Abstract
Purpose
To explore the appropriate method of mediastinal lymph node dissection for selected clinical stage IA (cIA) non-small cell lung cancer (NSCLC).
Methods
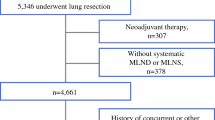
From 1998 through 2002, the curative-intent surgery was performed to 105 patients with cIA NSCLC who had been postoperatively identified as pathologic-stage T1. According to the method of intraoperative medistinal lymph node dissection, they were divided into radical systematic mediastinal lymphadenectomy (LA) group (n = 42) and mediastinal lymph-node sampling (LS) group (n = 63). The effects of LS and LA on morbidity, N staging, overall survival (OS) and disease-free survival (DFS) were investigated. Also, associations between clinicopathological parameters and survival were analyzed.
Results
The mean numbers of dissected lymph nodes per patient in the LA group was significantly greater than that in the LS group (15.59 ± 3.08 vs. 6.46 ± 2.21, P < 0.001), and the postoperative overall morbidity rate was higher in the LA group than that in the LS group (26.2 vs. 11.1%, P = 0.045). There were no significant difference in migration of N staging, OS and DFS between two groups. However, for patients with lesions between 2 and 3 cm, the 5-year OS in LA group was significantly higher than that in LS group (81.6 vs. 55.8%, P = 0.041), and the 5-year DFS was also higher (77.9 vs. 52.5%, P = 0.038). For patients with lesions of 2 cm or less, 5-year OS and DFS were similar in both groups. Multivariate analysis showed that lymph node metastasis was the unique unfavorable prognostic factor (P < 0.001).
Conclusions
After being intraoperatively identified as stage T1, patients with lesions between 2 and 3 cm in cIA NSCLC should be performed with LA to get a potentially better survival, and patients with lesions of 2 cm or less should be performed with LS to decrease invasion.




Similar content being viewed by others
Abbreviations
- cIA:
-
Clinical stage IA
- DFS:
-
Disease-free survival
- LA:
-
Radical systematic mediastinal lymphadenectomy
- LS:
-
Mediastinal lymph-node sampling
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
References
Bollen EC, van Duin CJ, Theunissen PH, vt Hof-Grootenboer BE, Blijham GH (1993) Mediastinal lymph node dissection in resected lung cancer: morbidity and accuracy of staging. Ann Thorac Surg 55:961–966
Cetinkaya E, Turna A, Yildiz P, Dodurgali R, Bedirhan MA, Gürses A, Yilmaz V (2002) Comparison of clinical and surgical-pathologic staging of the patients with non-small cell lung carcinoma. Eur J Cardiothorac Surg 22:1000–1005
Friedel G, Steger V, Kyriss T, Zoller J, Toomes H (2004) Prognosis in N2 NSCLC. Lung Cancer 45:S45–S53
Funatsu T, Matsubara Y, Ikeda S, Hatakenaka R, Hanawa T, Ishida H (1994) Preoperative mediastinoscopic assessment of N factors and the need for mediastinal lymphnode dissection in T1 lung cancer. J Thorac Cardiovasc Surg 108:321–328
Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, Morrow M (2002) AJCC Cancer Staging Manual, 6th edn. Springer, New York
Ishida T, Yano T, Madea K (1990) Strategy for lymphadenectomy in lung cancer 3 cm or less in diameter. Ann Thorac Surg 50:708–713
Izbicki JR, Thetter O, Habekost M, Karg O, Passlick B, Kubuschok B, Busch C, Haeussinger K, Knoefel WT, Pantel K et al (1994) Radical systematic mediastinal lymphadenectomy in non-small cell lung cancer: a randomized controlled trial. Br J Surg 81:229–235
Izbicki JR, Passlick B, Karg O, Bloechle C, Pantel K, Knoefel WT, Thetter O (1995) Impact of radical systemic mediastinal lymphadenectomy on tumor staging in lung cancer. Ann Thorac Surg 59:209–214
Izbicki JR, Passlick B, Pantel K, Pichlmeier U, Hosch SB, Karg O, Thetter O (1998) Effectiveness of radical systematic mediastinal lymphadenectomy in patients with resectable non-small cell lung cancer, results of a prospective randomized trial. Ann Surg 227:138–144
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer Statistics, 2007. CA Cancer J Clin 57:43–46
Keller SM, Adak S, Wagner H, Johnson DH (2000) Mediastinal lymph node dissection improves survival in patients with stages II and IIIa non-small cell lung cancer. Ann Thorac Surg 70:358–366
Martini N, Flehinger BJ (1987) The role of surgery in N2 lung cancer. Surg Clin North Am 67:1037–1049
Moutain CF (1997) Revisions in the international system for staging lung cancer. Chest 111:1710–1717
Naruke T, Suemasu K, Ishikawa S (1976) Surgical treatment for lung cancer with metastases to mediastinal lymph nodes. J Thorac Cardiovasc Surg 71:279–285
Naruke T, Tsuchiya R, Kondo H, Asamura H (2001) Prognosis and survival after resection for bronchogenic carcinoma based on the 1997 TNM-staging classification: the Japanese experience. Ann Thorac Surg 71:1759–1764
Nicholson AG, Graham AN, Pezzella F, Agneta G, Goldstraw P, Pastorino U (1997) Does the use of immunohistochemistry to identify micrometastasis provide useful information in the staging of node -negative non-small cell lung carcinomas? Lung Cancer 18:231–240
Oda M, Watanabe Y, Shimizu J, Murakami S, Ohta Y, Sekido N, Watanabe S, Ishikawa N, Nonomura A (1998) Extent of mediastinal node metastasis in clinical stageI non-small cell lung cancer: the role of systematic nodal dissection. Lung Cancer 22:23–30
Okada M, Sakamoto T, Yuki T, Mimura T, Miyoshi K, Tsubota N (2006) Selective mediastinal lymphadenectomy for clinico-surgical stage I non-small cell lung cancer. Ann Thorac Surg 81:1028–1032
Passlick B, Izbicki JR, Kubuschok B, Thetter O, Pantel K (1996) Detection of disseminated lung cancer cells in lymph nodes: impact on staging and prognosis. Ann Thorac Surg 61:177–183
Salerno CT, Frizelle S, Niehans GA, Ho SB, Jakkula M, Kratzke RA, Maddaus MA (1998) Detection of occult micrometastases in non-small cell lung carcinoma by reverse transcriptase-polymerase chain reaction. Chest 113:1526–1532
Sugi K, Nawata K, Fujita N, Ueda K, Tanaka T, Matsuoka T, Kaneda Y, Esato K (1998) Systematic lymph node dissection for clinically diagnosed non-small cell lung cancer less than 2 cm in diameter. World J Surg 22:290–295
Vansteenkiste JF, De Leyn PR, Deneffe GJ, Lerut TE, Demedts MG (1998) Clinical prognostic factor in surgically treated stage IIIA-N2 non-small cell lung cancer: analysis of the literature. Lung Cancer 19:3–13
Wu Y, Huang ZF, Wang SY, Yang XN, Ou W (2002) A randomized trial of systematic nodal dissection in resectable non-small cell lung cancer. Lung Cancer 36:1–6
Yamazaki K, Yoshino I, Yohena T, Kameyama T, Tagawa T, Kawano D, Oba T, Koso H, Maehara Y (2007) Clinically predictive factors of pathologic upstaging in patients with peripherally located clinical stage IA non-small cell lung cancer. Lung Cancer 55:365–369
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ma, K., Chang, D., He, B. et al. Radical systematic mediastinal lymphadenectomy versus mediastinal lymph node sampling in patients with clinical stage IA and pathological stage T1 non-small cell lung cancer. J Cancer Res Clin Oncol 134, 1289–1295 (2008). https://doi.org/10.1007/s00432-008-0421-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-008-0421-3