed in pancreatic cancer (73.51%), followed by colorectal cancer (41.45%), uterine cancer (21.23%), biliary tract cancer (14.56%), lung cancer (11.24%), gastric cancer (8.57%), thyroid cancer (7.41%), ovarian cancer (5.43%) (Table 1).
For analytical purposes, only those cancer types that had been observed in more than 50 cases with a KRAS mutation were considered. And then, this epidemiological distribution was compared with data from the TCGA database. The incidence of KRAS mutations was found to be higher in the Chinese NCCN patient cohort compared to the general TCGA population for PAAD (73.51% vs. 63.59%, p = 0.126), COADREAD (41.45% vs. 36.70%, p = 0.562), UCEC (21.23% vs. 17.62%, p = 0.592), and CHOL (14.56% vs. 17.62%, p = 0.038). Conversely, the incidence was lower in patients with LUAD (14.10% vs. 30.05%, p = 0.000) (Figure 1).
KRAS subtypes in diverse cancers
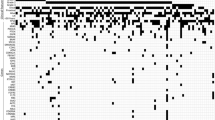
In pancreatic cancer and colorectal cancer, the G12D mutation was the most common, found in 34.23% and 13.37% of cases, respectively. Uterine cancer predominantly exhibited the G12D and G12V mutations, each accounting for 6.30% of cancer. In contrast, the G12C mutation was most frequently observed in lung cancer, representing 3.37% of cancer. Gastric cancer primarily exhibited the G12D mutation (2.86%) (Fig. 2A). An analysis of KRAS mutations subtypes reveals that the KRAS G12D mutation is the most prevalent in pancreatic, colorectal, and gastric cancers. In contrast, the KRAS G12V mutation predominates in uterine cancer, while KRAS G12C mutation is the most frequent mutation in lung cancer. Specifically, in pancreatic cancer, the KRAS G12D mutation was identified in 46.5% (115 out of 247) of KRAS mutations, followed by KRAS G12V mutation in 31.6% (78 out of 247), and KRAS G12R mutation in 12.5% (31 out of 247) (Fig. 2B). In colorectal cancer, the distribution of KRAS mutations was as follows: G12D mutation in 32.3% (372 out of 1153), G13D mutation in 18.9% (218 out of 1153), G12V mutation in 17.3% (200 out of 1153), and G12C mutation in 6.5% (75 out of 1153) (Fig. 2C). In uterine cancer, the prevalence of KRAS mutations was as follows: G12V mutation and G12D mutations were each present in 29.7% (38 out of 128 cases), G13D mutation in 14.1% (18 out of 128 cases), and G12A mutation in 7.8% (10 out of 128 cases) (Fig. 2D). In lung cancer, the distribution of KRAS mutations was observed as follows: G12C mutation in 29.9% (144 out of 481 cases), G12D mutation in 22.4% (108 out of 481 cases), G12V mutation in 18.9% (91 out of 481 cases), and G12A mutation in 7.3% (35 out of 481 cases) (Fig. 2E). In gastric cancer, KRAS mutations were identified as G12D mutation in 33.3% (20 out of 60 cases), G13D mutation in 28.3% (17 out of 60 cases), and G12V mutation in 10% (6 out of 60 cases) (Fig. 2F).
Distribution of KRAS mutations in all tumors and seven subtypes. A Proportional distribution of different mutation subtypes in tumors. Distribution and proportion of KRAS mutation subtypes in pancreatic cancers (B), colorectal cancers (C), uterine cancers (D), lung cancers (E) and gastric cancers (F), respectively
Association of TMB with KRAS mutations
The TMB values of each tumor were assessed through NGS during the identification of driver gene mutations. A TMB of 10 mutations per megabase (mut/Mb) was categorized as high TMB (TMB-H). TMB values demonstrated variability across different malignancies, with TMB-H being most prevalent in gastric cancer (37%, 22 out of 60 cases), followed by uterine cancer (25%, 32 out of 128 cases), lung cancer (25%, 120 out of 481 cases), colorectal cancer (16%, 186 out of 1153 cases), and pancreatic cancer (2%, 6 out of 247 cases) (Fig. 3). In colorectal cancer, significant associations with TMB were observed for the KRAS G13D (p = 0.016) and KRAS G12V (p = 0.005) mutations. In the context of lung cancer, the KRAS G12C mutation showed a positive correlation with TMB-H, with a p-value of 0.000. In uterine cancer, the KRAS G13D and G12V mutations were found to have a significant impact on TMB. In gastric cancer, the KRAS G13D mutation was found to have a significant impact on TMB, indicated by a p-value of 0.025. Conversely, no statistically significant associations were observed in pancreatic cancer (Table 2).
Association of MSI status with KRAS mutations
The status of microsatellite instability high (MSI-H) varied across different malignancies, with the highest prevalence observed in gastric cancer (30%, 18 out of 60 cases), followed by uterine cancer (16%, 20 out of 128 cases), colorectal cancer (7%, 77 out of 1153 cases), pancreatic cancer (0%, 1 out of 247 cases), and lung cancer (0%, 1 out of 481 cases) (Fig. 4). In colorectal cancer, the KRAS G13D (p = 0.000) and KRAS G12V (p = 0.001) mutations exhibited significant effects on MSI-H. In gastric cancer, the KRAS G13D mutation was found to have a significant impact on MSI, indicated by a p-value of 0.015. In contrast, no statistically significant associations were identified in uterine and gastric cancers (Table 3).
Discussion
KRAS is a critical component in the downstream signaling pathways of the EGFR, notably within the RAS-RAF-MAPK and PI3K-mTOR pathways. Extensive evidence indicates that mutations in the KRAS gene lead to persistent activation of these signaling cascades. As a result, individuals harboring KRAS mutations often exhibit resistance to anti-EGFR targeted therapies (Jiang et al. 2024). Meanwhile, it has been reported that specific KRAS mutations are associated with TMB and MSI in various cancer types, and may influence the efficacy of immunotherapy (Hargadon et al. 2018; McGranahan et al. 2016). Here, we analyzed 10,820 cases of prevalent malignant tumors, encompassing gastrointestinal, reproductive system, respiratory, soft tissue, bone, urological, and neurological tumors, using NGS. Approximately 19.97% of Chinese patients with malignant tumors harbored KRAS mutations, and the mutation frequency was different from Western populations, particularly in biliary tract, thyroid, and neurological cancers. As for KRAS subtypes, KRAS G12D mutation is most common in pancreatic, colorectal, and gastric cancers, while KRAS G12V mutation is predominant in uterine cancer, and KRAS G12C mutation is most frequent in lung cancer. Moreover, KRAS-specific subtype mutations, including G13D, G12V, and G12C, had a close association with MSI status and TMB value.
KRAS represents the most frequently mutated oncogene in human malignancies, predominantly impacting epithelial cancers. Mutations are observed with a high frequency in Western populations, accounting for approximately 30% of cancers. Here, we identified a KRAS mutation rate of 19.97% within the cohort, with variation in KRAS mutation rates depending on the cancer type. These discrepancies in mutation prevalence between Chinese and Western populations may plausibly be attributed to ethnic variations.
Substantial evidence indicates that the KRAS gene plays a pivotal role in tumorigenesis and the modulation of tumor immunity. Prior research has shown that mutations in KRAS mutation can lead to the overexpression of PD-L1 by activating downstream pathways in NSCLC (Amanam et al. 2020; Sumimoto et al. 2016). And it was observed that the PD-L1 positivity rate was higher in patients with KRAS mutations compared to those with the KRAS wild-type (Herbst et al. 2020). In the KEYNOTE-189 study, both PD-L1 expression and TMB levels were found to be elevated in patients harboring KRAS mutations (Gadgeel et al. 2019). TMB has been shown to enhance tumor immunogenicity and potentially influence the response to immune checkpoint inhibitors (ICIs). And the findings of multiple studies have indicated that patients with KRAS mutations display markedly elevated TMB (Dong et al. 2017; Rizvi et al. 2015). This frequently indicates that patients with KRAS-mutated tumors respond better to immunotherapy. The findings of our study indicate that the proportion of high TMB (≥10 mut/Mb) is highest in gastric cancer, at 37%, followed by uterine cancer (25%) and lung cancer (25%). Further Chi-square test yielded statistically significant correlations between the KRAS G13D and KRAS G12V mutations sites and TMB values in colorectal cancer. Additionally, the analysis revealed that the KRAS G13D mutation site had a notable influence on TMB in gastric cancer. Moreover, KRAS G12C mutation significantly associated with TMB in lung cancer, which provides a potential explanation for the favourable outcomes of pembrolizumab immunotherapy observed in patients with KRAS G12C mutation (Gadgeel et al. 2019; Diaz et al. 2022).
Defects in the mismatch repair system (dMMR) are a primary cause of MSI, which is characterised by a distinct mutant phenotype. The FDA has granted full approval to the use of pembrolizumab in the treatment of patients diagnosed with unresectable and metastatic MSI-H or dMMR solid tumors that have progressed following previous therapeutic intervention. Findings from multiple studies further substantiate the use of pembrolizumab as a primary treatment for Asian patients with mCRC and MSI-H/dMMR (Diaz et al. 2022; Yoshino et al. 2023). In this study, MSI status varied significantly across different malignancies, with the highest prevalence of MSI-H observed in gastric cancer (30.0%), followed by uterine cancer (15.6%), colorectal cancer (6.7%), pancreatic cancer (0.4%), and lung cancer (0.2%). In colorectal cancer, the KRAS G13D and KRAS G12V mutations demonstrated significant effects on MSI status.
There were several limitations. It must be acknowledged that the present study, which has yielded valuable insights into the role of KRAS mutation in tumor development, has been subject to a degree of bias in its sample selection process. The number of samples included in the analysis of breast tumors, bone tumors and neurotumors was comparatively low. Furthermore, this study offers new insights by concentrating on the characterization of KRAS mutantion molecular isoforms and their correlation with TMB and MSI. Nevertheless, our study has yet to assess the impact of these molecular characteristics on therapeutic efficacy. While our data provide clues to potential therapeutic targets, the therapeutic efficacy of these in real-world applications remains to be validated by further clinical trials. The association between these molecular features and therapeutic response, as well as the possibility of developing novel therapeutic strategies based on these findings, are avenues that future studies should explore.
In summary, the prevalence of KRAS mutations varied among different malignant tumors, with the highest frequency observed in tumors of the digestive, female reproductive, and respiratory systems. The influence of various KRAS mutation sites on TMB and MSI in distinct tumors suggests potential implications for immunotherapy. The findings of this study provide valuable insights into the potential applicability of targeted therapies and immunotherapy for KRAS-mutant tumors.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- KRAS :
-
Kirsten rat sarcoma viral oncogene
- NGS:
-
Next-generation sequencing
- TCGA:
-
The Cancer Genome Atlas
- CHCAMS:
-
Cancer Hospital Chinese academy of medical sciences
- PD-L1:
-
Programmed death-ligand-1
- EGFR:
-
Epidermal growth factor receptor
- TMB:
-
Tumor mutational burden
- MSI:
-
Microsatellite instability
- ICIs:
-
Immune checkpoint inhibitors
- NGS:
-
Next-generation sequencing
- PCR:
-
Polymerase chain reaction
- FDA:
-
Food and drug administration
- NSCLC:
-
Non-small cell lung cancer
- PDAC:
-
Pancreatic ductal adenocarcinoma
- COADREAD:
-
Colon adenocarcinoma/rectum adenocarcinoma esophageal carcinoma
- STAD:
-
Stomach adenocarcinoma
- PAAD:
-
Pancreatic adenocarcinoma
- ESCA:
-
Esophageal carcinoma
- CHOL:
-
Cholangiocarcinoma
- LUAD:
-
Lung adenocarcinoma
- LUSC:
-
Lung squamous cell carcinoma
- UCEC:
-
Uterine corpus endometrial carcinoma
- OV:
-
Ovarian serous cystadenocarcinoma
- CESC:
-
Cervical squamous cell carcinoma and endocervical adenocarcinoma
- HNSC:
-
Head and neck squamous cell carcinoma
- THCA:
-
Thyroid carcinoma
- dMMR:
-
Mismatch repair system
References
Amanam I, Mambetsariev I, Gupta R, Achuthan S, Wang Y, Pharaon R, Massarelli E, Koczywas M, Reckamp K, Salgia R (2020) Role of immunotherapy and co-mutations on KRAS-mutant non-small cell lung cancer survival. J Thorac Dis 12:5086–5095. https://doi.org/10.21037/jtd.2020.04.18
Cazzanelli G, Pereira FA-O, Alves SA-O, Francisco R, Azevedo L, Dias Carvalho P, Almeida A, Côrte-Real M, Oliveira MJ, Lucas C, Sousa MA-O, Preto A (2018) The yeast Saccharomyces cerevisiae as a model for understanding RAS proteins and their role in human tumorigenesis. Cells. https://doi.org/10.3390/cells7020014
Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, Schrock A, Campbell B, Shlien A, Chmielecki J, Huang F, He Y et al (2017) Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9:34. https://doi.org/10.1186/s13073-017-0424-2
Diaz LA Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, Smith D, Garcia-Carbonero R, Benavides M, Gibbs P, de la Fourchardiere C, Rivera F et al (2022) Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol 23:659
Dong ZY, Zhong WZ, Zhang XC, Su J, Xie Z, Liu SY, Tu HY, Chen HJ, Sun YL, Zhou Q, Yang JJ, Yang XN et al (2017) Potential predictive value of TP53 and KRAS mutation status for response to PD-1 blockade immunotherapy in lung adenocarcinoma. Clin Cancer Res 23:3012–3024. https://doi.org/10.1158/1078-0432.CCR-16-2554
Gadgeel S, Rodriguez-Abreu D, Felip E, Esteban E, Speranza G, Reck M, Hui R, Boyer M, Garon EB, Horinouchi H, Cristescu R, Aurora-Garg D et al (2019) KRAS mutational status and efficacy in KEYNOTE-189: pembrolizumab (pembro) plus chemotherapy (chemo) vs placebo plus chemo as first-line therapy for metastatic non-squamous NSCLC. Ann Oncol 30:xi64–xi65. https://doi.org/10.1093/annonc/mdz453.002
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C et al (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 6:1. https://doi.org/10.1126/scisignal.2004088
Hallin J, Bowcut V, Calinisan A, Briere DM, Hargis L, Engstrom LD, Laguer J, Medwid J, Vanderpool D, Lifset E, Trinh D, Hoffman N et al (2022) Anti-tumor efficacy of a potent and selective non-covalent KRAS(G12D) inhibitor. Nat Med 28:2171–2182. https://doi.org/10.1038/s41591-022-02007-7
Hargadon KM, Johnson CE, Williams CJ (2018) Immune checkpoint blockade therapy for cancer: an overview of FDA-approved immune checkpoint inhibitors. Int Immunopharmacol 62:29–39. https://doi.org/10.1016/j.intimp.2018.06.001
Herbst RS, Garon EB, Kim DW, Cho BC, Perez-Gracia JL, Han JY, Arvis CD, Majem M, Forster MD, Monnet I, Novello S, Szalai Z et al (2020) Long-term outcomes and retreatment among patients with previously treated, programmed death-ligand 1-positive, advanced non-small-cell lung cancer in the KEYNOTE-010 study. J Clin Oncol. https://doi.org/10.1200/JCO.19.02446
Hunter JC, Manandhar A, Carrasco MA, Gurbani D, Gondi S, Westover KD (2015) Biochemical and structural analysis of common cancer-associated KRAS mutations. Mol Cancer Res 13:1325–1335. https://doi.org/10.1158/1541-7786.MCR-15-0203
Jiang J, Berry MF, Lui NS, Liou DZ, Trope WL, Backhus LM, Shrager JB (2024) Clinical impact of EGFR and KRAS mutations in surgically treated unifocal and multifocal lung adenocarcinoma. Transl Lung Cancer Res. 13:1222–1231. https://doi.org/10.21037/tlcr-24-165
Kemp SB, Cheng N, Markosyan N, Sor R, Kim IK, Hallin J, Shoush J, Quinones L, Brown NV, Bassett JB, Joshi N, Yuan S et al (2023) Efficacy of a small-molecule inhibitor of KrasG12D in immunocompetent models of pancreatic cancer. Cancer Discov 13:298–311. https://doi.org/10.1158/2159-8290.CD-22-1066
Kim JH, Kim HS, Kim BJ (2017) Prognostic value of KRAS mutation in advanced non-small-cell lung cancer treated with immune checkpoint inhibitors: a meta-analysis and review. Oncotarget 8:48248–48252. https://doi.org/10.18632/oncotarget.17594
Kulkarni AM, Kumar VA-O, Parate SA-O, Lee G, Yoon S, Lee KW (2022) Identification of new KRAS G12D inhibitors through computer-aided drug discovery methods. Int J Mol Sci. https://doi.org/10.3390/ijms23031309
McGranahan N, Furness AJ, Rosenthal R, Ramskov S, Lyngaa R, Saini SK, Jamal-Hanjani M, Wilson GA, Birkbak NJ, Hiley CT, Watkins TB, Shafi S et al (2016) Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351:1463–1469. https://doi.org/10.1126/science.aaf1490
Nakajima EC, Drezner N, Li X, Mishra-Kalyani PS, Liu Y, Zhao H, Bi Y, Liu J, Rahman A, Wearne E, Ojofeitimi I, Hotaki LT et al (2022) FDA approval summary: sotorasib for KRAS G12C-mutated metastatic NSCLC. Clin Cancer Res 28:1482–1486. https://doi.org/10.1158/1078-0432.CCR-21-3074
Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, Miller ML, Rekhtman N et al (2015) Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. https://doi.org/10.1126/science.aaa1348
Stephen AG, Esposito D, Bagni RK, McCormick F (2014) Dragging ras back in the ring. Cancer Cell 25:272–281. https://doi.org/10.1016/j.ccr.2014.02.017
Sumimoto H, Takano A, Teramoto K, Daigo Y (2016) RAS-mitogen-activated protein kinase signal is required for enhanced PD-L1 expression in human lung cancers. PLoS ONE. https://doi.org/10.1371/journal.pone.0166626
Trabucco SE, Gowen K, Maund SL, Sanford E, Fabrizio DA, Hall MJ, Yakirevich E, Gregg JP, Stephens PJ, Frampton GM, Hegde PS, Miller VA et al (2019) A novel next-generation sequencing approach to detecting microsatellite instability and pan-tumor characterization of 1000 microsatellite instability-high cases in 67,000 patient samples. J Mol Diagn 21:1053–1066. https://doi.org/10.1016/j.jmoldx.2019.06.011
Yoshino TA-O, Andre T, Kim TW, Yong WP, Shiu KK, Jensen BV, Jensen LH, Punt CJA, Smith D, Garcia-Carbonero R, Alcaide-Garcia J, Gibbs P et al (2023) Pembrolizumab in Asian patients with microsatellite-instability-high/mismatch-repair-deficient colorectal cancer. Cancer Sci 114:1026
Acknowledgements
Not applicable.
Funding
This work was supported by grants from the National Key Research and Development Program of China (2022YFC2409902) and Beijing Hope Run Special Fund of Cancer Foundation of the People’s Republic of China (LC2019L04).
Author information
Authors and Affiliations
Contributions
J. Y., W. L. and L. G. contributed to methodology, validation, and project administration. L. W., W. R., F.Z. and W. L. conducted formal analysis and data curation. All authors contributed substantially to the interpretation and writing of the manuscript. L.W. and W. R. were co-first authors and their contributions to the article were equal. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Ethical approval
The NGS data included in this study have been subjected to a rigorous review process by the CHCAMS Ethics Committee, and ethical approval has been granted (NCC2694). The study was conducted in accordance with the ethical principles set forth in the Declaration of Helsinki for research involving human subjects. Prior to participation, all subjects were required to sign an informed consent form, which provided detailed information about the purpose of the experiment, the methods to be employed, the potential risks, the expected benefits, and the subjects' rights.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, L., Rao, W., Guo, L. et al. Pan-cancer analysis to character the clinicopathological and genomic features of KRAS-mutated patients in China. J Cancer Res Clin Oncol 151, 94 (2025). https://doi.org/10.1007/s00432-025-06118-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-025-06118-9