Abstract
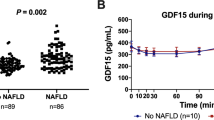
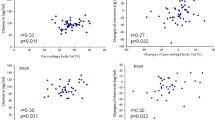
Obesity is a strong predictor for metabolic associated fatty liver disease (MAFLD), which has been associated with decreased insulin like growth factor 1 (IGF-1). In obesity, weight loss increases growth hormone secretion, but this is not unequivocally associated with increases in serum IGF-1 and IGF binding protein-3 (IGFBP-3). We studied the changes in the IGF axis in relation to weight loss and improvement in insulin resistance in children with or without MALFD after 10 weeks of lifestyle intervention at a weight loss camp (WLC). We investigated 113 (66 females) Caucasian children with obesity, median age 12.4 (range 7.3–14.6) years, before and after 10 weeks of lifestyle intervention at a WLC. We investigated children who was either MAFLD positive (n = 54) or negative (n = 59) before and after WLC. Children with MAFLD had lower baseline IGF-1 (249 ± 112 vs 278 ± 107 µg/l, P = 0.048), whereas the IGF-1/IGFBP-3 molar ratio was similar to children without MAFLD (19.4 ± 6.6 vs. 21.8 ± 6.6%, P = 0.108). When all children were considered as one group, WLC decreased SDS-BMI and HOMA-IR (P < 0.001, both) and increased IGF-1 (264 ± 110 vs 285 ± 108 µg/l, P < 0.001) and the IGF/IGFBP-3 molar ratio (20.7 ± 6.7 vs 22.4 ± 6.1%, P < 0.001). When categorized according to liver status, IGF-1 increased significantly in children with MAFLD (P = 0.008) and tended to increase in children without MAFLD (P = 0.052).
Conclusions: Ten weeks of lifestyle intervention decreased insulin resistance and improved the IGF axis. We observed slight differences in the IGF axis in relation to MAFLD status. This suggests that the IGF axis is primarily influenced by insulin resistance rather than MAFLD status.
What is New: • Weight loss decreases insulin resistance and subsequently increases the IGF axis in children with obesity. • Children with MAFLD had an aberration in the IGF axis compared to their MAFLD negative counter parts and the IGF axis was primarily influenced by the decreased BMI-SDS and insulin resistance, rather than MAFLD status. | |
What is Known: • NAFLD has previously been associated with reduced serum IGF-1 concentrations. • Data on the impact of MAFLD and aberrations in the growth hormone and IGF axis and the effects of lifestyle interventions in children are limited. |
Similar content being viewed by others
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OGTT:
-
2-h oral glucose tolerance test
- ALT:
-
Aminotransaminase
- BMI-SDS :
-
Body mass index standard deviation scores
- ELISA:
-
Enzyme-linked immunosorbent assay
- GGT:
-
Gamma-glutamyltransferase
- GH:
-
Growth hormone
- IGF-1:
-
Insulin-like growth factor-1
- IGFBPs:
-
IGF-binding proteins
- IGFBP-3:
-
IGF-binding protein-3
- IR:
-
Insulin resistance
- KIRA:
-
Kinase receptor activation
- MAFLD:
-
Metabolic-associated fatty liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- WLC:
-
Weight loss camp
References
Le Garf S, Nègre V, Anty R, Gual P (2021) Metabolic fatty liver disease in children: a growing public health problem. Biomedicines 9(12):1915. https://doi.org/10.3390/biomedicines9121915
Liu J, Mu C, Li K, Luo H, Liu Y, Li Z (2021) Estimating global prevalence of metabolic dysfunction-associated fatty liver disease in overweight or obese children and adolescents: systematic review and meta-analysis. Int J Public Health 66:1604371. https://doi.org/10.3389/ijph.2021.1604371
Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A (2017) Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol 23(47):8263–8276. https://doi.org/10.3748/wjg.v23.i47.8263
Eslam M, Alkhouri N, Vajro P, Baumann U, Weiss R, Socha P et al (2021) Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol Hepatol 6(10):864–873. https://doi.org/10.1016/s2468-1253(21)00183-7
Yan Y, Hou D, Zhao X, Liu J, Cheng H, Wang Y et al (2017) Childhood adiposity and nonalcoholic fatty liver disease in adulthood. Pediatrics 139(4). https://doi.org/10.1542/peds.2016-2738
Yang A, Cho SY, Kwak MJ, Kim SJ, Park SW, Jin DK et al (2019) Impact of BMI on peak growth hormone responses to provocative tests and therapeutic outcome in children with growth hormone deficiency. Sci Rep 9(1):16181. https://doi.org/10.1038/s41598-019-52644-1
Witkowska-Sędek E, Rumińska M, Stelmaszczyk-Emmel A, Majcher A, Pyrżak B (2018) The associations between the growth hormone/insulin-like growth factor-1 axis, adiponectin, resistin and metabolic profile in children with growth hormone deficiency before and during growth hormone treatment. Acta Biochim Pol 65(2):333–340. https://doi.org/10.18388/abp.2018_2601
Forrest L, Sedmak C, Sikder S, Grewal S, Harman SM, Blackman MR et al (2019) Effects of growth hormone on hepatic insulin sensitivity and glucose effectiveness in healthy older adults. Endocrine 63(3):497–506. https://doi.org/10.1007/s12020-018-01834-4
Dunger DB, Ahmed ML, Ong KK (2006) Early and late weight gain and the timing of puberty. Mol Cell Endocrinol 254–255:140–145. https://doi.org/10.1016/j.mce.2006.04.003
Bini V, Igli Baroncelli G, Papi F, Celi F, Saggese G, Falorni A (2004) Relationships of serum leptin levels with biochemical markers of bone turnover and with growth factors in normal weight and overweight children. Horm Res 61(4):170–175. https://doi.org/10.1159/000076134
Herndon DN, Ramzy PI, DebRoy MA, Zheng M, Ferrando AA, Chinkes DL et al (1999) Muscle protein catabolism after severe burn: effects of IGF-1/IGFBP-3 treatment. Ann Surg 229(5):713–20; discussion 20–2. https://doi.org/10.1097/00000658-199905000-00014
Xie S, Jiang R, Xu W, Chen Y, Tang L, Li L et al (2019) The relationship between serum-free insulin- like growth factor-1 and metabolic syndrome in school adolescents of northeast China. Diabetes Metab Syndr Obes 12:305–313. https://doi.org/10.2147/dmso.S195625
Duran-Ortiz S, Noboa V, Kopchick JJ (2020) Tissue-specific disruption of the growth hormone receptor (GHR) in mice: an update. Growth Horm IGF Res 51:1–5. https://doi.org/10.1016/j.ghir.2019.12.004
Frystyk J, Teran E, Gude MF, Bjerre M, Hjortebjerg R (2020) Pregnancy-associated plasma proteins and stanniocalcin-2 - novel players controlling IGF-I physiology. Growth Horm IGF Res 53–54:101330. https://doi.org/10.1016/j.ghir.2020.101330
Friedrich N, Wolthers OD, Arafat AM, Emeny RT, Spranger J, Roswall J et al (2014) Age- and sex-specific reference intervals across life span for insulin-like growth factor binding protein 3 (IGFBP-3) and the IGF-I to IGFBP-3 ratio measured by new automated chemiluminescence assays. J Clin Endocrinol Metab 99(5):1675–1686. https://doi.org/10.1210/jc.2013-3060
Chen JW, Ledet T, Orskov H, Jessen N, Lund S, Whittaker J et al (2003) A highly sensitive and specific assay for determination of IGF-I bioactivity in human serum. Am J Physiol Endocrinol Metab 284(6):E1149–E1155. https://doi.org/10.1152/ajpendo.00410.2002
Yao Y, Miao X, Zhu D, Li D, Zhang Y, Song C et al (2019) Insulin-like growth factor-1 and non-alcoholic fatty liver disease: a systemic review and meta-analysis. Endocrine 65(2):227–237. https://doi.org/10.1007/s12020-019-01982-1
Clemmons DR (2012) Metabolic actions of insulin-like growth factor-I in normal physiology and diabetes. Endocrinol Metab Clin North Am 41(2):425–43, vii-viii. https://doi.org/10.1016/j.ecl.2012.04.017
Gronbaek H, Lange A, Birkebaek NH, Holland-Fischer P, Solvig J, Horlyck A et al (2012) Effect of a 10-week weight loss camp on fatty liver disease and insulin sensitivity in obese Danish children. J Pediatr Gastroenterol Nutr 54(2):223–228. https://doi.org/10.1097/MPG.0b013e31822cdedf
Birkebaek NH, Lange A, Holland-Fischer P, Kristensen K, Rittig S, Vilstrup H et al (2010) Effect of weight reduction on insulin sensitivity, sex hormone-binding globulin, sex hormones and gonadotrophins in obese children. Eur J Endocrinol 163(6):895–900. https://doi.org/10.1530/eje-10-0538
Nysom K, Mølgaard C, Hutchings B, Michaelsen KF (2001) Body mass index of 0 to 45-y-old Danes: reference values and comparison with published European reference values. Int J Obes Relat Metab Disord 25(2):177–184. https://doi.org/10.1038/sj.ijo.0801515
Salgado AL, Carvalho L, Oliveira AC, Santos VN, Vieira JG, Parise ER (2010) Insulin resistance index (HOMA-IR) in the differentiation of patients with non-alcoholic fatty liver disease and healthy individuals. Arq Gastroenterol 47(2):165–169. https://doi.org/10.1590/s0004-28032010000200009
Bidlingmaier M, Friedrich N, Emeny RT, Spranger J, Wolthers OD, Roswall J et al (2014) Reference intervals for insulin-like growth factor-1 (IGF-I) from birth to senescence: results from a multicenter study using a new automated chemiluminescence IGF-I immunoassay conforming to recent international recommendations. J Clin Endocrinol Metab 99(5):1712–1721. https://doi.org/10.1210/jc.2013-3059
Peplies J, Jiménez-Pavón D, Savva SC, Buck C, Günther K, Fraterman A et al (2014) Percentiles of fasting serum insulin, glucose, HbA1c and HOMA-IR in pre-pubertal normal weight European children from the IDEFICS cohort. Int J Obes 38(S2):S39–S47. https://doi.org/10.1038/ijo.2014.134
Reinehr T, Panteliadou A, de Sousa G, Andler W (2009) Insulin-like growth factor-I, insulin-like growth factor binding protein-3 and growth in obese children before and after reduction of overweight. J Pediatr Endocrinol Metab 22(3):225–233. https://doi.org/10.1515/jpem.2009.22.3.225
Reinehr T, Bosse C, Lass N, Rothermel J, Knop C, Roth CL (2017) Effect of weight loss on puberty onset in overweight children. J Pediatr 184:143–50.e1. https://doi.org/10.1016/j.jpeds.2017.01.066
Yang HF, Lin XJ, Wang XH (2018) Effects of aerobic exercise plus diet control on serum levels of total IGF-1 and IGF-1 binding protein-3 in female obese youths and adolescents. Zhongguo Ying Yong Sheng Li Xue Za Zhi 34(1):78–82. https://doi.org/10.12047/j.cjap.5571.2018.020
Hagström H, Stål P, Hultcrantz R, Brismar K, Ansurudeen I (2017) IGFBP-1 and IGF-I as markers for advanced fibrosis in NAFLD - a pilot study. Scand J Gastroenterol 52(12):1427–1434. https://doi.org/10.1080/00365521.2017.1379556
Wang J, Li YC, Deng M, Jiang HY, Guo LH, Zhou WJ et al (2017) Serum insulin-like growth factor-1 and its binding protein 3 as prognostic factors for the incidence, progression, and outcome of hepatocellular carcinoma: a systematic review and meta-analysis. Oncotarget 8(46):81098–81108. https://doi.org/10.18632/oncotarget.19186
Acknowledgements
We thank the participants and the staff at Julemærkehjemmet Hobro for the collaboration during the study. Laboratory technician, Jane Hansen, Aarhus University Hospital, is thanked for helping drawing and processing all blood samples.
Funding
This work was supported by “Helsefonden, Denmark” and the Sanming Project of Medicine in Shenzhen (No. SZSM201612074) and Science and Technology Program of Shenzhen (No. JCYJ20190812164211151) of China.
Author information
Authors and Affiliations
Contributions
CW, HG, NB, JF, AH, and JS designed the study and collected data. NB, HG, KK, SR, and AL performed consultations. PHF performed consultation and reference of statistics. CW, DH, NB, JF, and HG analyzed the children’s data. JF did the IGF and IGFBP-3 analysis. CW and DH wrote the manuscript draft. JF supervised manuscript writing. All authors contributed important intellectual content and critically revised the manuscript. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haldrup, D., Wei, C., Holland-Fischer, P. et al. Effects of lifestyle intervention on IGF-1, IGFBP-3, and insulin resistance in children with obesity with or without metabolic-associated fatty liver disease. Eur J Pediatr 182, 855–865 (2023). https://doi.org/10.1007/s00431-022-04731-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04731-1