Abstract
Background
Surgical gastrojejunostomy has traditionally been the palliative treatment of choice for patients with advanced malignancies and gastric outlet obstruction syndrome. Recently, palliative endoscopic duodenal stenting has increased in popularity. We report outcomes after gastrojejunostomy and duodenal stenting when used for palliative indications.
Methods
Consecutive patients undergoing palliative gastrojejunostomy or palliative endoscopic duodenal stenting in a Finnish tertiary referral center between January 2015 and December 2020 were included. The postoperative outcomes of these two palliative interventions were compared. The main outcome measures were mortality and morbidity, rate of reoperations, postoperative oral intake ability, and length of hospital stay.
Results
A total of 88 patients, 46 (52%) patients underwent palliative gastrojejunostomy and 42 (48%) duodenal stenting. All patients had malignant disease, most typically hepatopancreatic cancer. Nineteen (44%) patients in duodenal stenting group and 4 (8.7%) patients in gastrojejunostomy group required subsequent interventions due to persisting or progressing symptoms (p < 0.001). Median delay until first oral intake was 2 days (1–24) after gastrojejunostomy and 0 days (0–3) after stenting (p < 0.001). Postoperative morbidity was 30% after gastrojejunostomy and 45% after stenting (p < 0.001). Median length of hospital stay was 7 days (1–27) after surgery and 5 days (0–20) after endoscopy (p < 0.001).
Conclusions
Patients undergoing endoscopic duodenal stenting are more able to initiate rapid oral intake and have shorter hospital stay. On the other hand, there are significantly more reoperations in stenting group. If the patient’s life expectancy is short, we recommend stenting, but for patients whose life expectancy is longer, gastrojejunostomy could be a better procedure, for the reasons mentioned above.
Similar content being viewed by others
Introduction
Gastric outlet obstruction (GOO) is a constrictive process of the duodenum often associated with advanced gastrointestinal malignancies. [1, 2] Open surgical gastrojejunostomy (GJ) has traditionally been the treatment of choice for patients with advanced malignancies. Although considered a relatively simple procedure, it is associated with significant morbidity and mortality. Less invasive techniques, such as laparoscopic GJ and endoscopic duodenal stenting with self-expanding metal stents (SEMS), have recently increased in popularity. [1,2,3] While earlier studies have reported lower morbidity associated with endoscopy, long-term functional outcomes are reportedly better after surgery [4, 5]. As patients with advanced and incurable cancer are often particularly frail, the advantages of endoscopy have included that endoscopic procedures can be performed in sedation, in contrast to GJ, which requires general anesthesia. [6]
While some earlier studies have been presented, there is only scant data comparing outcomes of different treatment modalities. Consequently, the aim of this study was to compare the short- and long-term outcomes of GJ and stenting in the palliative care of GOO. [1, 4, 7, 8].
Materials and methods
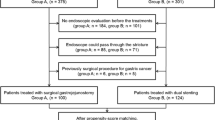
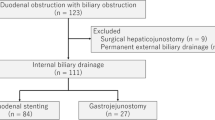
The study is based on retrospective data. Each consecutive patient who underwent palliative GJ or SEMS for malignant GOO in Tampere University Hospital, Finland from January 1, 2015 to December 31, 2020 was included in study. A total of 74 endoscopic duodenal stentings were performed during follow-up, of which 32 were excluded because operation sought curative and in 42 were palliative procedures. At the same time, 70 gastrojejunostomies were performed at Tampere University Hospital, of which 46 were palliative procedures as shown in Fig. 1. Patients’ medical records were reviewed. Only those undergoing the procedure for a palliative indication were included. Patients receiving neoadjuvant therapies after stenting or patients with GOO due to benign causes, such as pancreatitis, were excluded. The type of procedure was selected based on the judgment of an experienced clinician.
Patients were identified by retrieving all cases associated with the Nordic Medico-Statistical Committee classification of surgical procedures (version 1.13) codes. The study population included all patients requiring surgical or endoscopic treatment for malignant GOO in a catchment area of over 500,000 inhabitants as well as some referred patients, when the hospital catchment area exceed one million inhabitants.
Patient data was collected from the Tampere University Hospital surgical database and the medical records. Patient characteristics were recorded, and included age, sex, comorbidities, type of malignancy, preoperative functional ability, preoperative Gastric Outlet Obstruction Scoring System (GOOSS), and indication for the procedure. Main outcomes were postoperative morbidity (according to Clavien-Dindo classification of surgical complications) [9], reoperations, postoperative GOOSS, postoperative oral intake ability, postoperative length of hospital stay, follow-up treatment location, and mortality. GOOSS is one of the most frequently used scoring systems for patients with GOO. GOOSS was originally developed by Adler in 2002. Its ranges 0–3 (0: no oral intake at all, 1: liquids oral intake, 2: soft foods oral intake, 3: normal food oral intake). [10]
Patients underwent either surgery or endoscopic procedures. Both laparoscopic and open surgical techniques were used. GJ was performed by using side-to-side loop anastomosis technique. For endoscopic procedures, the study hospital offered two different self-expanding stent options for duodenal stenting, namely uncovered metal stents (Olympus Hanarostent®) and duodenal stents (Boston scientific Wallflex®). Several size options were available for both stents, which were selected according to the clinician’s assessment.
Statistical analyses were performed using SPSS Statistics version 22 for Windows (IBM Corp, Armonk, NY, USA). Summary measurements were expressed as means with standard deviations or as medians with minimum and maximum values unless otherwise stated. Continuous variables were analyzed using Student’s t-test or Mann–Whitney U-test, the latter for non-normally distributed data. Chi-square or Fisher’s exact test was used for categorical variables. Two-tailed P values were reported and a P value < 0.05 was deemed statistically significant.
The study was conducted according to the requirements of the Helsinki declaration. In compliance with the principles of the local ethics committee, exemption from consent was obtained as the data had already been collected for clinical purposes.
Results
Forty-six patients (24 females, median age 66 years [47–92]) underwent GJ and 42 patients (16 females, median age 72 years [37–95]) SEMS placement. Median follow-up time was 76 days (3–972). Demographic characteristics were practically similar. Most of patients were diagnosed with hepatobiliary (n = 10 in the GJ group and n = 2 in the SEMS group) or pancreatic cancer (n = 16 in the GJ group and n = 25 in SEMS group) (59% in the GJ group and 62% in the SEMS group). Other malignities were in the SEMS group and in the GJ group: gastric (n = 7 and n = 4), duodenal (n = 3 and n = 6), colorectal (n = 1 and n = 3), other (n = 5 and n = 6). The share of patients with locally advanced cancer was 46% in the GJ group and 21% in the SEMS group (p = 0.006) and 52% of GJ group patients and 60% SEMS group patients had distant metastases or peritoneal carcinosis (p = 0.006). Twenty-four percent of the GJ group and 33% of the SEMS group had peritoneal carcinosis (p = 0.328). Table 1 shows the main characteristics of the study population.
Seventy-one percent of SEMS patients received uncovered metal stents and 29% fully covered metal stents. Thirteen of GJ group had undergone stenting attempt, the most typical reason for failure was complete stenosis, i.e., stenting was not technically feasible. The mean interval from the first stenting to the second procedure was 9 days (0–313). A typical reason for the renewed stenting was gastric outlet obstruction. Two patients suffered from stenting associated perforation and required emergency laparotomy and gastrojejunostomy immediately after the operation.
Only one patient required postoperative ICU care. Nineteen patients (45%) in the SEMS group and four (8.7%) in GJ underwent reoperation. In the SEMS group, the most typical reoperation was re-stenting (21%) or gastrojejunostomy (21%). Most typical reason for reoperation was stent obstruction as the disease progressed or problems with gastric emptying even stent was open. Morbidity was 30% in the GJ group and 45% in the SEMS group (p < 0.001). In-hospital mortality was 6.5% in the GJ group and 2.4 in SEMS group (p = 0.113). Short-term hospital readmissions (in 3 months after procedure) were 7 (15%) in GJ group and 17 (41%) in SEMS group (p = 0.003). There was no significant difference in postoperative GOOSS in the study population (p = 0.899). Among GJ patients, the median delay to feeding initiation with liquids was 2 days (1–24) and less than 1 day (0–3) in the SEMS group. Patients in the GJ group received normal food after 6.5 days (1–10) and after 2 days (0–5) in SEMS group. Table 2 show postoperative outcomes.
Times to postoperative oral intake of the patient groups by Kaplan–Meier graphs are presented in Fig. 2. In the SEMS group, oral intake of fluids (p < 0.001), soft foods (p < 0.001), and normal food (p = 0.737) was faster than in the GJ group.
Kaplan–Meier curves illustrating lengths of hospital stay are shown in Fig. 3 and mortality in Fig. 4. Median length of stay in the GJ group was 7 days (1–27) and in the SEMS group 5 days (0–20), p = 0.002. The overall mortality rate during follow-up was 94% in the GJ group and 100% in the SEMS group (p = 0.092). Median survival in the GJ group was 108 days (3–972) and 50 days (9–597) in the SEMS group (p = 0.016).
Discussion
This study compared the two most commonly used methods for palliative relief of malignant GOO. Patients receiving SEMS were able to initiate oral intake more rapidly and had shorter hospital stay than those receiving with GJ but had higher rates of reoperations and mortality.
The goals of palliative care differ from those of curative care. Palliative care aims to prevent and alleviate physical, emotional, and mental suffering among patients dealing with advanced and incurable illness. [11,12,13] Such patients have limited expected life span, and it is easy to understand that rapid recovery, including initiation of oral intake and short hospital stay, are of the utmost importance. Our results were consistent with earlier findings; patients in the SEMS group recovered more rapidly and were able to initiate oral intake faster than those undergoing surgery. Stent insertion is a less invasive procedure, which may explain the faster alleviation of symptoms. [4, 6,7,8, 14] While symptoms were relieved in the majority of patients, a significant portion of our patients required further care at other health care facilities or in residential care. Only a few patients were able to return to their own homes. There was no significant difference between the GJ and SEMS groups in terms of follow-up care. Other important goals of palliative care include low morbidity. Patients are often in poor clinical condition due to multiple days of reduced food intake and weight loss. SEMS group had higher rate of reoperations. Complications were more common after SEMS, but almost every complication that lead to reoperation was related to slowed gastric emptying. Two patients underwent emergency surgery due to stent-associated perforation immediately after stenting and both were treated surgically with gastrojejunostomy. This is comparable to major early complications reported in earlier publications. However, in our study population, there was no bleeding after stenting, which is another typical early major complication. [5, 6, 15] There were no long-term complications associated with stenting, i.e., there were no cases with stent migration or late perforation. While mortality was significant in both patient populations, there were no procedure-associated deaths. Short-term readmissions (max 3 months) were more common among patients with SEMS.
The data were collected in a single high-volume tertiary care center with experienced endoscopists and surgeons performing all procedures. The most significant strength of the present study was the inclusion of all patients undergoing palliative surgery within the second largest hospital district in Finland. The data was comprehensive and included follow-up data on all patients. In our hospital, stents were placed in with the patient under sedation. Patients did not receive general anesthesia unless it was absolutely necessary (e.g., due to fear related to endoscopy or co-operation difficulties). Therefore, we consider patients with more advanced disease and significant co-existing conditions might have undergone stenting instead of possible surgery. This may explain the poorer long-term outcome among SEMS patients, but as noted there were no procedure-related deaths. The relatively short survival among patients with advanced and incurable cancer is not exceptionally dismal. The biggest weakness in this study is the retrospective data, where the clinician’s view of patients is likely to cause selection bias.
Conclusion
The results of our study are similar to those of earlier studies. [1, 7] Patients undergoing endoscopic duodenal stenting are more able to initiate rapid oral intake and have shorter hospital stay. On the other hand, there are significantly more reoperations in stenting group. If the patient’s life expectancy is short, we recommend stenting, but for patients whose life expectancy is longer, gastrojejunostomy could be a better procedure, for the reasons mentioned above. However, further qualitative research on the subject is needed, especially as new and interesting treatment options such as endoscopic ultrasound–guided gastrojejunostomy have been introduced for clinical use. Our study group have plans to conduct an RTC study on this challenging palliative topic in the future.
References
Upchurch E, Ragusa M, Cirocchi R (2018) Stent placement versus surgical palliation for adults with malignant gastric outlet obstruction. Cochrane Database Syst Rev 5:CD012506. https://doi.org/10.1002/14651858.CD012506.pub2
Potz BA, Miner TJ (2016) Surgical palliation of gastric outlet obstruction in advanced malignancy. World J Gastrointest Surg 8(8):545–555. http://lib.cqvip.com/qk/71421X/201608/7000175528.html. https://doi.org/10.4240/wjgs.v8.i8.545. Accessed 21 Dec 2021
Troncone et al (2020) Malignant gastric outlet obstruction: which is the best therapeutic option? World J Gastroenterol 26(16):1847–1860. https://doi.org/10.3748/wjg.v26.i16.1847
Troncone E, Fugazza A, Cappello A et al (2020) Malignant gastric outlet obstruction: which is the best therapeutic option? World journal of gastroenterology:WJG 26(16):1847–1860. https://www.ncbi.nlm.nih.gov/pubmed/32390697. https://doi.org/10.3748/wjg.v26.i16.1847. Accessed 21 Dec 2021
Ratone J, Caillol F, Zemmour C et al (2020) Outcomes of duodenal stenting: experience in a French tertiary center with 220 cases. Dig Liver Dis 52(1):51–56. https://doi.org/10.1016/j.dld.2019.06.025
Uemura S, Iwashita T, Iwata K et al (2018) Endoscopic duodenal stent versus surgical gastrojejunostomy for gastric outlet obstruction in patients with advanced pancreatic cancer. Pancreatol: Off J Int Assoc Pancreatol (IAP) 18(5):601–607. https://doi.org/10.1016/j.pan.2018.04.015
Jang S, Lee H, Min B et al (2017) Palliative gastrojejunostomy versus endoscopic stent placement for gastric outlet obstruction in patients with unresectable gastric cancer: a propensity score-matched analysis. Surg Endosc 31(10):4217–4223. https://www.ncbi.nlm.nih.gov/pubmed/28281127. https://doi.org/10.1007/s00464-017-5480-6. Accessed 19 Dec 2021
Fiori E, MD, Lamazza A, MD, DeMasi E, MD, DeCesare A, Schillaci A, MD, Sterpetti AV, MD (2013) Endoscopic stenting for gastric outlet obstruction in patients with unresectable antro pyloric cancer. Systematic review of the literature and final results of a prospective study. The point of view of a surgical group. Am J Surg 206(2):210–217. https://www.clinicalkey.es/playcontent/1-s2.0-S0002961013001943. https://doi.org/10.1016/j.amjsurg.2012.08.018. Accessed 21 Dec 2021
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Adler DG, Baron TH (2002) Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol 97(1):72–78. https://doi.org/10.1111/j.1572-0241.2002.05423.x
World health organization (2020) World health organization. who.int Web site. https://www.who.int/news-room/fact-sheets/detail/palliative-care. Accessed 16 June 2021
Mosenthal AC, Dunn GP (2019) Surgical palliative care. Oxford University Press, New York, NY
Dunn GP (2015) Surgery, palliative care, and the American College of Surgeons. Ann Palliat Med 4(1):5–9. https://doi.org/10.3978/j.issn.2224-5820.2015.01.03
Jeurnink SM, Steyerberg EW, van Hooft JE et al (2010) Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointestinal endoscopy. 71(3):490–499. https://www.clinicalkey.es/playcontent/1-s2.0-S0016510709025590. https://doi.org/10.1016/j.gie.2009.09.042. Accessed 19 Dec 2021
Keränen I, Kylänpää L, Udd M et al (2013) Gastric outlet obstruction in gastric cancer: a comparison of three palliative methods. J Surg Oncol 108(8):537–541. https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1002/jso.23442
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laitamäki, M., Tyrväinen, T., Lehto, J.T. et al. Endoscopic duodenal stenting is efficient, but has higher rate of reoperations than gastrojejunostomy in palliative treatment for gastric outlet obstruction. Langenbecks Arch Surg 407, 2509–2515 (2022). https://doi.org/10.1007/s00423-022-02565-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02565-x