Abstract
Purpose
The goal of this study is to examine the chronological development of hospitalized oncology and COVID-19 patients, and compare effects on oncology sub-disciplines for pre-pandemic (2017–19) and pandemic (2020–21) years in the setting of a German university maximum care provider.
Methods
Data were retrospectively retrieved from the hospital performance controlling system for patient collectives with oncological main (nOnco) and COVID-19 secondary diagnosis (nCOVID-19). Data analysis is based on descriptive statistical assessment.
Results
The oncology patient collective (nOnco = 27,919) shows a decrease of hospitalized patients for the whole pandemic (− 4% for 2020 and − 2,5% for 2021 to 2019). The number of hospitalized COVID-19 patients increases from first to second pandemic year by + 106.71% (nCOVID-19 = 868). Maximum decline in monthly hospitalized oncology patients amounts to − 19% (May 2020) during the first and − 21% (December 2020) during the second lockdown. Relative monthly hospitalization levels of oncology patients reverted to pre-pandemic levels from February 2021 onwards.
Conclusion
The results confirm a decline in hospitalized oncology patients for the entire pandemic in the setting of a maximum care provider. Imposed lockdown and contact restrictions, rising COVID-19 case numbers, as well as discovery of new virus variants have a negative impact on hospitalized treated oncological patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the onset of the rapidly advancing pandemic, spread of COVID-19 in the spring of 2020 society worldwide has been characterized by significant restrictions. Over the course of the last 2 years, the Federal Republic of Germany has registered about 7.109.182 confirmed COVID-19 cases (data from December 30th of 2021) (Robert Koch Institut 2021). The state of Hesse confirmed 477,279 COVID-19 cases with 8548 fatal outcomes leaving a state mortality rate of 1.8% on December 30th 2021 according to the Robert Koch Institute, the central national institution in the field of disease surveillance and prevention in Germany (Robert Koch Institut 2021). A variety of measures have been enforced politically restricting work and social life in a counterplay of recurrent lockdowns and gradual easing attempts. Internationally, the care of acute and chronic diseases has experienced noxious effects due to the pandemic (Czeisler et al. 2020; Lazzerini et al. 2020; Tangcharoensathien et al. 2021). To guarantee planning security and prevent critical capacity overload for the health care system, strong political influence was exerted on the medical care structure and organization which made regular service provision in German hospitals almost impossible at times. Oncology has widely been discussed as the medical field being particularly vulnerable to negative impact of the pandemic on the care situation (Alagoz et al. 2021; Andrew et al. 2021; De Luca et al. 2022; Earnshaw et al. 2020; Erdmann et al. 2021; Gurney et al. 2021; Jacob et al. 2021; Kuzuu et al. 2021; Patt et al. 2020; Peacock et al. 2021; Piontek et al. 2021; Reichardt et al. 2021; Ruiz-Medina et al. 2021; Stang et al. 2021; Tsibulak et al. 2020; Vardhanabhuti and Ng 2021; Voigtländer et al. 2021). In Germany, studies conducted in various states, e.g., Saxony (Piontek et al. 2021), North Rhine-Westphalia (Stang et al. 2021), or Bavaria (Voigtländer et al. 2021), have confirmed a decline of cancer cases during different time periods of the pandemic and on national scale studies have confirmed a decrease in oncological cases in general and specialized practices in Germany for April 2020–March 2021 and March–May 2020 (Jacob et al. 2021, 2022). The current literature focusses on parts of the pandemic and leaves out the perspective of an in-patient oncological maximum care provider.
This was an occasion to examine and compare the entire pandemic period of 2020 and 2021 with the previous years of 2017–2019 as a university maximum service provider of the state of Hesse with regard to the development of hospitalized oncology and COVID-19 patients, whether oncological sub-disciplines differ in terms of absolute and relative change of case count and how the monthly relative case development of admitted oncological patients relates to national lockdown and contact measures or to the discovery to new COVID-19 virus variants, e.g., delta and omicron virus variants.
Methods
Data generation
The data for the present analysis were retrospectively generated for the time period of 1st January 2017–31st December 2021 and retrieved from the hospital performance controlling program QlikView® of Marburg University Hospital, which records all medical, nursing, and equipment services coded in the hospital information system. Data were collected for all patients with a main oncology nOnco (ICD C-diagnosis) and a secondary COVID-19 diagnosis nCOVID-19 (ICD-code “U07.1 COVID-19, virus identified”). Furthermore, the oncological patient collective was divided in ICD-based groups for oncology sub-disciplines depicted in Table 3 and the statistical protocol was repeated. The data were fully anonymized before analysis.
Statistical methods
The evaluation is exclusively based on methods of descriptive statistics. The focus of the study lies on the analysis of the patient collective regarding age and gender distribution, the monthly and yearly relative development of the overall number of hospitalized patients, as well as the recorded main and secondary ICD diagnoses.
Results
Descriptive analysis of the patient collectives
A total of nOnco = 27,919 oncology patients have been hospitalized at Marburg University Hospital within the observation period. The data show a yearly relative increase in total case number for pre-pandemic years (+ 3% 2017–18, + 6% 2018–19) followed by decrease of − 4% (2019–20) for the first and an increase of + 1% (2020–21; − 2,5% 2019–21) for the second pandemic year. The oncology patient collective is divided in 45.4% female and 54.5% male with an average age of 64 and 66.1, respectively (n = 9 cases with unspecified gender). Regarding the in-patiently treated COVID-19 patient collective, a total of nCOVID-19 = 868 patients were analyzed leaving a relative increase of + 106.71% (2020–21) between the first and second pandemic year. The gender distribution divides in 42.2% female and 57.8% male with a mean age of 63.2 and 62, respectively. Absolute figures and the ten most common main diagnoses are illustrated in Tables 1 and 2.
Yearly absolute and relative development of oncology sub-disciplines (2017–21)
The yearly relative development and absolute patient numbers of the oncology sub-disciplines for pre-pandemic (2017–19) as well as pandemic years (2020–21) in comparison to the pre-pandemic baseline of 2019 are depicted in Table 3. Furthermore, the overall relative share of the nonco = 27,919 cases for whole observation period was identified for each oncological sub-discipline.
Monthly relative case development of the oncology and COVID-19 patient collectives (2019–21)
The monthly case count of all in-patient cases with an oncological main diagnosis admitted at the Marburg University Hospital in 2019 was used as a pre-pandemic baseline to visualize the relative monthly change in comparison to the pandemic years of 2020 and 2021. The illustration is combined with dates of lockdown and contact restriction measures taken by the Government of the Federal Republic of Germany and dates of the first national cases of COVID-19 delta and omicron virus variants.
Discussion
Main findings
The analysis illustrates a worrisome chronological development of in-patient oncology cases for the catchment area of Marburg University Hospital. The data confirm the national and international recognized decline in oncological cases for the setting of a maximum service provider for the entire pandemic time of 2020 and 2021, and show differences for oncological sub-disciplines (Andrew et al. 2021; De Luca et al. 2022; Erdmann et al. 2021; Gurney et al. 2021; Patt et al. 2020; Peacock et al. 2021; Piontek et al. 2021; Reichardt et al. 2021; Ruiz-Medina et al. 2021; Stang et al. 2021; Tsibulak et al. 2020; Vardhanabhuti and Ng 2021; Voigtländer et al. 2021). After 3 years of consecutive increase in oncological case count, that predominantly connects to the successive closure of regional peripheral care providers and the vice versa expansion of the oncological care network, the pandemic has stirred up oncological care in the catchment area of Marburg University Hospital.
Interpretation of findings
Comparison of oncological sub-disciplines
Worrisome, sub-groups with a high share of overall case count tend to realize a relative decline in the first pandemic year that intensifies for the second (i.e., − 15% in 2020 and − 18% in 2021 for uro-oncology C64-68; − 2% and − 6% for gastrointestinal oncology C15-C26; − 6% and − 18% for gyne-oncology of inner female genitals C51-C58). The extent of patient number decline for C60-63 and C64-C58 sub-groups could fraudulently be intensified by the departure of two specialized urologists for 2021. Other prominent sub-disciplines overcome the pandemic effects in the second year of observation (i.e., − 6% and + 2% for breast cancer C50; − 8% and + 1% for respiratory and thoracic cancer C30-39) or seem to be not affected at all (i.e., + 7% and + 3% for malignant skin cancer C43-C44; + 1% and + 2% for haemato- and lymphoid oncology C81-C96). International findings are coherent with these developments and confirm this noxious but divergent developments (Jacob et al. 2022; Kuzuu et al. 2021; Monroy‐Iglesias et al. 2022). Changes in sub-disciplines with small overall share (≤ 5% of overall oncology cases) tend to be biased by structural changes, managerial decisions, or changes in assigning out-patient physicians and practices, and display counterintuitive development (i.e., + 190% and 145% for bone and cartilage cancer C40-41, + 29% and + 25% for mesothelial cancer C45-C49). The contradicting increase for C40-41 for instance is likely affected by the external factor of an ownership exchange of an assigning local practice. Further managerial and structural biases can be ruled out to a large extent in case of Marburg University Hospital. The comparison of German out-patient and in-patient case numbers suggests that especially cancer types with out-patient screening programs (in Germany, e.g., skin, cervical, breast, colorectal, and prostate cancer) are effected by the pandemic leading to an expected increase of cancer stage upon primary disease diagnosis (Mayo et al. 2021).
Comparison of chronological development of oncology and COVID-19 patient collectives
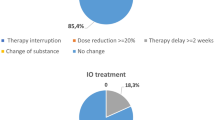
On January 27th of 2020, the first national COVID-19 case was registered in Germany. Due to the swift case development, the government of the Federal Republic of Germany initiated a “hard” lockdown with complete contact restrictions on March 22nd. Decision on first relaxations of contact measures was taken on May 3rd of 2020. During summer, only minor restrictions were maintained and the government reacted to a second accelerated COVID-19 case development by imposing a second lockdown “light” in early November including softer contact measures than during the first “hard” lockdown. Following the first national lockdown, Fig. 1 depicts a fierce decline in monthly relative case development of hospitalized oncology patients with a negative maximum of − 19% in May 2020 for Marburg University Hospital. The months of June and August display the only relative increase for the pandemic part of 2020, although these months realized a relative increase for 2019 and, therefore, we expect the data to be biased to external factors not mirroring the real relative development. As such, the decrease of monthly relative case development of oncological cases worsens with imposition of the lockdown “light” in early November reaching another negative maximum of − 21% in December 2020. As the national vaccination program is initiated in January, it also constitutes the last month of heavy relative decline in regional oncological cases leading to a phase of stabilization and oncological case growth. From February 2021 onwards, the registered monthly hospitalizations nearly fully revert to pre-pandemic levels. Figure 1 supports the second wave of COVID-19 cases to be far more intense in terms of in-patiently treated COVID-19. In contrast to other states in Germany, the Hessian state government did not actively interfere with hospital management by imposing a necessary amount of blocked beds for COVID-19 treatment, but provided accurate prediction of bed demand and, therefore, in Hesse proactive bed management for COVID-19 leaving no major discrepancies between used and blocked beds. An international study for 15 tumor types in 61 countries confirms a fragility of cancer surgery to lockdowns with one in seven patients in “hard” lockdowns not undergoing planned surgery for the first 3 months from local emergence of COVID-19 (Glasbey et al. 2021). While most of the literature only focusses on the first national “hard” lockdown with complete contact restrictions, the hereby presented study not only confirms the development during the first national “hard” lockdown for a German maximum service provider, but beyond that enables a comparison with the second “soft” lockdown. Thus, the second so-called German “lockdown light” lasting for a period of more than three times as long as the first one and that did not include complete contact restrictions, but, e.g., limitations to the certain amount of group sizes that varied according to incidence, compares to the first full lockdown in terms of decline of in-patient oncological cases. Interestingly, national number of COVID-19 cases as well as the registered in-patient of Marburg University Hospital clearly surpass the levels of the first “hard” lockdown, but the chronological development of in-patient oncological cases is similar.
While higher morbidity and mortality for the delta variant (AlQahtani et al. 2021; He et al. 2021; Hussey et al. 2021; Khedar et al. 2021) as well as faster spread due to higher contagiousness for the omicron variant (Grabowski et al. 2022; Pulliam et al. 2021) have widely been discussed, little is known about the consequences for oncological care. Furthermore, the swift increase of omicron variant is combined with a lower vaccination efficacy (Burki 2022) that presents to be even worse in cancer patients (Zeng 2021). To our knowledge, no study has investigated the effect of the discovery of new COVID-19 virus variants on in-patient oncological cases development. In June 2021, the first official delta virus variant case of COVID-19 was reported. While Marburg University Hospital realizes a relative increase in monthly relative case development of regional oncological cases for June 2021, it is followed by fierce decline of − 7% in July. The first omicron virus variant cases were officially reported in November 2021 and monthly regional oncological cases were identical for the same month in comparison to the 2019 baseline, while October and December realized a relative increase of + 7% and + 6%. The data suggest that the discovery of new virus variants of COVID-19 may have a negative effect on the monthly relative case development of in-patient oncological cases, although the impact presents to be far more short-term and lower in terms of intensity in comparison to the lockdown and contact measures.
Limitations
The presented analysis is based on the data of a single regional maximum service supplier of the state of Hesse in Germany, the Marburg University Hospital. Therefore, the transfer of the proposed findings is limited as the data are mainly valid for rural care. Effects of external variables cannot be ruled out based on the presented analysis and an expansion of the analysis to urban areas and multicentric data comparison would be favorable.
Conclusion
The presented analysis examines and compares the pandemic with the previous pre-pandemic years regarding the chronological development of the in-patient oncological care of Marburg University Hospital. Coherent to international studies, the number of overall cancer cases has declined in the observation period and the analysis suggests that the negative impact on hospitalized oncology patients diverges between sub-disciplines. The findings suggest imposed “hard” and “soft” lockdown and contact restrictions as well as discovery of new virus variants to have a negative impact on in-patiently treated oncology patients. Further research needs to confirm or invalidate these findings in other settings, while it is of utmost importance to measure the effects of lockdown and contact measures as well as discovery of new virus variants to be able to proactively act against a negative impact on cancer care and prohibit an increase in cancer stage upon disease onset.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Alagoz O, Lowry KP, Kurian AW et al (2021) Impact of the COVID-19 pandemic on breast cancer mortality in the US: estimates from collaborative simulation modeling. J Natl Cancer Inst 113(11):1484–1494. https://doi.org/10.1093/jnci/djab097
AlQahtani M, Bhattacharyya S, Alawadi A et al (2021) Morbidity and mortality from COVID-19 post-vaccination breakthrough infections in association with vaccines and the emergence of variants in Bahrain. Res Sq. https://doi.org/10.21203/rs.3.rs-828021/v1
Andrew TW, Alrawi M, Lovat P (2021) Reduction in skin cancer diagnoses in the UK during the COVID-19 pandemic. Clin Exp Dermatol 46(1):145–146. https://doi.org/10.1111/ced.14411
Burki TK (2022) Omicron variant and booster COVID-19 vaccines. Lancet Respir Med. https://doi.org/10.1016/s2213-2600(21)00559-2
Czeisler MÉ, Marynak K, Clarke KEN et al (2020) Delay or avoidance of medical care because of COVID-19-related concerns. Morb Mortal Wkly Rep 69(36):1250–1257. https://doi.org/10.15585/mmwr.mm6936a4
De Luca P, Bisogno A, Colacurcio V et al (2022) Diagnosis and treatment delay of head and neck cancers during COVID-19 era in a tertiary care academic hospital: what should we expect? Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-06834-1
Earnshaw CH, Hunter HJA, McMullen E et al (2020) Reduction in skin cancer diagnosis, and overall cancer referrals, during the COVID-19 pandemic. Br J Dermatol 183(4):792–794. https://doi.org/10.1111/bjd.19267
Erdmann F, Wellbrock M, Trübenbach C et al (2021) Impact of the COVID-19 pandemic on incidence, time of diagnosis and delivery of healthcare among paediatric oncology patients in Germany in 2020: evidence from the German childhood cancer registry and a qualitative survey. Lancet Reg Health Eur. https://doi.org/10.1016/j.lanepe.2021.100188
Glasbey J, Ademuyiwa A, Adisa A et al (2021) Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol 22(11):1507–1517. https://doi.org/10.1016/S1470-2045(21)00493-9
Grabowski F, Kochańczyk M and Lipniacki T (2022) The spread of SARS-CoV-2 variant Omicron with the doubling time of 2.0–3.3 days can be explained by immune evasion. medRxiv: 2021.12.08.21267494. https://doi.org/10.1101/2021.12.08.21267494. Accessed 1 Apr. 2022.
Gurney JK, Millar E, Dunn A et al (2021) The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand–a country pursuing COVID-19 elimination. Lancet Reg Health West Pac. https://doi.org/10.1016/j.lanwpc.2021.100127
He X, He C, Hong W et al (2021) The challenges of COVID-19 delta variant: prevention and vaccine development. MedComm 2(4):846–854. https://doi.org/10.1002/mco2.95
Hussey H, Davies M-A, Heekes A, et al. (2021) Higher mortality associated with the SARS-CoV-2 Delta variant in the Western Cape, South Africa, using RdRp target delay as a proxy. medRxiv 13(July): 2021.10.23.21265412. https://doi.org/10.1101/2021.10.23.21265412. Accessed 1 Apr. 2022.
Jacob L, Loosen SH, Kalder M et al (2021) Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers 13(3):1–11. https://doi.org/10.3390/cancers13030408
Jacob L, Kalder M, Kostev K (2022) Decrease in the number of patients diagnosed with cancer during the COVID-19 pandemic in Germany. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-03922-5
Khedar RS, Mittal K, Ambaliya HC, et al. (2021) Greater Covid-19 severity and mortality in hospitalized patients in second (Delta Variant) wave compared to the first: single centre prospective study in India. medRxiv: 2021.09.03.21263091. https://doi.org/10.1101/2021.09.03.21263091. Accessed 1 Apr. 2022.
Kuzuu K, Misawa N, Ashikari K et al (2021) Gastrointestinal cancer stage at diagnosis before and during the COVID-19 pandemic in Japan. JAMA Netw Open 4(9):1–12. https://doi.org/10.1001/jamanetworkopen.2021.26334
Lazzerini M, Barbi E, Apicella A et al (2020) Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 4(5):e10–e11. https://doi.org/10.1016/S2352-4642(20)30108-5
Mayo M, Potugari B, Bzeih R et al (2021) Cancer screening during the COVID-19 pandemic: a systematic review and meta-analysis. Mayo Clin Proc Innov Qual Outcomes. https://doi.org/10.1016/j.mayocpiqo.2021.10.003
Monroy-Iglesias MJ, Rai S, Mistretta FA et al (2022) Impact of the COVID-19 pandemic on urological cancers: the surgical experience of two cancer hubs in London and Milan. BJUI Compass. https://doi.org/10.1002/bco2.135
Patt D, Gordan L, Diaz M et al (2020) Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform 4:1059–1071. https://doi.org/10.1200/cci.20.00134
Peacock HM, Tambuyzer T, Verdoodt F et al (2021) Decline and incomplete recovery in cancer diagnoses during the COVID-19 pandemic in Belgium: a year-long, population-level analysis. ESMO Open. https://doi.org/10.1016/j.esmoop.2021.100197
Piontek D, Klagges S, Schubotz B et al (2021) Dokumentierte Krebsneuerkrankungen in den klinischen Krebsregistern Sachsens im Verlauf der COVID-19-Pandemie. Deutsches Arzteblatt International 118(18):328–329. https://doi.org/10.3238/arztebl.2021.0216
Pulliam JRC, Schalkwyk C van, Govender N, et al. (2021) Increased risk of SARS-CoV-2 reinfection associated with emergence of the Omicron variant in South Africa. medRxiv: 2021.11.11.21266068. https://doi.org/10.1101/2021.11.11.21266068. Accessed 1 Apr. 2022.
Reichardt P, Bollmann A, Hohenstein S et al (2021) Decreased incidence of oncology admissions in 75 Helios hospitals in Germany during the COVID-19 pandemic. Oncol Res Treatment 44(3):71–75. https://doi.org/10.1159/000512935
Robert Koch Institut (2021) Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). Robert Koch Institut 2021: 1–4. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Dez_2021/2021-12-30-en.pdf?__blob=publicationFile. Accessed 20 Apr. 2022.
Ruiz-Medina S, Gil S, Jimenez B et al (2021) Significant decrease in annual cancer diagnoses in Spain during the covid-19 pandemic: a real-data study. Cancers. https://doi.org/10.3390/cancers13133215
Stang A, Kühling L, Khil L et al (2021) Drop in cancer reporting by pathologists in North Rhine-Westphalia, Germany, during the COVID-19 lockdown. Deutsches Arzteblatt International 117(51–52):886–887. https://doi.org/10.3238/arztebl.2020.0886
Tangcharoensathien V, Bassett MT, Meng Q et al (2021) Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. https://doi.org/10.1136/bmj.n83
Tsibulak I, Reiser E, Bogner G et al (2020) Decrease in gynecological cancer diagnoses during the COVID-19 pandemic: an Austrian perspective. Int J Gynecol Cancer 30(11):1667–1671. https://doi.org/10.1136/ijgc-2020-001975
Vardhanabhuti V, Ng KS (2021) Differential impact of COVID-19 on cancer siagnostic services based on body regions: a public facility-based study in Hong Kong. Int J Radiat Oncol Biol Phys 111(2):331–336. https://doi.org/10.1016/j.ijrobp.2021.05.010
Voigtländer S, Hakimhashemi A, Inwald EC et al (2021) Auswirkungen der COVID-19-Pandemie auf die Zahl der Krebsneuerkrankungen und Krebsbehandlungen nach Tumorstadium in Bayern. Deutsches Arzteblatt International 118(39):660–661. https://doi.org/10.3238/arztebl.m2021.0329
Zeng C (2021) Neutralization and stability of SARS-CoV-2 omicron variant. Problems Endocr Pathol 78(4):57–64. https://doi.org/10.21856/j-pep.2021.4.08
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors declare that no funds and grants of other support were received during preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by SG. The first draft of the manuscript was written by SG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Griewing, S., Wagner, U., Lingenfelder, M. et al. Chronological development of in-patient oncology in times of COVID-19: a retrospective analysis of hospitalized oncology and COVID-19 patients of a German University Hospital. J Cancer Res Clin Oncol 149, 2551–2558 (2023). https://doi.org/10.1007/s00432-022-04044-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04044-8