Abstract
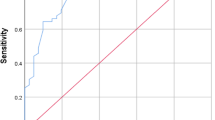
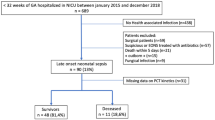
Infection is an important cause of death during infancy worldwide and is a frequent etiology of sudden unexpected death in infancy (SUDI). Procalcitonin (PCT) is a useful marker to diagnose infection in patients, and several studies report the stability of PCT after death. The added value of a biological marker, such as the PCT level in the blood, remains controversial in investigating SUDI. The aim of this study was to determine if PCT can help clinicians determine whether infection caused SUDI. We conducted a retrospective, multicenter study with the French SUDI registry (Observatoire National des Morts Inattendues du Nourrisson; OMIN). We collected data from this registry on children who died between May 2015 and June 2021. The levels of PCT in the blood of 540 SUDI patients were measured. We compared PCT and other biological tests performed in terms of infection status, autopsy results, and cause of death using clinical and biological data compiled by pediatricians at the SUDI referral center. PCT levels were significantly higher in the children who died from infection than in those who did not (0.12 µg/L vs. 0.08 µg/L, p < 0.001). A PCT blood level exceeding 0.2 µg/L was more frequently observed when infection was present than in the absence of infection (44.3% vs. 15.4%, p < 0.001). The same data were obtained with a 0.5 µg/L cut-off (36.1% with infection vs. 9.2% without, p < 0.001).
Conclusions: PCT is a sensitive biomarker for detecting infections postmortem; thus, additional samples may be necessary during autopsy.
What is known: • PCT is a stable marker postmortem and increases earlier than CRP, i.e., 2–4 h after the beginning of an infection vs. 6 h. • PCT can be measured up to 140 h after death. | |
What is new: • PCT is a sensitive marker for detecting infection in SUDI patients postmortem. • This test can reveal an infection from non-standardized samples obtained during autopsy if such an infection was not determined before death. |


Similar content being viewed by others
References
Levieux K, Patural H, Harrewijn I, Briand Huchet E, de Visme S, Gallot G, Chalumeau M, Gras Le Guen C, Hanf M, OMIN Study Group (2018) The French prospective multisite registry on sudden unexpected infant death (OMIN): rationale and study protocol. Br Med J 8(4):e020883. https://doi.org/10.1136/bmjopen-2017-020883
HAS (2007) Prise en charge en cas de mort inattendue du nourrisson (moins de 2 ans). https://www.has-sante.fr/jcms/c_533467/fr/prise-en-charge-en-cas-de-mort-inattendue-du-nourrisson-moins-de-2-ans. Accessed 3 Jan 2022
OMIN (2022) Observatoire national des morts inattendues du nourrisson. OMIN https://www.omin.fr/. Accessed 10 Jan 2022
de Visme S, Chalumeau M, Levieux K, Patural H, Harrewijn I, Briand-Huchet É, Rey G, Morgand C, Blondel B, Gras-Le Guen C, Hanf M (2020) National variations in recent trends of sudden unexpected infant death rate in Western Europe. J Pediatr 226:179-185.e4. https://doi.org/10.1016/j.jpeds.2020.06.052
Bloch J, Denis P, Jezewski-Serra D (2022) Les morts inattendues des nourrissons de moins de 2 ans. InVS. http://archives.invs.santepubliquefrance.fr/publications/2011/morts_nourrissons/index.html. Accessed 10 Jan 2022
Oliveira M, Amorim A (2018) Microbial forensics: new breakthroughs and future prospects. Appl Microbiol Biotechnol 102(24):10377–10391. https://doi.org/10.1007/s00253-018-9414-6
Gaaloul I, Riabi S, Evans M, Hunter T, Huber S, Aouni M (2016) Postmortem diagnosis of infectious heart diseases: a mystifying cause of Sudden Infant Death. Forensic Sci Int 262:166–172. https://doi.org/10.1016/j.forsciint.2016.03.002
Hamade B, Huang DT (2020) Procalcitonin : where are we now? Crit Care Clin 36(1):23–40. https://doi.org/10.1016/j.ccc.2019.08.003
Biomnis (2012) Procalcitonine In : Précis de biopathologie analyses médicales spécialisées Biomnis. https://www.eurofins-biomnis.com/referentiel/liendoc/precis/PROCALCITONINE.pdf. Accessed 15 Jan 2022
Damman J, Arias P, Kerner J, Zhang K-Y, Dehghan M, Krishnan G, Nespor C, Bensen R, Park KT (2019) Procalcitonin as a predictive marker for bacteremia in children with a central line and fever. Hosp Pediatr 9(6):434–439. https://doi.org/10.1542/hpeds.2018-0123
Shaikh KJ, Osio VA, Leeflang MM, Shaikh N (2020) Procalcitonin, C-reactive protein, and erythrocyte sedimentation rate for the diagnosis of acute pyelonephritis in children. Cochr Data Syst Rev 9(9):CD009185. https://doi.org/10.1002/14651858.CD009185.pub3
Tsokos M, Reichelt U, Nierhaus A, Püschel K (2001) Serum procalcitonin (PCT): a valuable biochemical parameter for the post-mortem diagnosis of sepsis. Int J Leg Med 114(4–5):237–243. https://doi.org/10.1007/s004140000177
Schrag B, Roux-Lombard P, Schneiter D, Vaucher P, Mangin P, Palmiere C (2012) Evaluation of C-reactive protein, procalcitonin, tumor necrosis factor alpha, interleukin-6, and interleukin-8 as diagnostic parameters in sepsis-related fatalities. Int J Leg Med 126(4):505–512. https://doi.org/10.1007/s00414-011-0596-z
Barranco R, Ventura F (2019) Biochemical markers and microbiology in post-mortem diagnosis of sepsis: a systematic review. Rom J Leg Med 27(3):230–238. https://doi.org/10.4323/rjlm.2019.230
Attia AM, Abo El-Atta HM, El-sherbiny M, El-Shahat EE (2016) Evaluation of procalcitonin postmortem levels in some models of death: an experimental study. J Forensic Leg Med 37:28–32. https://doi.org/10.1016/j.jflm.2015.08.011
Ferrière F (2000) Intérêt de la procalcitonine, nouveau marqueur de l’infection bactérienne. Ann Biol Clin 58(1):49–59
Bruel AV, den Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, Mant D (2011) Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 342:d3082. https://doi.org/10.1136/bmj.d3082
Leroy S, Fernandez-Lopez A, Nikfar R, Romanello C, Bouissou F, Gervaix A, Gurgoze MK, Bressan S, Smolkin V, Tuerlinckx D, Stefanidis CJ, Vaos G, Leblond P, Gungor F, Gendrel D, Chalumeau M (2013) Association of procalcitonin with acute pyelonephritis and renal scars in pediatric UTI. Pediatr 131(5):870–879. https://doi.org/10.1542/peds.2012-2408
Oussalah A, Ferrand J, Filhine-Tresarrieu P, Aissa N, Aimone-Gastin I, Namour F, Garcia M, Lozniewski A, Guéant JL (2015) Diagnostic accuracy of procalcitonin for predicting blood culture results in patients with suspected bloodstream infection. Medicine 94(44):e1774. https://doi.org/10.1097/MD.0000000000001774
Sager R, Kutz A, Mueller B, Schuetz P (2017) Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med 15(1):15. https://doi.org/10.1186/s12916-017-0795-7
Saegeman V, Cohen MC, Burton JL, Martinez MJ, Rakislova N, Offiah AC, Fernandez-Rodriguez A (2021) Microbiology in minimally invasive autopsy: best techniques to detect infection. ESGFOR (ESCMID study group of forensic and post-mortem microbiology) guidelines. Forensic Sci Med Pathol 17(1):87–100. https://doi.org/10.1007/s12024-020-00337-x
Weber MA, Hartley JC, Brooke I, Lock PE, Klein NJ, Malone M, Sebire NJ (2010) Post-mortem interval and bacteriological culture yield in sudden unexpected death in infancy (SUDI). Forensic Sci Int 198(1–3):121–125. https://doi.org/10.1016/j.forsciint.2010.02.002
Astrup BS, Thomsen JL (2007) The routine use of C-reactive protein in forensic investigations. Forensic Sci Int 172(1):49–55. https://doi.org/10.1016/j.forsciint.2006.10.021
Ondruschka B, Woydt L, Bernhard M, Franke H, Kirsten H, Löffler S, Pohlers D, Hammer N, Dreßler J (2019) Post-mortem in situ stability of serum markers of cerebral damage and acute phase response. Int J Leg Med 133(3):871–881. https://doi.org/10.1007/s00414-018-1925-2
Lindroos-Jokinen K, Keltanen T, Vanhala T, Valonen T, Sajantila A (2012) Postmortem measurement of C-reactive protein and interpretation of results in ketoacidosis. Leg Med 14(3):140–146. https://doi.org/10.1016/j.legalmed.2012.01.009
Downes KJ, Fitzgerald JC, Weiss SL (2020) Utility of procalcitonin as a biomarker for sepsis in children. J Clin Microbiol 58(7):e01851-e1919. https://doi.org/10.1128/JCM.01851-19
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P (2013) Procalcitonin as a diagnostic marker for sepsis : a systematic review and meta-analysis. Lancet Infect Dis 13(5):426–435. https://doi.org/10.1016/S1473-3099(12)70323-7
Kim H, Roh YH, Yoon SH (2021) Blood procalcitonin level as a diagnostic marker of pediatric bacterial meningitis: a systematic review and meta-analysis. Diagn (Basel, Switzerland) 11(5):846. https://doi.org/10.3390/diagnostics11050846
Stassi C, Mondello C, Baldino G, Ventura Spagnolo E (2020) Post-mortem investigations for the diagnosis of sepsis: a review of literature. Diagn 10(10):E849. https://doi.org/10.3390/diagnostics10100849
Segal GS, Chamberlain JM (2000) Resource utilization and contaminated blood cultures in children at risk for occult bacteremia. Arch Pediatr Adolesc Med 154(5):469–473. https://doi.org/10.1001/archpedi.154.5.469
Acknowledgements
We thank the families affected by SUDI as well as the participating centers. We also are grateful to the OMIN study group for the data.
Author information
Authors and Affiliations
Contributions
Author Contributions: All authors contributed to the study's conception and design. Material preparation, data collection and analysis were performed by M.C., M.H. and A.W.. M.C. and A.W. wrote the first draft of the manuscript, and all authors commented on the previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Collette, M., Hauet, M., de Visme, S. et al. Procalcitonin is associated with sudden unexpected death in infancy due to infection. Eur J Pediatr 182, 3929–3937 (2023). https://doi.org/10.1007/s00431-023-05064-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05064-3