Abstract
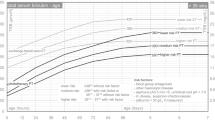
Neonatal jaundice is common and associated with delay in hospital discharge and risk of neurological sequelae if not treated. The objectives of the study were to report on our experience of the monitoring and treatment of neonatal jaundice in a home care setting and its feasibility and safety for neonates with high risk of severe hyperbilirubinemia. The 2-year study has been led in the greater Paris University Hospital At Home (Assistance Publique—Hôpitaux de Paris). The device of the intervention was the Bilicocoon® Bag, a light-emitting diode sleeping bag worn by the neonate when the total serum bilirubin value exceeds intensive phototherapy threshold, according to the guidelines from the American Academy of Pediatrics. One hundred and thirty-nine neonates had participated in the intervention and 39 (28%) were treated by phototherapy at home, as continuation of inpatient phototherapy or started at home. Seventy-five percent of the sample had more than two risk factors for development of severe hyperbilirubinemia. Twenty five percent of the cohort who received phototherapy at home had lower gestational age (p < 0.014) and had younger age at discharge from maternity (p < 0.09). Median length of stay in hospital at home was 5 days. Two patients needed readmission in conventional hospital (1%) for less than 24 h. In multivariate model, the length of stay decreased with the higher gestational age (p < 0.001) and increased significantly with the older age at discharge, the birth weight < 10th percentile, and a treatment by phototherapy at home.
Conclusion: Hospital at home, which is a whole strategy using an effective and convenient phototherapy device combined with a specialized medical follow-up, could be an alternative to conventional hospitalization for neonates at high risk of severe jaundice. The maternity discharge is facilitated, the mother-infant bonding can be promoted, and the risk of conventional rehospitalization is minimal, while guaranteeing the safety of this specific care.
What is Known: • Managing neonatal jaundice is provided in conventional hospital with phototherapy. • Neonatal jaundice increases the risk of prolonged hospitalization or readmission. | |
What is New: • Phototherapy is feasible in hospital at home for neonates with high risk of severe hyperbilirubinemia. • The care pathway of neonates from conventional hospital to hospital at home is described. |


Similar content being viewed by others
Availability of data and materials
Data are available. Some variables have been removed to ensure confidentiality.
Code availability
Analyses were performed with R. The script cannot be provided because it contains some data management parts with identifying variables. However, functions used in the script can be found in the repository: https://github.com/AlexandreGGS/R-statistics-functions (reference: https://pubmed.ncbi.nlm.nih.gov/30306900/).
Abbreviations
- AAP:
-
The American Academy of Pediatrics
- APHP:
-
Assistance Publique—Hôpitaux de Paris
- BIND:
-
Bilirubin-induced neurological dysfunctions
- CNRHP:
-
French National Reference Center in Perinatal Hemobiology
- G6PD:
-
Glucose-6 phosphate dehydrogenase
- LED:
-
Light-emitting diode
- PT:
-
Phototherapy
- SFN:
-
French Society of Neonatology
- SD:
-
Standard deviation
- TcB:
-
Transcutaneous bilirubin measurements
- TSB:
-
Total serum bilirubin level
References
Kaplan M, Muraca M, Hammerman C, Rubaltelli FF, Vilei MT, Vreman HJ, Stevenson DK (2002) Imbalance between production and conjugation of bilirubin: a fundamental concept in the mechanism of neonatal jaundice. Pediatrics 110(4):e47. https://doi.org/10.1542/peds.110.4.e47
Maisels MJ, McDonagh AF (2008) Phototherapy for neonatal jaundice. N Engl J Med 358(9):920–8. https://doi.org/10.1056/NEJMct0708376
Pan DH, Rivas Y (2017) Jaundice: newborn to age 2 months. Pediatr Rev 38(11):499–510. https://doi.org/10.1542/pir.2015-0132
Bhutani VK, Stark AR, Lazzeroni LC, Poland R, Gourley GR, Kazmierczak S, Meloy L, Burgos AE, Hall JY, Stevenson DK (2013) Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J Pediatr 162(3):477-482.e1. https://doi.org/10.1016/j.jpeds.2012.08.022
Cortey A, Renesme L, Raignoux J, Bedu A, Casper C, Tourneux P, Truffert P (2017) Management of jaundice in the newborn ≥ 35 GW: from screening to follow-up after discharge. Guidelines for clinical practice. Arch Pediatr 24(2):192–203. French. https://doi.org/10.1016/j.arcped.2016.11.011
Amos RC, Jacob H, Leith W (2016) Jaundice in newborn babies under 28 days: NICE guideline 2016 (CG98). Arch Dis Child Educ Pract Ed 102(4):207–209. https://doi.org/10.1136/archdischild-2016-311556
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia (2004) Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114(1):297–316. https://doi.org/10.1542/peds.114.1.297
Hansen TW (2000) Kernicterus in term and near-term infants-the specter walks again. Acta Paediatr 89(10):1155–1157. https://doi.org/10.1080/080352500750027484
Kaplan M, Bromiker R, Hammerman C (2011) Severe neonatal hyperbilirubinemia and kernicterus: are these still problems in the third millennium? Neonatology 100(4):354–362. https://doi.org/10.1159/000330055
Bhutani VK, Johnson L, Sivieri EM (1999) Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 103:6–14. https://doi.org/10.1542/peds.103.1.6
De Luca D, Carnielli VP, Paolillo P (2009) Neonatal hyperbilirubinemia and early discharge from the maternity ward. Eur J Pediatr 168:1025–1030. https://doi.org/10.1007/s00431-009-0969-1
Maisels MJ, Kring E (1998) Length of stay, jaundice, and hospital readmission. Pediatrics 101(6):995–998. https://doi.org/10.1542/peds.101.6.995
Seidman DS, Stevenson DK, Ergaz Z, Gale R (1995) Hospital readmission due to neonatal hyperbilirubinemia. Pediatrics 96(4 Pt 1):727–729 (PMID: 7567338)
Colletti JE, Kothari S, Jackson DM, Kilgore KP, Barringer K (2007) An emergency medicine approach to neonatal hyperbilirubinemia. Emerg Med Clin North Am 25(4):1117–35, vii. https://doi.org/10.1016/j.emc.2007.07.007
Bhutani VK, Committee on Fetus and Newborn American Academy of Pediatrics (2011) Phototherapy to prevent severe neonatal hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 128(4):e1046–e1052. https://doi.org/10.1542/peds.2011-1494
Ross G (2003) Hyperbilirubinemia in the 2000s: what should we do next? Am J Perinatol 20(8):415–424. https://doi.org/10.1055/s-2003-45385
De Luca D, Tridente A (2012) Efficacy of light-emitting diode versus other light sources for treatment of neonatal hyperbilirubinemia: a systematic review and meta-analysis. Acta Paediatr 101(5):458–65. https://doi.org/10.1111/j.1651-2227.2011.02561.x
Montealegre A, Charpak N, Parra A, Devia C, Coca I (2020) Bertolotto AM (2020) Effectiveness and safety of two phototherapy devices for the humanised management of neonatal jaundice. An Pediatr (Barc) 92(2):79–87
Noureldein M, Mupanemunda G, McDermott H, Pettit K, Mupanemunda R (2021) Home phototherapy for neonatal jaundice in the UK: a single-centre retrospective service evaluation and parental survey. BMJ Paediatr Open 5(1):e001027. https://doi.org/10.1136/bmjpo-2021-001027
NeoMedLight. BiliCocoon® (2021) NeoMedLight. https://www.neomedlight.com/bilicocoon. Accessed 2020
Kumar P, Murki S, Malik GK, Chawla D, Deorari AK, Karthi N, Subramanian S, Sravanthi J, Gaddam P, Singh SN (2010) Light emitting diodes versus compact fluorescent tubes for phototherapy in neonatal jaundice: a multi center randomized controlled trial. Indian Pediatr 47(2):131–137. https://doi.org/10.1007/s13312-010-0020-7
Kumar P, Chawla D, Deorari A (2011) Light-emitting diode phototherapy for unconjugated hyperbilirubinaemia in neonates. Cochrane Database Syst Rev 7(12):CD007969. https://doi.org/10.1002/14651858.CD007969.pub2
Mills JF, Tudehope D (20011) Fibreoptic phototherapy for neonatal jaundice. Cochrane Database Syst Rev 1:CD002060. https://doi.org/10.1002/14651858.CD002060
Briand-Huchet E, Tursz A, Revel C (2007) [New guidelines for care and investigation of sudden unexpected deaths in infant]. Arch Pediatr 14(6):633–5. French. https://doi.org/10.1002/14651858.CD007969.pub2
Luciano R, Mancini G, Cota F, Romano A, Purcaro V, Lerro F, Corsello M, Vento G (2019) New high intensity fibreoptic phototherapy devices in healthy newborns: a single pad wrapped around the neonate body in comparison with a double pad device. Ital J Pediatr 45(1):68. https://doi.org/10.1186/s13052-019-0663-5
Newman TB, Liljestrand P, Escobar GJ (2002) Jaundice noted in the first 24 hours after birth in a managed care organization. Arch Pediatr Adolesc Med 156(12):1244–1250. https://doi.org/10.1001/archpedi.156.12.1244
Newman TB, Xiong B, Gonzales VM, Escobar GJ (2000) Prediction and prevention of extreme neonatal hyperbilirubinemia in a mature health maintenance organization. Arch Pediatr Adolesc Med 154(11):1140–1147. https://doi.org/10.1001/archpedi.154.11.1140
Gale R, Seidman DS, Dollberg S, Stevenson DK (1990) Epidemiology of neonatal jaundice in the Jerusalem population. J Pediatr Gastroenterol Nutr 10(1):82–86. https://doi.org/10.1097/00005176-199001000-00016
Stevenson DK, Fanaroff AA, Maisels MJ, Young BW, Wong RJ, Vreman HJ, MacMahon JR, Yeung CY, Seidman DS, Gale R, Oh W, Bhutani VK, Johnson LH, Kaplan M, Hammerman C, Nakamura H (2001) Prediction of hyperbilirubinemia in near-term and term infants. Pediatrics 108(1):31–39. https://doi.org/10.1542/peds.108.1.31 (PMID: 11433051)
Rogerson AG, Grossman ER, Gruber HS, Boynton RC, Cuthbertson JG (1986) 14 years of experience with home phototherapy. Clin Pediatr (Phila) 25(6):296–299. https://doi.org/10.1177/000992288602500602
Eggert LD, Pollary RA, Folland DS, Jung AL (1985) Home phototherapy treatment of neonatal jaundice. Pediatrics 76(4):579–584 (PMID: 4047802)
Snook J (2017) Is home phototherapy in the term neonate with physiological jaundice a feasible practice? A systematic literature review. J Neonatal Nurs 23(1):28–39
Malwade US, Jardine LA (2014) Home- versus hospital-based phototherapy for the treatment of non-haemolytic jaundice in infants at more than 37 weeks’ gestation. Cochrane Neonatal Group, éditeur. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010212.pub2
Pettersson M, Eriksson M, Albinsson E, Ohlin A (2021) Home phototherapy for hyperbilirubinemia in term neonates - an unblinded multicentre randomized controlled trial. Eur J Pediatr 180:1603–1610
Acknowledgements
The authors thank Pr Pascal Boileau and Pr Jean Marie Jouannic for their great contribution to the proofreading of the manuscript. Authors also thank Aymeric Watine and Nesrine Belkadi Cheniki for their help in the redaction of the article.
Author information
Authors and Affiliations
Contributions
S.S.C contributed to the conception of the study design, prepared material, collected data, drafted the manuscript, and approved the final version. AG performed analysis and drafted the manuscript. He approved the final version of the manuscript. A.C. contributed to the study conception and design and she approved the final version of the manuscript. C.F. contributed to the study conception and design and she approved the final version of the manuscript. D.A. contributed to the study conception and design, collected data, and approved the final version of the manuscript. E.G. contributed to the study conception and design, collected data, and approved the final version of the manuscript. C.M.J. contributed to the study conception and design, drafted the manuscript, and approved the final version of the manuscript. M.D.S. contributed to the study conception and design, participated in the data analysis, drafted the manuscript, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Assistance Publique Hopitaux de Paris (APHP) ethical review board, Paris (n° 20210625102716).
Consent to participate
Written informed consent was obtained from the parents.
Consent for publication
Written informed consent was obtained from the parents.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Coquery, S.S., Georges, A., Cortey, A. et al. Discharge of newborns with risk factors of severe hyperbilirubinemia: description of a hospital at home-based care monitoring and phototherapy. Eur J Pediatr 181, 3075–3084 (2022). https://doi.org/10.1007/s00431-022-04461-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04461-4