Abstract
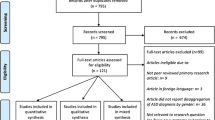
Early puberty signs lead to an increase in anxiety levels of parents and children. The aim of this study was to investigate the quality of life and anxiety levels of girls and their mothers who were admitted to a pediatric endocrinology clinic with concerns about early puberty. Girls and their mothers who were admitted to endocrinology outpatient clinic with concerns about early puberty were compared to healthy control group. Screen for Child Anxiety Related Emotional Disorders (SCARED) parent form, Quality of Life for Children Scale (PedsQL) parent form, and Beck Anxiety Inventory (BAI) were administered to the mothers. Children were evaluated with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (Kiddie-SADS Lifetime Version) (K-SADS-PL). The study sample consisted of 92 girls and 62 of them were administered to clinic with concerns about early puberty. There were 30 girls in early puberty group (group 1), 32 girls were in the normal development group (group 2), and 30 were in the healthy control group (group 3). The anxiety level of group 1 and group 2 was significantly higher, and their quality of life was significantly lower when compared to group 3 (p < 0.001). Mother’s anxiety level was found significantly higher in group 2 (p < 0.001). It has shown that anxiety level and quality of life of children were associated with anxiety level of mothers and the current Tanner stage (r = 0.302, p < 0.005).
Conclusion: Mothers and children who have concerns about early puberty are negatively affected when early puberty is a possibility. For this reason, educating parents will prevent negative impacts of this situation on children. At the same time, it will decrease health burden.
What is Known? • Early adolescence is one of the most common reasons for admission to pediatric endocrinology outpatient clinics. It is known that increasing early adolescence anxiety in the society causes cost and time losses in the field of health. However, studies investigating the reasons for this result are limited in the literature. | |
What’s New? • The level of anxiety increased significantly in girls with suspected precocious puberty and their mothers, and their quality of life was affected. • For this reason, we would like to emphasize the importance of multidisciplinary approaches before psychiatric disorders occur in children with suspected precocious puberty and their parents. |
Similar content being viewed by others
Availability of data and material
N/A.
Code availability
N/A.
Abbreviations
- BAI:
-
Beck Anxiety Inventory
- K-SADS-PL:
-
Schedule for Affective Disorders and Schizophrenia for School-Age Children (Kiddie-SADS Lifetime Version)
- PHTS:
-
Physical health total score
- PSTS:
-
Psychosocial health total score
- PedsQL:
-
Pediatric Quality of Life Inventory
- SCARED:
-
Screen for Child Anxiety and Related Disorders
References
Berberoğlu M (2009) Precocious puberty and normal variant puberty: definition, etiology, diagnosis and current management - review. J Clin Res Pediatr Endocrinol 1(4):164
Berberoğlu M (2010) Erken puberte. Türkiye Çocuk Hast Derg / Turkish J Pediatr Dis 4(1):61–64
Farello G, Altieri C, Cutini M, Pozzobon G, Verrotti A (2019) Review of the literature on current changes in the timing of pubertal development and the incomplete forms of early puberty. Front Pediatr 8:7
Kim YJ, Kwon A, Jung MK, Kim KE, Suh J, Chae HW, Kim DH, Ha S, Seo GH, Kim HS (2019) Incidence and prevalence of central precocious puberty in Korea: an epidemiologic study based on a national database. J Pediatr 208:221–228
Latronico AC, Brito VN, Carel JC (2016) Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 4(3):265–274
Partsch CJ (2001) Pathogenesis and epidemiology of precocious puberty. Effects of exogenous oestrogens. Hum Reprod Update 7(3):292–302
Esen İ, Demirel F, Tepe D, Demir B (2011) Bir Çocuk Endokrinolojisi Ünivertesine Başvuran Çocukların Klinik Özellikleri. Türkiye Çocuk Hastalıkları Dergisi 5(3):133–138
Erling A, Wiklund I, Albertsson-Wikland K (1994) Prepubertal children with short stature have a different perception of their well-being and stature than their parents. Qual Life Res 3(6)
Ahmadzadeh YI, Eley TC, Leve LD, Shaw DS, Natsuaki MN, Reiss D, Neiderhiser JM, McAdams TA (2019) Anxiety in the family: a genetically informed analysis of transactional associations between mother, father and child anxiety symptoms. J Child Psychol Psychiatry 60(12)
Niditch LA, Varela RE (2011) Mother-child disagreement in reports of child anxiety: effects of child age and maternal anxiety. J Anxiety Disord 25(3)
Rudolph KD (2014) Puberty as a developmental context of risk for psychopathology. In: Handbook of Developmental Psychopathology: Third Edition
Tsai MC, Strong C, Lin CY (2015) Effects of pubertal timing on deviant behaviors in Taiwan: alongitudinal analysis of 7th- to 12th-grade adolescents. J Adolesc 42
Galvao TF, Silva MT, Zimmermann IR, Souza KM, Martins SS, Pereira MG (2014) Pubertal timing in girls and depression: a systematic review. J Affect Disord 155
Toffol E, Koponen P, Luoto R, Partonen T (2014) Pubertal timing, menstrual irregularity, and mental health: results of a population-based study. Arch Womens Ment Health 17(2)
Yıldız Ö, Çakın-Memik N, Ağaoğlu B (2010) Dikkat eksikliği hiperaktivite bozukluğu tanılı çocuklarda yaşam kalitesi: Kesitsel bir çalışma. Noropsikiyatri Arsivi. 47
Turan AP, Akca SO (2021) The quality of life of children with precocious puberty and healthy children in turkey. Am J Health Behav 45(1)
Çoban ÖG, Bedel A, Önder A, Adanır AS, Tuhan H, Parlak M (2021) Psychiatric disorders, peer-victimization, and quality of life in girls with central precocious puberty. J Psychosom Res 143:110–401
Temelturk RD, Ilcioglu Ekici G, Beberoglu M, Siklar Z, Kilic BG (2021) Managing precocious puberty: a necessity for psychiatric evaluation. Asian J Psychiatr 58:102617
Eren SE, Simsek E (2023) Comparison of makorin ring finger protein 3 levels between obese and normal weight patients with central precocious puberty. J Clin Res Pediatr Endocrinol. https://doi.org/10.4274/jcrpe.galenos.2023.2022-6-6
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M (1999) Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38(10)
Çakmakçı FK (2004) Çocuklarda anksiyete bozukluklarını tarama ölçeği geçerlik ve güvenirlik çalışması. Çocuk ve Gençlik Ruh Sağlığı Dergisi 11(2)
Varni JW, Rode CA, Seid M, Katz ER, Friedman-Bender A, Quiggins DJL (1999) The pediatric cancer quality of life inventory-32 (PCQL-32). II. Feasibility and range of measurement. J Behav Med 122(4)
Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 56(6):893–897
Ulusoy M, Sahin NH, Erkmen H. (1998). Turkish version of the Beck anxiety inventory: psychometric properties. J Cogn Psychother: Int Quat 12(2)
Kaufman JBBAD et al (2016) Schedule for affective disorders and schizophrenia for school-aged children: present and lifetime version (K-SADS-PL) DSM-5. New Haven
Ünal F, Öktem F, Çetin Çuhadaroğlu F, Çengel Kültür SE, Akdemir D, Foto Özdemir D et al (2019) Reliability and validity of the schedule for affective disorders and schizophrenia for school-age children-present and lifetime version, DSM-5 November 2016-Turkish adaptation (K-SADS-PL-DSM-5-T). Turk Psikiyatri Dergisi 30(1)
Young Ahn H, Hee Yoo K, Ryeong Song M (2022) Guilt, uncertainty, education needs, and knowledge of mothers with children experiencing precocious puberty. Glob Pediatr Health 12(9):2333794X2210983
Cemeroglu AP, Kaval D, Ozcan O (2022) Etiology of increased referrals for evaluation of early puberty in a tertiary care center in turkey: true precocious puberty, obesity, or parental anxiety and lack of knowledge? Glob Pediatr Health 8:2333794X2110090
Li W, Liu Q, Deng X, Chen Y, Liu S, Story M(2017) Association between obesity and puberty timing: a systematic review and meta-analysis. Int J Environ Res Public Health 14(10):1266
Ellis BJ (2004) Timing of pubertal maturation in girls: an integrated life history approach. Psychol Bull 130(6):920–958
Magnus MC, Anderson EL, Howe LD, Joinson CJ, Penton-Voak IS, Fraser A (2018) Childhood psychosocial adversity and female reproductive timing: a cohort study of the ALSPAC mothers. J Epidemiol Community Health 72(1):34–40
Culpin I, Heron J, Araya R, Joinson C (2015) Early childhood father absence and depressive symptoms in adolescent girls from a UK cohort: the mediating role of early menarche. J Abnorm Child Psychol 43(5):921–31
Kaplowitz P, Bloch C, Sills IN, Bloch CA, Casella SJ, Gonzalez JL et al (2016) Evaluation and referral of children with signs of early puberty. Pediatrics 137(1)
Wohlfahrt-Veje C, Mouritsen A, Hagen CP, Tinggaard J, Mieritz MG, Boas M et al (2016) Pubertal onset in boys and girls is influenced by pubertal timing of both parents. J Clin Endocrinol Metab 101(7):2667–2674
Xiao Y, Li Y, Cai Z, Xie J (2022) Investigation on the correlation of anxiety degree with family atmosphere in children with precocious puberty. Emerg Med Int 23(2022):1–8
Reardon LE, Leen-Feldner EW, Hayward C (2009) A critical review of the empirical literature on the relation between anxiety and puberty. Clin Psychol Rev 29(1):1–23
Schoelwer MJ, Donahue KL, Didrick P, Eugster EA (2017) One-year follow-up of girls with precocious puberty and their mothers: do psychological assessments change over time or with treatment? Horm Res Paediatr 88(5):347–353
Mercader-Yus E, Neipp-López MC, Gómez-Méndez P, Vargas-Torcal F, Gelves-Ospina M, Puerta-Morales L et al (2018) Ansiedad, autoestima e imagen corporal en niñas con diagnóstico de pubertad precoz. Rev Colomb Psiquiatr 47(4):229–236
Zehr J, Culbert K, Sisk C, Klump K (2007) An association of early puberty with disordered eating and anxiety in a population of undergraduate women and men. Horm Behav 52(4):427–435
Barlow JH, Ellard DR (2006) The psychosocial well-being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child: Care, Health and Development 32
Yang H, Luo S, Liang X, Lin Q, Cheng T, Zeng L et al (2021) The association between family impact and health-related quality of life of children with idiopathic central precocious puberty in Chongqing. China Health Qual Life Outcomes 19(1):171
Akça ÖF, Ağaç Vural T, Türkoğlu S, Kılıç EZ (2015) Anxiety sensitivity: changes with puberty and cardiovascular variables. Pediatr Int 57(1):49–54
Ge X, Conger RD, Elder GH (1996) Coming of age too early: pubertal influences on girls’ vulnerability to psychological distress. Child Dev 67(6):3386–3400
Pomerantz H, Parent J, Forehand R, Breslend NL, Winer JP (2017) Pubertal timing and youth internalizing psychopathology: the role of relational aggression. J Child Fam Stud 26(2)
Author information
Authors and Affiliations
Contributions
BK, ÖK, and MD designed and conducted this study. ÖK and MD undertook the statistical analyses. BK wrote the first draft of the manuscript. All authors have participated to drafting the manuscript; authors BK and MNÖ revised it critically. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted after approval from the University of Health Sciences Diyarbakır Gazi Yaşargil Training and Research Hospital Ethics Committee approval, dated 02.03.2018/36.The study was conducted in accordance with the Helsinki Declarations.
Consent to participate
N/A.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kardaş, B., Kardaş, Ö., Demiral, M. et al. Early puberty paradox: an investigation of anxiety levels of mothers and children, children’s quality of life, and psychiatric diagnoses. Eur J Pediatr 182, 3775–3783 (2023). https://doi.org/10.1007/s00431-023-05057-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05057-2