Abstract
Purpose
The use of synthetic mesh to repair infected abdominal wall defects remains controversial. Polyvinylidene fluoride (PVDF) mesh was introduced in 2002 as an alternative to polypropylene, with the advantages of improved biostability, lowered bending stiffness, and minimum tissue response. This study aimed to evaluate the short-term outcomes of using PVDF mesh to treat infected abdominal wall defects in the elective setting.
Methods
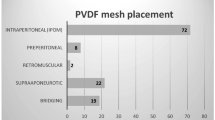
This prospective clinical trial started in 2016 and was designed to evaluate the short- and mid-term outcomes of 38 patients submitted to abdominal wall reconstruction in the setting of active mesh infection and/or enteric fistulas (AI) when compared to a group of 38 patients submitted to clean ventral hernia repairs (CC). Patients were submitted to single-staged repairs, using onlay PVDF mesh (DynaMesh®—CICAT) reinforcement to treat their defects.
Results
Groups had comparable demographic characteristics. The AI group had more previous abdominal operations and required a longer operative and anesthesia time. At 30 days, surgical site occurrences were observed in 16 (42.1%) AI vs. 17 (44.7%) CC, p = 0.817; surgical site infection occurred in 4 (10.5%) AI vs. 6 (15.8%) CC, p = 0.497; and a higher number of procedural interventions were required in the CC group, 15.8 AI vs. 28.9% CC, p = 0.169. Both groups did not have chronic infections at 1 year of follow-up, and one hernia recurrence was observed in the AI group.
Conclusions
The use of PVDF mesh in the infected setting presented favorable results with a low incidence of wound infection.

Similar content being viewed by others
References
Hodgkinson JD, Maeda Y, Leo CA et al (2017) Complex abdominal wall reconstruction in the setting of active infection and contamination: a systematic review of hernia and fistula recurrence rates. Colorectal Dis 19:319–330. https://doi.org/10.1111/codi.13609
Birolini C, de Miranda JS, Utiyama EM, Rasslan S (2015) A retrospective review and observations over a 16-year clinical experience on the surgical treatment of chronic mesh infection. What about replacing a synthetic mesh on the infected surgical field? Hernia 19:239–246. https://doi.org/10.1007/s10029-014-1225-9
Birolini C, de Miranda JS, Tanaka EY et al (2020) The use of synthetic mesh in contaminated and infected abdominal wall repairs: challenging the dogma-a long-term prospective clinical trial. Hernia 24:307–323. https://doi.org/10.1007/s10029-019-02035-2
Klinge U, Klosterhalfen B, Ottinger AP et al (2002) PVDF as a new polymer for the construction of surgical meshes. Biomaterials 23:3487–3493. https://doi.org/10.1016/s0142-9612(02)00070-4
Klink CD, Junge K, Binnebösel M et al (2011) Comparison of long-term biocompability of PVDF and PP meshes. J Invest Surg 24:292–299. https://doi.org/10.3109/08941939.2011.589883
Berger D, Bientzle M (2009) Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia 13:167–172. https://doi.org/10.1007/s10029-008-0435-4
Sommer T, Friis-Andersen H (2013) DynaMesh® in the repair of laparoscopic ventral hernia: a prospective trial. Hernia 17:613–618. https://doi.org/10.1007/s10029-013-1090-y
Barski D, Arndt C, Gerullis H et al (2017) Transvaginal PVDF-mesh for cystocele repair: a cohort study. Int J Surg 39:249–254. https://doi.org/10.1016/j.ijsu.2017.02.006
Alemrajabi M, Darabi B, Banivaheb B et al (2020) Polyvinylidene fluoride mesh use in laparoscopic ventral mesh rectopexy in patients with obstructive defecation syndrome for the first time. J Invest Surg 1–6. https://doi.org/10.1080/08941939.2020.1767734
Sánchez-Arteaga A, Tallón-Aguilar L, Tinoco-González J et al (2021) Use of polyvinylidene fluoride (PVDF) meshes for ventral hernia repair in emergency surgery. Hernia 25:99–106. https://doi.org/10.1007/s10029-020-02209-3
Garner JS (1986) CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in November 1985). Revised. Infect Control 7:193–200
Muysoms F, Campanelli G, Champault GG et al (2012) EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia 16:239–250. https://doi.org/10.1007/s10029-012-0912-7
Tanaka EY, Yoo JH, Rodrigues AJ et al (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14:63–69. https://doi.org/10.1007/s10029-009-0560-8
Haskins IN, Horne CM, Krpata DM et al (2018) A call for standardization of wound events reporting following ventral hernia repair. Hernia 22:729–736. https://doi.org/10.1007/s10029-018-1748-6
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Shubinets V, Carney MJ, Colen DL et al (2018) Management of infected mesh after abdominal hernia repair: systematic review and single-institution experience. Ann Plast Surg 80:145–153. https://doi.org/10.1097/SAP.0000000000001189
Warren J, Desai SS, Boswell ND et al (2020) Safety and efficacy of synthetic mesh for ventral hernia repair in a contaminated field. J Am Coll Surg 230:405–413. https://doi.org/10.1016/j.jamcollsurg.2019.12.008
Rosen MJ, Krpata DM, Petro CC et al (2022) Biologic vs synthetic mesh for single-stage repair of contaminated ventral hernias: a randomized clinical trial. JAMA Surg 157:293–301. https://doi.org/10.1001/jamasurg.2021.6902
Majumder A, Winder JS, Wen Y et al (2016) Comparative analysis of biologic versus synthetic mesh outcomes in contaminated hernia repairs. Surgery 160:828–838. https://doi.org/10.1016/j.surg.2016.04.041
Lee L, Mata J, Landry T et al (2014) A systematic review of synthetic and biologic materials for abdominal wall reinforcement in contaminated fields. Surg Endosc 28:2531–2546. https://doi.org/10.1007/s00464-014-3499-5
Atema JJ, de Vries FEE, Boermeester MA (2016) Systematic review and meta-analysis of the repair of potentially contaminated and contaminated abdominal wall defects. Am J Surg 212:982-995.e1. https://doi.org/10.1016/j.amjsurg.2016.05.003
Sadava EE, Bras Harriott C, Angeramo CA, Schlottmann F (2021) Synthetic mesh in contaminated abdominal wall surgery: friend or foe? A literature review. J Gastrointest Surg. https://doi.org/10.1007/s11605-021-05155-2
Köckerling F, Alam NN, Antoniou SA et al (2018) What is the evidence for the use of biologic or biosynthetic meshes in abdominal wall reconstruction? Hernia 22:249–269. https://doi.org/10.1007/s10029-018-1735-y
Carbonell AM, Criss CN, Cobb WS et al (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 217:991–998. https://doi.org/10.1016/j.jamcollsurg.2013.07.382
Laroche G, Marois Y, Schwarz E et al (1995) Polyvinylidene fluoride monofilament sutures: can they be used safely for long-term anastomoses in the thoracic aorta? Artif Organs 19:1190–1199. https://doi.org/10.1111/j.1525-1594.1995.tb02282.x
Conze J, Junge K, Weiss C et al (2008) New polymer for intra-abdominal meshes–PVDF copolymer. J Biomed Mater Res Part B Appl Biomater 87:321–328. https://doi.org/10.1002/jbm.b.31106
Kallinowski F, Baumann E, Harder F et al (2015) Dynamic intermittent strain can rapidly impair ventral hernia repair. J Biomech 48:4026–4036. https://doi.org/10.1016/j.jbiomech.2015.09.045
Groene SA, Prasad T, Lincourt AE et al (2016) Prospective, multi-institutional surgical and quality-of-life outcomes comparison of heavyweight, midweight, and lightweight mesh in open ventral hernia repair. Am J Surg 212:1054–1062. https://doi.org/10.1016/j.amjsurg.2016.09.003
Bakker WJ, Aufenacker TJ, Boschman JS, Burgmans JPJ (2021) Heavyweight mesh is superior to lightweight mesh in laparo-endoscopic inguinal hernia repair: a meta-analysis and trial sequential analysis of randomized controlled trials. Ann Surg 273:890–899. https://doi.org/10.1097/SLA.0000000000003831
Birolini C, Utiyama EM, Rodrigues AJ, Birolini D (2000) Elective colonic operation and prosthetic repair of incisional hernia: does contamination contraindicate abdominal wall prosthesis use? J Am Coll Surg 191:366–372. https://doi.org/10.1016/s1072-7515(00)00703-1
Lima HVG, Rasslan R, Novo FCF et al (2020) Prevention of fascial dehiscence with onlay prophylactic mesh in emergency laparotomy: a randomized clinical trial. J Am Coll Surg 230:76–87. https://doi.org/10.1016/j.jamcollsurg.2019.09.010
Dilek ON, Güler O, Güler AA et al (2001) Prophylactic appendectomy: is it worth to be done? Acta Chir Belg 101:65–67
Newhall K, Albright B, Tosteson A et al (2017) Cost-effectiveness of prophylactic appendectomy: a Markov model. Surg Endosc 31:3596–3604. https://doi.org/10.1007/s00464-016-5391-y
AlMarzooqi R, Tish S, Tastaldi L et al (2021) Is concomitant cholecystectomy safe during abdominal wall reconstruction? An AHSQC analysis. Hernia 25:295–303. https://doi.org/10.1007/s10029-020-02208-4
Arnold MR, Kao AM, Gbozah KK et al (2018) Optimal management of mesh infection: evidence and treatment options. Int J Abdom wall Hernia Surg 1:42–49
Author information
Authors and Affiliations
Contributions
Study conception and design: CB, EYT. Acquisition of data: CB, YET, JSM, AHM. Analysis and interpretation of data: CB, YET, EMU. Drafting of the manuscript: CB. Critical revision of the manuscript: SHBD, EMU.
Corresponding author
Ethics declarations
Mesh samples were provided by the manufacturer (FEG Textiltechnik, Aachen, Germany) at no cost.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Study registration
Plataforma Brasil (www.plataformabrasil.saude.gov.br/login.jsf), CAAE 52383615.0.0000.0068, Identifier 1.412.367
Clinical Trials, registration ID NCT05061264
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Birolini, C., Tanaka, E.Y., de Miranda, J.S. et al. The early outcomes of complex abdominal wall reconstruction with polyvinylidene (PVDF) mesh in the setting of active infection: a prospective series. Langenbecks Arch Surg 407, 3089–3099 (2022). https://doi.org/10.1007/s00423-022-02625-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02625-2