Abstract
Purpose
Appendicitis is a common cause of acute abdominal pain, and treatment with laparoscopy has become increasingly common during the past two decades. Guidelines recommend that normal appendices are removed if operated for suspected acute appendicitis. It is unclear how many patients are affected by this recommendation. The aim of this study was to estimate the rate of negative appendectomies in patients undergoing laparoscopic surgery for suspected acute appendicitis.
Methods
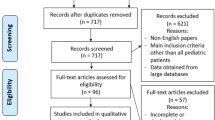
This study was reported following the PRISMA 2020 statement. A systematic search was conducted in PubMed and Embase for retrospective or prospective cohort studies (with n ≥ 100) including patients with suspected acute appendicitis. The primary outcome was the histopathologically confirmed negative appendectomy rate after a laparoscopic approach with a 95% confidence interval (CI). We performed subgroup analyses on geographical region, age, sex, and use of preoperative imaging or scoring systems. The risk of bias was assessed using the Newcastle-Ottawa Scale. Certainty of the evidence was assessed using GRADE.
Results
In total, 74 studies were identified, summing up to 76,688 patients. The negative appendectomy rate varied from 0% to 46% in the included studies (interquartile range 4–20%). The meta-analysis estimated the negative appendectomy rate to be 13% (95% CI 12–14%) with large variations between the individual studies. Sensitivity analyses did not change the estimate. The certainty of evidence by GRADE was moderate due to inconsistency in point estimates.
Conclusion
The overall estimated negative appendectomy rate after laparoscopic surgery was 13% with moderate certainty of evidence. The negative appendectomy rate varied greatly between studies.


Similar content being viewed by others
Data availability
Extracted data, bias assessment, and meta-analyses can be made available upon request to the corresponding author.
References
Wickramasinghe DP, Xavier C, Samarasekera DN (2021) The worldwide epidemiology of acute appendicitis: an analysis of the global health data exchange dataset. World J Surg 45:1999–2008. https://doi.org/10.1007/s00268
Stewart B, Khanduri P, McCord C et al (2014) Global disease burden of conditions requiring emergency surgery. Br J Surg 101:e9–e22. https://doi.org/10.1002/bjs.9329
Sartelli M, Baiocchi GL, Di Saverio S et al (2018) Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Med 13:19. https://doi.org/10.1186/s13017-018-0179-0
Jaschinski T, Mosch CG, Eikermann M et al (2018) Laparoscopic versus open surgery for suspected appendicitis. Cochrane database Syst Rev 11:CD001546. https://doi.org/10.1002/14651858.CD001546.pub4
Di Saverio S, Podda M, De Simone B et al (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Med 15:27. https://doi.org/10.1186/S13017-020-00306-3
Di Saverio S, Birindelli A, Kelly MD et al (2016) WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Med 11:34. https://doi.org/10.1186/S13017-016-0090-5
Andersson RE, Hugander A, Thulin AJG (1992) Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg 158:37–41
Emre A, Akbulut S, Bozdag Z et al (2013) Routine histopathologic examination of appendectomy specimens: retrospective analysis of 1255 patients. Int Surg 98:354–362. https://doi.org/10.9738/INTSURG-D-13-00098.1
Allaway MGR, Eslick GD, Cox MR (2019) The unacceptable morbidity of negative laparoscopic appendicectomy. World J Surg 43:405–414. https://doi.org/10.1007/S00268-018-4784-6
Knaapen M, van Amstel P, van Amstel T et al (2021) Outcomes after appendectomy in children with acute appendicitis treated at a tertiary paediatric centre: results from a retrospective cohort study. Langenbeck’s Arch Surg 406:163–169. https://doi.org/10.1007/s00423-020-01976-y
Luksaite-Lukste R, Kliokyte R, Samuilis A et al (2021) Conditional CT strategy—an effective tool to reduce negative appendectomy rate and the overuse of the CT. J Clin Med 10:2456. https://doi.org/10.3390/jcm10112456
Photi E, Barker S, Kapur S, Shaikh I (2017) Diagnosis and management of acute abdominal pain in young young females. Colorectal Dis 19:67–68. https://doi.org/10.1111/CODI.13798
Lu Y, Friedlander S, Lee SL (2016) Negative appendectomy: clinical and economic implications. Am Surg 82:1018–1022. https://doi.org/10.1177/000313481608201036
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88:105906. https://doi.org/10.1016/J.IJSU.2021.105906
Henriksen SR, Christophersen C, Rosenberg J, Fonnes S (2022) PROSPERO protocol – negative appendectomy rate after laparoscopic appendectomy: a systematic review. CRD42022331928. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022331928. Accessed 22 Nov 2022
Greenhalgh T, Peacock R (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331:1064–1065. https://doi.org/10.1136/bmj.38636.593461.68
Elsevier, Mendeley reference manager. https://www.mendeley.com/reference-manager/. Accessed 22 Nov 2022
Veritas Health Innovation, Covidence systematic review management. https://www.covidence.org/. Accessed 22 Nov 2022
United Nations Statistics Division. Standard country or area codes for statistical use. https://unstats.un.org/unsd/methodology/m49/. Accessed 22 nov 2022
Wells GA, Shea B, O’Connell D, et al The Newcastle-Ottawa Scale for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 22 Nov 2022
Brown University, OpenMeta[Analyst]. http://www.cebm.brown.edu/openmeta/. Accessed 22 Nov 2022
Migliavaca CB, Stein C, Colpani V et al (2022) Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity. Res Synth Methods 13:363–367. https://doi.org/10.1002/JRSM.1547
The GRADE Working Group (2013) GRADE handbook for grading quality of evidence and strength of recommendations. https://gdt.gradepro.org/app/handbook/handbook.html. Accessed 22 Nov 2022
McMaster University and Evidence Prime (2022) GRADEpro Guideline Development Tool. https://www.gradepro.org/. Accessed 22 Nov 2022
Iorio A, Spencer FA, Falavigna M et al (2015) Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ 350:h870. https://doi.org/10.1136/BMJ.H870
Noureldin K, Ali AAH, Issa M et al (2022) Negative appendicectomy rate: incidence and predictors. Cureus 14:e21489. https://doi.org/10.7759/cureus.21489
Noureldin K, Ayantunde A, Elkholy M et al (2021) Evaluating the rate, the predictors and the outcomes of patients with negative appendectomy(NAR). Br J Surg 108(suppl):2. https://doi.org/10.1093/bjs/znab134.530
Horst KK, Kolbe AB, McDonald JS et al (2021) Imaging pediatric acute appendicitis during the coronavirus disease 2019 (COVID-19) pandemic: collateral damage is variable. Pediatr Radiol 51:1991–1999. https://doi.org/10.1007/s00247-021-05128-2
Kim CW, Lee S-H (2021) Impact of COVID-19 on the care of acute appendicitis: a single-center experience in Korea. Ann Surg Treat Res 101:240–246. https://doi.org/10.4174/astr.2021.101.4.240
Meyer T (2021) Auswirkung der COVID-19-Pandemie auf die Appendizitis bei COVID-19-negativen Kindern. Monatsschr Kinderheilkd 169:633–638. https://doi.org/10.1007/s00112-021-01161-5
Orban YA, Algazar M, Farag A, Elalfy TR (2021) Do we still encounter non-appendicitis pathologies during laparoscopic appendectomy? World 14:10–14. https://doi.org/10.5005/jp-journals-10033-1432
Pringle HCM, Donigiewicz U, Bennett M-R et al (2021) Appendicitis during the COVID-19 pandemic: lessons learnt from a district general hospital. BMC Surg 21:242. https://doi.org/10.1186/s12893-021-01231-1
Qin RX, Yen DLA (2021) Do the “Eyes” have it? How good are surgeons at identifying appendicitis macroscopically? A retrospective study in New Zealand. N Z Med J 134:55–62
Scheijmans JCG, Borgstein ABJ, Puylaert CAJ et al (2021) Impact of the COVID-19 pandemic on incidence and severity of acute appendicitis: a comparison between 2019 and 2020. BMC Emerg Med 21:61. https://doi.org/10.1186/s12873-021-00454-y
So CP, Bradley N, Crumley ABC, Wilson MSJ (2021) Negative appendicectomy rate and role of biomarkers in predicting the severity of acute appendicitis. Br J Surg 108:7. https://doi.org/10.1093/BJS/ZNAB312.043
Somers K, Elwahab SA, Raza MZ et al (2021) Impact of the COVID-19 pandemic on management and outcomes in acute appendicitis: should these new practices be the norm? Surgeon 19:e310–e317. https://doi.org/10.1016/j.surge.2021.01.009
Yeh DD, Eid AI, Young KA et al (2021) Multicenter study of the treatment of appendicitis in America. Ann Surg 273:548–556. https://doi.org/10.1097/SLA.0000000000003661
Noureldin K, Elkhouly M, Shah H et al (2021) Evaluating the incidence, the predictors and the outcomes of patients with negative appendicectomy. Br J Surg 108(7). https://doi.org/10.1093/bjs/znab362.104
Dezfuli SAT, Yazdani R, Khorasani M, Hosseinikhah SA (2019) Comparison between the specificity and sensitivity of the RIPASA and Alvarado scoring systems in the diagnosis of acute appendicitis among patients with complaints of right iliac fossa. AIMS Public Health 7:1–9. https://doi.org/10.3934/publichealth.2020001
Fan SM, Grigorian A, Smith BR et al (2020) Geriatric patients undergoing appendectomy have increased risk of intraoperative perforation and/or abscess. Surgery 168:322–327. https://doi.org/10.1016/j.surg.2020.04.019
Foley MP, MacLean M, Doyle C et al (2020) Factors influencing surgical management of acute appendicitis in a large university hospital without a dedicated emergency theatre. Ir J Med Sci 189:649–653. https://doi.org/10.1007/s11845-019-02135-z
Fonseca MK, Trindade EN, Filho OPC et al (2020) Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am Surg 86:1508–1512. https://doi.org/10.1177/0003134820972098
Gelpke K, Hamminga JTH, van Bastelaar JJ et al (2020) Reducing the negative appendectomy rate with the laparoscopic appendicitis score; a multicenter prospective cohort and validation study. Int J Surg 79:257–264. https://doi.org/10.1016/j.ijsu.2020.04.041
Gronroos J, Konstantinou C (2020) Accuracy of intraoperative diagnosis of appendicitis in laparoscopy. Should this affect decision for appendicectomy. Br J Surg 107:199. https://doi.org/10.1002/bjs.11642
Hajuthman W, Cyriac C, Seitler S et al (2020) Trends & outcomes in paediatric appendicectomy. Colorectal Dis 22:13–64. https://doi.org/10.1111/codi.15169
Hamer J, Bhasin S, Wilkinson B, Singh-ranger D (2020) Acute appendicitis management: does gender matter? A retrospective study. Colorectal Dis 22:57. https://doi.org/10.1111/CODI.15169
Bhasin S, Hamer J, Wilkinson B et al (2020) Acute appendicitis management: does gender matter? A single centre retrospective study. Br J Surg 107:116. https://doi.org/10.1002/bjs.12069
Kabir SMU, Bucholc M, Walker C-A et al (2020) Quality outcomes in appendicitis care: identifying opportunities to improve care. Life 10:358. https://doi.org/10.3390/life10120358
Alotaibi AM, Moshref LH, Moshref RH, Felemban LS (2021) Analysis of 190 female patients after appendectomy. Obstet Gynecol Int 2021:8036970. https://doi.org/10.1155/2021/8036970
Keohane D, O’Leary P, Nagle M et al (2020) A correlation of blood panel results and histologically confirmed appendicitis. Cureus 12:e10641. https://doi.org/10.7759/cureus.10641
Khan MH, Sultana J, Ahsan T, Ahsan SA (2020) Role of laparoscopic appendicectomy in the treatment of acute appendicitis and its complications. Mymensingh Med J 29:887–894
Kim JJY, Dobson BH, Ng CLH et al (2020) Can normal inflammatory markers rule out acute appendicitis? The reliability of biochemical investigations in diagnosis. ANZ J Surg 90:1970–1974. https://doi.org/10.1111/ans.15559
Knotts CM, Prange EJ, Orminski K et al (2020) The provision of acute pediatric surgical care by adult acute care general surgeons. Am Surg 86:1640–1646. https://doi.org/10.1177/0003134820933251
Kuhlenschmidt KM, Houshmand N, Comish PB et al (2020) Pathology is a better predictor of outcomes than operative surgeon. J Am Coll Surg 231:e134. https://doi.org/10.1016/j.jamcollsurg.2020.08.351
Mackay TG, Dissanayake B, Yuide PJ et al (2020) Cohort study of 1241 patients to identify predictors of negative appendicectomy. ANZ J Surg 90:1984–1990. https://doi.org/10.1111/ans.16203
Mahendran V, El-Houssari T (2020) Underestimated tools in predicting acute appendicitis: a retrospective observational study on lymphocyte ratios, neutrophil count and CRP. Colorectal Dis 22:21–22. https://doi.org/10.1111/CODI.15169
Rait JS, Ajzajian J, McGillicuddy J et al (2020) Acute appendicitis and the role of pre-operative imaging: a cohort study. Ann Med Surg 59:258–263. https://doi.org/10.1016/j.amsu.2020.10.008
RIFT Study Group (2020) Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg 107:73–86. https://doi.org/10.1002/bjs.11440
Tamini N, Santurro L, Chiappetta MF et al (2020) Morbidity after negative appendectomy: a single-centre experience on 627 cases. Eur J Trauma Emerg Surg 46:859–864. https://doi.org/10.1007/s00068-019-01138-w
Antakia R, Xanthis A, Georgiades F et al (2021) Acute appendicitis management during the COVID-19 pandemic: a prospective cohort study from a large UK centre. Int J Surg 86:32–37. https://doi.org/10.1016/j.ijsu.2020.12.009
Wagner PDJ, Haroon M, Morarasu S et al (2020) Does CT reduce the rate of negative laparoscopies for acute appendicitis? A single-center retrospective study. J Med Life 13:26–31. https://doi.org/10.25122/jml-2019-0099
Zaman S, Amada H, Bhattacharya P et al (2020) Peri-operative management of acute appendicitis: a re-audit. Br J Surg 107:203. https://doi.org/10.1002/BJS.11642
Aljoe J, Enoch J, Ferguson JS (2019) Diagnosis of acute appendicitis and clinical outcomes following laparoscopic surgery: a cohort study. ANZ J Surg 89:1437–1440. https://doi.org/10.1111/ans.15464
Allaway MGR, Eslick GD, Kwok GTY, Cox MR (2017) The established acute surgical unit: a reduction in nighttime appendicectomy without increased morbidity. Int J Surg 43:81–85. https://doi.org/10.1016/J.IJSU.2017.05.045
Childers CP, Dworsky JQ, Maggard-Gibbons M, Russell MM (2019) The contemporary appendectomy for acute uncomplicated appendicitis in adults. Surgery 165:593–601. https://doi.org/10.1016/j.surg.2018.09.009
Guthrie GJ, Johnston T, Ewing A et al (2019) A prospective observational study of the utility of early diagnostic laparoscopy for right lower abdominal pain: a safe and effective diagnostic and therapeutic tool. Scott Med J 64:49–55. https://doi.org/10.1177/0036933016649869
Jones RE, Gee KM, Preston SC et al (2019) Diagnostic utilization and accuracy of pediatric appendicitis imaging at adult and pediatric centers. J Surg Res 240:97–103. https://doi.org/10.1016/j.jss.2019.02.047
Kliuchanok K, Keßler W, Partecke I et al (2019) A comparison of non-absorbable polymeric clips and staplers for laparoscopic appendiceal stump closure: analysis of 618 adult patients. Langenbeck’s Arch Surg 404:711–716. https://doi.org/10.1007/s00423-019-01814-w
Lansdale N, Fryer S, Stockdale M et al (2019) Prospective evaluation of a clinical response directed pathway for complicated appendicitis. J Pediatr Surg 54:272–275. https://doi.org/10.1016/j.jpedsurg.2018.10.082
Lima M, Persichetti-Proietti D, Di Salvo N et al (2019) The appendicitis pediatric (APPE) score: a new diagnostic tool in suspected pediatric acute appendicitis. Pediatr Med Chir 41:10–16. https://doi.org/10.4081/pmc.2019.209
Eamer G, Turnbull V, Robinson T et al (2021) Cost effectiveness of the quality assurance and performance improvement project for suspected appendicitis study. J Pediatr Surg 56:1528–1535. https://doi.org/10.1016/j.jpedsurg.2020.09.006
López JRG, del Olmo JCM, Martín MAM et al (2019) Laparoscopic appendectomy in the setting of clinical prediction rules. J Laparoendosc Adv Surg Tech 29:184–191. https://doi.org/10.1089/lap.2018.0707
Thong DW, Crouch S, Morgan S, Arthur T (2019) Can surgeons identify appendicitis macroscopically? Results from a multicentre prospective study. Surg Laparosc Endosc Percutan Tech 29:344–348. https://doi.org/10.1097/SLE.0000000000000687
Zosimas D, Lykoudis PM, Burke J et al (2019) Postoperative outcomes in laparoscopic appendicectomies with histopathologically normal appendix. Ann Ital Chir 90:72–77
Zosimas D, Lykoudis P, Pilavas A et al (2018) Open versus laparoscopic appendicectomy in acute appendicitis: results of a district general hospital. S Afr J Surg 56:59–63. https://doi.org/10.17159/2078-5151/2018/v56n2a2392
Ali MT, Saleem MR, Sajid M, Ansari H (2018) Causes of perforated appendicitis and its prevalence in patients whom undergone appendectomy. Pakistan J Med Heal Sci 12:900–902
Augustin G, Čižmešija Z, Žedelj J et al (2018) Laparoscopic appendectomy does not increase the rate of negative appendectomy along with a lower rate of perforated appendicitis – results in 1899 patients at Zagreb UHC. Acta Clin Croat 57:503–509. https://doi.org/10.20471/acc.2018.57.03.14
Bolmers M, van Rossem C, Gorter R et al (2018) Imaging in pediatric appendicitis is key to a low normal appendix percentage: a national audit on the outcome of appendectomy for appendicitis in children. Pediatr Surg Int 34:543–551. https://doi.org/10.1007/s00383-018-4244-2
Boshnak N, Boshnaq M, Elgohary H (2018) Evaluation of platelet indices and red cell distribution width as new biomarkers for the diagnosis of acute appendicitis. J Invest Surg 31:121–129. https://doi.org/10.1080/08941939.2017.1284964
D’Souza N, Marsden M, Bottomley S et al (2018) Cost-effectiveness of routine imaging of suspected appendicitis. Ann R Coll Surg Engl 100:47–51. https://doi.org/10.1308/rcsann.2017.0132
de Burlet KJ, Crane G, Cullinane R et al (2018) Review of appendicectomies over a decade in a tertiary hospital in New Zealand. ANZ J Surg 88:1253–1257. https://doi.org/10.1111/ans.14203
Fuentes EJ, Pérez EA, Díez R et al (2021) Use of hem-o-lok clips for laparoscopic appendectomy in children: retrospective analysis and comparison to ligature loop and endoscopic surgical stapler. Transl Gastroenterol Hepatol 6:44. https://doi.org/10.21037/tgh-20-213
Dumas RP, Subramanian M, Hodgman E et al (2018) Laparoscopic appendectomy: a report on 1164 operations at a single-institution, safety-net hospital. Am Surg 84:1110–1116. https://doi.org/10.1177/000313481808400674
Er S, Çomçalı B, Soykurt A et al (2018) Diagnosis of appendicitis in patients with a normal white blood cell count; a cross-sectional study. Bull Emerg trauma 6:128–132. https://doi.org/10.29252/beat-060207
Khan A, Riaz M, Kelly ME et al (2018) Prospective validation of neutrophil-to-lymphocyte ratio as a diagnostic and management adjunct in acute appendicitis. Ir J Med Sci 187:379–384. https://doi.org/10.1007/s11845-017-1667-z
McGrath R, Mustafa H, Khodear Y et al (2018) An evaluation of the impact of a dedicated emergency surgical service on the management and outcomes of acute appendicitis. Ir J Med Sci 187:S148–S149. https://doi.org/10.1007/s11845-018-1861-7
Almström M, Svensson JF, Patkova B et al (2017) In-hospital surgical delay does not increase the risk for perforated appendicitis in children. Ann Surg 265:616–621. https://doi.org/10.1097/SLA.0000000000001694
Arthur T, Gartrell R, Manoharan B, Parker D (2017) Emergency appendicectomy in Australia: findings from a multicentre, prospective study. ANZ J Surg 87:656–660. https://doi.org/10.1111/ans.14088
Blane C, Fordham T, Howes N, Richards S (2017) Contaminated appendicitis – is irrigation a habit or a requirement? Int J Surg 47:535. https://doi.org/10.1016/j.ijsu.2017.08.189
Borissova A, Hotouras A, Hotouras PH et al (2017) Should all patients with suspected appendicitis undergo computed tomography? Colorectal Dis 19:35–139. https://doi.org/10.1111/CODI.13798
Brideaux A, Khan S, Denby E et al (2017) Acute appendicitis: a single centre review of pre-surgical diagnostic imaging in patients who proceeded to appendicectomy. J Med Imaging Radiat Oncol 61:138–197. https://doi.org/10.1111/1754-9485.12657
Khan S, Brideaux A, Denby E et al (2017) The quality use of imaging to prevent unnecessary surgery: an evaluation of patient morbidity and healthcare costs as a result of negative laparoscopic appendicectomies. J Med Imaging Radiat Oncol 61:21. https://doi.org/10.1111/1754-9485.12656
Hammett F, Ali S, Adair R et al (2021) Long term outcomes after resection of a “normal” appendix. Br J Surg 108:2. https://doi.org/10.1093/bjs/znab134.214
Jeon BG (2017) Predictive factors and outcomes of negative appendectomy. Am J Surg 213:731–738. https://doi.org/10.1016/j.amjsurg.2016.05.020
McKinlay L, Gray J (2017) The negative appendicectomy rate: a new gender gap? J R Coll Physicians Edinb 104:173. https://doi.org/10.1002/bjs.10634
Segev L, Segev Y, Rayman S et al (2017) Acute appendicitis during pregnancy: different from the nonpregnant state? World J Surg 41:75–81. https://doi.org/10.1007/s00268-016-3731-7
Shuaib A, Shuaib A, Fakhra Z et al (2017) Evaluation of modified Alvarado scoring system and RIPASA scoring system as diagnostic tools of acute appendicitis. World J Emerg Med 8:276. https://doi.org/10.5847/wjem.j.1920-8642.2017.04.005
Tind S, Qvist N (2017) Acute appendicitis: a weak concordance between perioperative diagnosis, pathology and peritoneal fluid cultivation. World J Surg 41:70–74. https://doi.org/10.1007/s00268-016-3686-8
Yaşar NF, Uylaş MU, Ateş E et al (2017) Is laparoscopy superior than open surgery in finding unexpected pathologies in negative appendectomies? Med J Bakirköy 13:118–121. https://doi.org/10.5350/BTDMJB201713302
Hannan E, El-Masry S (2021) The impact of the acute surgical assessment unit on the management of acute appendicitis: a single-centre review. Ir J Med Sci 191:1361–1367. https://doi.org/10.1007/s11845-021-02706-z
Heise JW, Kentrup H, Dietrich CG et al (2021) Laparoscopic appendectomy: a safe and definitive solution for suspected appendicitis. Visc Med 37:180–188. https://doi.org/10.1159/000510487
Vuille-Dit-Bille RN, Staerkle RF, Derderian SC et al (2020) Appendiceal stump closure in children using polymeric clips is a reliable alternative to endoloops. Minerva Chir 75:274–275. https://doi.org/10.23736/S0026-4733.20.08313-3
Guy S, Wysocki P (2018) Risk factors for intra-abdominal abscess post laparoscopic appendicectomy for gangrenous or perforated appendicitis: a retrospective cohort study. Int J Surg Open 10:47–54. https://doi.org/10.1016/j.ijso.2017.12.003
Jamil M, Ahmed A, Qamar A et al (2018) Is laparoscopic appendectomy better choice compared to open appendectomy. Rawal Med J 43:301–305
Strong S, Blencowe N, Bhangu A et al (2015) How good are surgeons at identifying appendicitis? Results from a multi-centre cohort study. Int J Surg 15:107–112. https://doi.org/10.1016/J.IJSU.2015.01.032
Sørensen AK, Bang-Nielsen A, Levic-Souzani K et al (2019) Readmission and reoperation rates following negative diagnostic laparoscopy for clinically suspected appendicitis: the “normal” appendix should not be removed – a retrospective cohort study. Int J Surg 64:1–4. https://doi.org/10.1016/j.ijsu.2019.02.001
Van Den Broek WT, Bijnen AB, De Ruiter P, Gouma DJ (2000) A normal appendix found during diagnostic laparoscopy should not be removed. Br J Surg 88:251–254. https://doi.org/10.1046/j.1365-2168.2001.01668.x
El-Gohary Y, Molina M, Chang J et al (2021) The use of computed tomography versus clinical acumen in diagnosing appendicitis in children: a two-institution international study. J Pediatr Surg 56:1356–1361. https://doi.org/10.1016/J.JPEDSURG.2020.09.061
Sallinen V, Akl EA, You JJ et al (2016) Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg 103:656–667. https://doi.org/10.1002/bjs.10147
Yang Z, Sun F, Ai S et al (2019) Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg 19:110. https://doi.org/10.1186/s12893-019-0578-5
Author information
Authors and Affiliations
Contributions
Siri Rønholdt Henriksen: conceptualisation, formal analysis, methodology, writing – original draft
Camilla Christophersen: conceptualisation, writing – review and editing
Jacob Rosenberg: conceptualisation, writing – review and editing, supervision
Siv Fonnes: conceptualisation, methodology, writing – review and editing, project administration, visualisation
Corresponding author
Ethics declarations
Ethical approval
PROSPERO registration ID: CRD42022331928; access to the protocol available through https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022331928.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 2035 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Henriksen, S.R., Christophersen, C., Rosenberg, J. et al. Varying negative appendectomy rates after laparoscopic appendectomy: a systematic review and meta-analysis. Langenbecks Arch Surg 408, 205 (2023). https://doi.org/10.1007/s00423-023-02935-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02935-z