Abstract
Background
Pancreatic cancer (PC) remains one of the most devastating malignant diseases, predicted to become the second leading cause of cancer-related death by 2030. Despite advances in surgical techniques and in systemic therapy, the 5-year relative survival remains a grim 9% for all stages combined. The extent of lymphadenectomy has been discussed intensively for decades, given that even in early stages of PC, lymph node (LN) metastasis can be detected in approximately 80%.
Purpose
The primary objective of this review was to provide an overview of the current literature evaluating the role of lymphadenectomy in resected PC. For this, we evaluated randomized controlled studies (RCTs) assessing the impact of extent of lymphadenectomy on OS and studies evaluating the prognostic impact of anatomical site of LN metastasis and the impact of the number of resected LNs on OS.
Conclusions
Lymphadenectomy plays an essential part in the multimodal treatment algorithm of PC and is an additional therapeutic tool to increase the chance for surgical radicality and to ensure correct staging for optimal oncological therapy. Based on the literature from the last decades, standard lymphadenectomy with resection of at least ≥ 15 LNs is associated with an acceptable postoperative complication risk and should be recommended to obtain local radicality and accurate staging of the disease. Although radical surgery including appropriate lymphadenectomy of regional LNs remains the only chance for long-term tumor control, future studies specifically assessing the impact of neoadjuvant therapy on extraregional LNs are warranted.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Kleeff J, Korc M, Apte M, La Vecchia C, Johnson CD, Biankin AV, Neale RE, Tempero M, Tuveson DA, Hruban RH, Neoptolemos JP (2016) Pancreatic cancer. Nat Rev Dis Primers 2:16022. https://doi.org/10.1038/nrdp.2016.22
Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, Niedergethmann M, Zulke C, Fahlke J, Arning MB, Sinn M, Hinke A, Riess H (2013) Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA 310(14):1473–1481. https://doi.org/10.1001/jama.2013.279201
Neoptolemos JP, Stocken DD, Bassi C, Ghaneh P, Cunningham D, Goldstein D, Padbury R, Moore MJ, Gallinger S, Mariette C, Wente MN, Izbicki JR, Friess H, Lerch MM, Dervenis C, Olah A, Butturini G, Doi R, Lind PA, Smith D, Valle JW, Palmer DH, Buckels JA, Thompson J, McKay CJ, Rawcliffe CL, Buchler MW, European Study Group for Pancreatic C (2010) Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA 304(10):1073–1081. https://doi.org/10.1001/jama.2010.1275
Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, Kaneoka Y, Shimizu Y, Nakamori S, Sakamoto H, Morinaga S, Kainuma O, Imai K, Sata N, Hishinuma S, Ojima H, Yamaguchi R, Hirano S, Sudo T, Ohashi Y, Group JS (2016) Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 388(10041):248–257. https://doi.org/10.1016/S0140-6736(16)30583-9
Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, Faluyi O, O'Reilly DA, Cunningham D, Wadsley J, Darby S, Meyer T, Gillmore R, Anthoney A, Lind P, Glimelius B, Falk S, Izbicki JR, Middleton GW, Cummins S, Ross PJ, Wasan H, McDonald A, Crosby T, Ma YT, Patel K, Sherriff D, Soomal R, Borg D, Sothi S, Hammel P, Hackert T, Jackson R, Buchler MW, European Study Group for Pancreatic C (2017) Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet 389(10073):1011–1024. https://doi.org/10.1016/S0140-6736(16)32409-6
Sinn M, Bahra M, Liersch T, Gellert K, Messmann H, Bechstein W, Waldschmidt D, Jacobasch L, Wilhelm M, Rau BM, Grutzmann R, Weinmann A, Maschmeyer G, Pelzer U, Stieler JM, Striefler JK, Ghadimi M, Bischoff S, Dorken B, Oettle H, Riess H (2017) CONKO-005: Adjuvant chemotherapy with gemcitabine plus erlotinib versus gemcitabine alone in patients after R0 resection of pancreatic cancer: a multicenter randomized phase III trial. J Clin Oncol 35(29):3330–3337. https://doi.org/10.1200/JCO.2017.72.6463
Altman AM, Wirth K, Marmor S, Lou E, Chang K, Hui JYC, Tuttle TM, Jensen EH, Denbo JW (2019) Completion of adjuvant chemotherapy after upfront surgical resection for pancreatic cancer is uncommon yet associated with improved survival. Ann Surg Oncol 26(12):4108–4116. https://doi.org/10.1245/s10434-019-07602-6
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardiere C, Bennouna J, Bachet JB, Khemissa-Akouz F, Pere-Verge D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M, Groupe Tumeurs Digestives of U, Intergroup P (2011) FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364(19):1817–1825. https://doi.org/10.1056/NEJMoa1011923
Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul JL, Chone L, Francois E, Artru P, Biagi JJ, Lecomte T, Assenat E, Faroux R, Ychou M, Volet J, Sauvanet A, Breysacher G, Di Fiore F, Cripps C, Kavan P, Texereau P, Bouhier-Leporrier K, Khemissa-Akouz F, Legoux JL, Juzyna B, Gourgou S, O'Callaghan CJ, Jouffroy-Zeller C, Rat P, Malka D, Castan F, Bachet JB, Canadian Cancer Trials G, the Unicancer GIPG (2018) FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med 379(25):2395–2406. https://doi.org/10.1056/NEJMoa1809775
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369(18):1691–1703. https://doi.org/10.1056/NEJMoa1304369
Isaji S, Mizuno S, Windsor JA, Bassi C, Fernandez-Del Castillo C, Hackert T, Hayasaki A, Katz MHG, Kim SW, Kishiwada M, Kitagawa H, Michalski CW, Wolfgang CL (2018) International consensus on definition and criteria of borderline resectable pancreatic ductal adenocarcinoma 2017. Pancreatology 18(1):2–11. https://doi.org/10.1016/j.pan.2017.11.011
Zhan HX, Xu JW, Wu D, Wu ZY, Wang L, Hu SY, Zhang GY (2017) Neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of prospective studies. Cancer Med 6(6):1201–1219. https://doi.org/10.1002/cam4.1071
Hackert T, Sachsenmaier M, Hinz U, Schneider L, Michalski CW, Springfeld C, Strobel O, Jager D, Ulrich A, Buchler MW (2016) Locally advanced pancreatic cancer: neoadjuvant therapy with FOLFIRINOX results in resectability in 60% of the patients. Ann Surg 264(3):457–463. https://doi.org/10.1097/SLA.0000000000001850
Niesen W, Hank T, Buchler M, Strobel O (2019) Local radicality and survival outcome of pancreatic cancer surgery. Ann Gastroenterol Surg 3(5):464–475. https://doi.org/10.1002/ags3.12273
Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA (2012) ‘Artery-first’ approaches to pancreatoduodenectomy. Br J Surg 99(8):1027–1035. https://doi.org/10.1002/bjs.8763
Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, Schirmacher P, Buchler MW (2008) Most pancreatic cancer resections are R1 resections. Ann Surg Oncol 15(6):1651–1660. https://doi.org/10.1245/s10434-008-9839-8
Nakao A, Harada A, Nonami T, Kaneko T, Murakami H, Inoue S, Takeuchi Y, Takagi H (1995) Lymph node metastases in carcinoma of the head of the pancreas region. Br J Surg 82(3):399–402. https://doi.org/10.1002/bjs.1800820340
Hirono S, Kawai M, Okada KI, Miyazawa M, Shimizu A, Kitahata Y, Ueno M, Shimokawa T, Nakao A, Yamaue H (2017) Mesenteric approach during pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. Ann Gastroenterol Surg 1(3):208–218. https://doi.org/10.1002/ags3.12013
Schneider M, Strobel O, Hackert T, Buchler MW (2019) Pancreatic resection for cancer-the Heidelberg technique. Langenbecks Arch Surg 404(8):1017–1022. https://doi.org/10.1007/s00423-019-01839-1
Hackert T, Strobel O, Michalski CW, Mihaljevic AL, Mehrabi A, Muller-Stich B, Berchtold C, Ulrich A, Buchler MW (2017) The TRIANGLE operation - radical surgery after neoadjuvant treatment for advanced pancreatic cancer: a single arm observational study. HPB (Oxford) 19(11):1001–1007. https://doi.org/10.1016/j.hpb.2017.07.007
Strobel O, Hinz U, Gluth A, Hank T, Hackert T, Bergmann F, Werner J, Buchler MW (2015) Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg 261(5):961–969. https://doi.org/10.1097/SLA.0000000000000814
Sergeant G, Melloul E, Lesurtel M, Deoliveira ML, Clavien PA (2013) Extended lymphadenectomy in patients with pancreatic cancer is debatable. World J Surg 37(8):1782–1788. https://doi.org/10.1007/s00268-013-2064-z
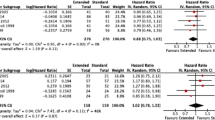
Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C, Kloppel G, Dhaene K, Michelassi F (1998) Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg 228(4):508–517. https://doi.org/10.1097/00000658-199810000-00007
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, Hodgin MB, Sauter PK, Hruban RH, Riall TS, Schulick RD, Choti MA, Lillemoe KD, Yeo CJ (2006) 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10(9):1199–1210; discussion 1210-1191. https://doi.org/10.1016/j.gassur.2006.08.018
Showalter TN, Winter KA, Berger AC, Regine WF, Abrams RA, Safran H, Hoffman JP, Benson AB, MacDonald JS, Willett CG (2011) The influence of total nodes examined, number of positive nodes, and lymph node ratio on survival after surgical resection and adjuvant chemoradiation for pancreatic cancer: a secondary analysis of RTOG 9704. Int J Radiat Oncol Biol Phys 81(5):1328–1335. https://doi.org/10.1016/j.ijrobp.2010.07.1993
Morales-Oyarvide V, Rubinson DA, Dunne RF, Kozak MM, Bui JL, Yuan C, Qian ZR, Babic A, Da Silva A, Nowak JA, Khalaf N, Brais LK, Welch MW, Zellers CL, Ng K, Chang DT, Miksad RA, Bullock AJ, Tseng JF, Swanson RS, Clancy TE, Linehan DC, Findeis-Hosey JJ, Doyle LA, Hornick JL, Ogino S, Fuchs CS, Hezel AF, Koong AC, Wolpin BM (2017) Lymph node metastases in resected pancreatic ductal adenocarcinoma: predictors of disease recurrence and survival. Br J Cancer 117(12):1874–1882. https://doi.org/10.1038/bjc.2017.349
Groot VP, Rezaee N, Wu W, Cameron JL, Fishman EK, Hruban RH, Weiss MJ, Zheng L, Wolfgang CL, He J (2018) Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg 267(5):936–945. https://doi.org/10.1097/SLA.0000000000002234
Manabe T, Ohshio G, Baba N, Miyashita T, Asano N, Tamura K, Yamaki K, Nonaka A, Tobe T (1989) Radical pancreatectomy for ductal cell carcinoma of the head of the pancreas. Cancer 64(5):1132–1137. https://doi.org/10.1002/1097-0142(19890901)64:5<1132::aid-cncr2820640528>3.0.co;2-v
Ishikawa O, Ohhigashi H, Sasaki Y, Kabuto T, Fukuda I, Furukawa H, Imaoka S, Iwanaga T (1988) Practical usefulness of lymphatic and connective tissue clearance for the carcinoma of the pancreas head. Ann Surg 208(2):215–220. https://doi.org/10.1097/00000658-198808000-00014
Warschkow R, Tsai C, Kohn N, Erdem S, Schmied B, Nussbaum DP, Gloor B, Muller SA, Blazer D 3rd, Worni M (2020) Role of lymphadenectomy, adjuvant chemotherapy, and treatment at high-volume centers in patients with resected pancreatic cancer-a distinct view on lymph node yield. Langenbecks Arch Surg 405(1):43–54. https://doi.org/10.1007/s00423-020-01859-2
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, Coleman J, Abrams RA, Hruban RH (2002) Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg 236(3):355–366; discussion 366-358. https://doi.org/10.1097/00000658-200209000-00012
Farnell MB, Pearson RK, Sarr MG, DiMagno EP, Burgart LJ, Dahl TR, Foster N, Sargent DJ, Pancreas Cancer Working G (2005) A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery 138(4):618–628; discussion 628-630. https://doi.org/10.1016/j.surg.2005.06.044
Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, Andren-Sandberg A, Asbun HJ, Bockhorn M, Buchler MW, Conlon KC, Fernandez-Cruz L, Fingerhut A, Friess H, Hartwig W, Izbicki JR, Lillemoe KD, Milicevic MN, Neoptolemos JP, Shrikhande SV, Vollmer CM, Yeo CJ, Charnley RM, International Study Group on Pancreatic S (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156(3):591–600. https://doi.org/10.1016/j.surg.2014.06.016
Pedrazzoli S, Beger HG, Obertop H, Andren-Sandberg A, Fernandez-Cruz L, Henne-Bruns D, Luttges J, Neoptolemos JP (1999) A surgical and pathological based classification of resective treatment of pancreatic cancer. Summary of an international workshop on surgical procedures in pancreatic cancer. Dig Surg 16(4):337–345. https://doi.org/10.1159/000018744
Isaji SMY, Kishiwada M (2018) New Japanese classification of pancreatic cancer Pancreatic cancer 7 ed Springer: p. 1021–1037
Society JP (2003) Classification of pancreatic carcinoma (2nd English ed.). Kanehara & Co Ltd, Tokyo
Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goere D, Seufferlein T, Haustermans K, Van Laethem JL, Conroy T, Arnold D, Committee EG (2015) Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):v56–v68. https://doi.org/10.1093/annonc/mdv295
Nappo G, Perinel J, El Bechwaty M, Adham M (2016) The standardization of pancreatoduodenectomy: where are we? Pancreas 45(4):493–502. https://doi.org/10.1097/MPA.0000000000000503
Japan Pancreas Society KC, Ltd. Classification of pancreatic carcinoma. 2nd English ed. Tokyo
Hirata K, Sato T, Mukaiya M, Yamashiro K, Kimura M, Sasaki K, Denno R (1997) Results of 1001 pancreatic resections for invasive ductal adenocarcinoma of the pancreas. Arch Surg 132(7):771–776; discussion 777. https://doi.org/10.1001/archsurg.1997.01430310085018
Nimura Y, Nagino M, Takao S, Takada T, Miyazaki K, Kawarada Y, Miyagawa S, Yamaguchi A, Ishiyama S, Takeda Y, Sakoda K, Kinoshita T, Yasui K, Shimada H, Katoh H (2012) Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci 19(3):230–241. https://doi.org/10.1007/s00534-011-0466-6
Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Yu HC, Kang KJ, Kim SG, Kim SW (2014) A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg 259(4):656–664. https://doi.org/10.1097/SLA.0000000000000384
Jang JY, Kang JS, Han Y, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Park JS, Yu HC, Kang KJ, Kim SG, Lee H, Kwon W, Yoon YS, Han HS, Kim SW (2017) Long-term outcomes and recurrence patterns of standard versus extended pancreatectomy for pancreatic head cancer: a multicenter prospective randomized controlled study. J Hepatobiliary Pancreat Sci 24(7):426–433. https://doi.org/10.1002/jhbp.465
Ignjatovic I, Knezevic S, Knezevic D, Dugalic V, Micev M, Matic S, Ostojic S, Bogdanovic M, Pavlovic I, Jurisic V (2017) Standard versus extended lymphadenectomy in radical surgical treatment for pancreatic head carcinoma. J BUON 22(1):232–238
Nagakawa T, Kobayashi H, Ueno K, Ohta T, Kayahara M, Miyazaki I (1994) Clinical study of lymphatic flow to the paraaortic lymph nodes in carcinoma of the head of the pancreas. Cancer 73(4):1155–1162. https://doi.org/10.1002/1097-0142(19940215)73:4<1155::aid-cncr2820730406>3.0.co;2-h
Yoshida T, Matsumoto T, Sasaki A, Shibata K, Aramaki M, Kitano S (2004) Outcome of paraaortic node-positive pancreatic head and bile duct adenocarcinoma. Am J Surg 187(6):736–740. https://doi.org/10.1016/j.amjsurg.2003.07.031
Kanda M, Fujii T, Nagai S, Kodera Y, Kanzaki A, Sahin TT, Hayashi M, Yamada S, Sugimoto H, Nomoto S, Takeda S, Morita S, Nakao A (2011) Pattern of lymph node metastasis spread in pancreatic cancer. Pancreas 40(6):951–955. https://doi.org/10.1097/MPA.0b013e3182148342
Murakami Y, Uemura K, Sudo T, Hayashidani Y, Hashimoto Y, Nakashima A, Yuasa Y, Kondo N, Ohge H, Sueda T (2010) Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg 211(2):196–204. https://doi.org/10.1016/j.jamcollsurg.2010.03.037
Liu C, Lu Y, Luo G, Cheng H, Guo M, Liu Z, Xu J, Long J, Liu L, Fu D, Ni Q, Li M, Yu X (2016) Which patients with para-aortic lymph node (LN16) metastasis will truly benefit from curative pancreaticoduodenectomy for pancreatic head cancer? Oncotarget 7(20):29177–29186. https://doi.org/10.18632/oncotarget.8690
Kayahara M, Nagakawa T, Ueno K, Ohta T, Tsukioka Y, Miyazaki I (1995) Surgical strategy for carcinoma of the pancreas head area based on clinicopathologic analysis of nodal involvement and plexus invasion. Surgery 117(6):616–623. https://doi.org/10.1016/s0039-6060(95)80003-4
Yeo CJ, Cameron JL, Sohn TA, Coleman J, Sauter PK, Hruban RH, Pitt HA, Lillemoe KD (1999) Pancreaticoduodenectomy with or without extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma: comparison of morbidity and mortality and short-term outcome. Ann Surg 229(5):613–622; discussion 622-614. https://doi.org/10.1097/00000658-199905000-00003
Schwarz L, Lupinacci RM, Svrcek M, Lesurtel M, Bubenheim M, Vuarnesson H, Balladur P, Paye F (2014) Para-aortic lymph node sampling in pancreatic head adenocarcinoma. Br J Surg 101(5):530–538. https://doi.org/10.1002/bjs.9444
Shimada K, Sakamoto Y, Sano T, Kosuge T (2006) The role of paraaortic lymph node involvement on early recurrence and survival after macroscopic curative resection with extended lymphadenectomy for pancreatic carcinoma. J Am Coll Surg 203(3):345–352. https://doi.org/10.1016/j.jamcollsurg.2006.05.289
Chun YS, Pawlik TM, Vauthey JN (2018) 8th Edition of the AJCC cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol 25(4):845–847. https://doi.org/10.1245/s10434-017-6025-x
Shrikhande SV, Kleeff J, Reiser C, Weitz J, Hinz U, Esposito I, Schmidt J, Friess H, Buchler MW (2007) Pancreatic resection for M1 pancreatic ductal adenocarcinoma. Ann Surg Oncol 14(1):118–127. https://doi.org/10.1245/s10434-006-9131-8
Hackert T, Niesen W, Hinz U, Tjaden C, Strobel O, Ulrich A, Michalski CW, Buchler MW (2017) Radical surgery of oligometastatic pancreatic cancer. Eur J Surg Oncol 43(2):358–363. https://doi.org/10.1016/j.ejso.2016.10.023
Sperti C, Gruppo M, Blandamura S, Valmasoni M, Pozza G, Passuello N, Beltrame V, Moletta L (2017) Para-aortic node involvement is not an independent predictor of survival after resection for pancreatic cancer. World J Gastroenterol 23(24):4399–4406. https://doi.org/10.3748/wjg.v23.i24.4399
van Rijssen LB, Narwade P, van Huijgevoort NC, Tseng DS, van Santvoort HC, Molenaar IQ, van Laarhoven HW, van Eijck CH, Busch OR, Besselink MG, Dutch Pancreatic Cancer G (2016) Prognostic value of lymph node metastases detected during surgical exploration for pancreatic or periampullary cancer: a systematic review and meta-analysis. HPB (Oxford) 18(7):559–566. https://doi.org/10.1016/j.hpb.2016.05.001
Agalianos C, Gouvas N, Papaparaskeva K, Dervenis C (2016) Positive para-aortic lymph nodes following pancreatectomy for pancreatic cancer. Systematic review and meta-analysis of impact on short term survival and association with clinicopathologic features. HPB (Oxford) 18(8):633–641. https://doi.org/10.1016/j.hpb.2016.04.007
Sho M, Murakami Y, Motoi F, Satoi S, Matsumoto I, Kawai M, Honda G, Uemura K, Yanagimoto H, Kurata M, Fukumoto T, Akahori T, Kinoshita S, Nagai M, Nishiwada S, Unno M, Yamaue H, Nakajima Y (2015) Postoperative prognosis of pancreatic cancer with para-aortic lymph node metastasis: a multicenter study on 822 patients. J Gastroenterol 50(6):694–702. https://doi.org/10.1007/s00535-014-1005-4
Ashfaq A, Pockaj BA, Gray RJ, Halfdanarson TR, Wasif N (2014) Nodal counts and lymph node ratio impact survival after distal pancreatectomy for pancreatic adenocarcinoma. J Gastrointest Surg 18(11):1929–1935. https://doi.org/10.1007/s11605-014-2566-5
Malleo G, Maggino L, Ferrone CR, Marchegiani G, Mino-Kenudson M, Capelli P, Rusev B, Lillemoe KD, Bassi C, Fernandez-Del Castillo C, Salvia R (2019) Number of examined lymph nodes and nodal status assessment in distal pancreatectomy for body/tail ductal adenocarcinoma. Ann Surg 270(6):1138–1146. https://doi.org/10.1097/SLA.0000000000002781
Elshaer M, Gravante G, Kosmin M, Riaz A, Al-Bahrani A (2017) A systematic review of the prognostic value of lymph node ratio, number of positive nodes and total nodes examined in pancreatic ductal adenocarcinoma. Ann R Coll Surg Engl 99(2):101–106. https://doi.org/10.1308/rcsann.2016.0340
Schwarz RE, Smith DD (2006) Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol 13(9):1189–1200. https://doi.org/10.1245/s10434-006-9016-x
Warschkow R, Widmann B, Beutner U, Marti L, Steffen T, Schiesser M, Schmied BM (2017) The more the better-lower rate of stage migration and better survival in patients with retrieval of 20 or more regional lymph nodes in pancreatic cancer: a population-based propensity score matched and trend SEER analysis. Pancreas 46(5):648–657. https://doi.org/10.1097/MPA.0000000000000784
Vuarnesson H, Lupinacci RM, Semoun O, Svrcek M, Julie C, Balladur P, Penna C, Bachet JB, Resche-Rigon M, Paye F (2013) Number of examined lymph nodes and nodal status assessment in pancreaticoduodenectomy for pancreatic adenocarcinoma. Eur J Surg Oncol 39(10):1116–1121. https://doi.org/10.1016/j.ejso.2013.07.089
Valsangkar NP, Bush DM, Michaelson JS, Ferrone CR, Wargo JA, Lillemoe KD, Fernandez-del Castillo C, Warshaw AL, Thayer SP (2013) N0/N1, PNL, or LNR? The effect of lymph node number on accurate survival prediction in pancreatic ductal adenocarcinoma. J Gastrointest Surg 17(2):257–266. https://doi.org/10.1007/s11605-012-1974-7
Riediger H, Kulemann B, Wittel U, Adam U, Sick O, Neeff H, Hoppner J, Hopt UT, Makowiec F (2016) Prognostic role of log odds of lymph nodes after resection of pancreatic head cancer. J Gastrointest Surg 20(10):1707–1715. https://doi.org/10.1007/s11605-016-3200-5
La Torre M, Cavallini M, Ramacciato G, Cosenza G, Rossi Del Monte S, Nigri G, Ferri M, Mercantini P, Ziparo V (2011) Role of the lymph node ratio in pancreatic ductal adenocarcinoma. Impact on patient stratification and prognosis. J Surg Oncol 104(6):629–633. https://doi.org/10.1002/jso.22013
Mirkin KA, Hollenbeak CS, Wong J (2017) Greater lymph node retrieval and lymph node ratio impacts survival in resected pancreatic cancer. J Surg Res 220:12–24. https://doi.org/10.1016/j.jss.2017.06.076
Tol JA, Brosens LA, van Dieren S, van Gulik TM, Busch OR, Besselink MG, Gouma DJ (2015) Impact of lymph node ratio on survival in patients with pancreatic and periampullary cancer. Br J Surg 102(3):237–245. https://doi.org/10.1002/bjs.9709
Nakao A, Harada A, Nonami T, Kaneko T, Nomoto S, Koyama H, Kanazumi N, Nakashima N, Takagi H (1997) Lymph node metastasis in carcinoma of the body and tail of the pancreas. Br J Surg 84(8):1090–1092. https://doi.org/10.1046/j.1365-2168.1997.02754.x
Kayahara M, Nagakawa T, Futagami F, Kitagawa H, Ohta T, Miyazaki I (1996) Lymphatic flow and neural plexus invasion associated with carcinoma of the body and tail of the pancreas. Cancer 78(12):2485–2491. https://doi.org/10.1002/(sici)1097-0142(19961215)78:12<2485::aid-cncr6>3.0.co;2-j
Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A, Bassi C, Butturini G, Salvia R (2015) Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the standard international study group of pancreatic surgery definition of lymphadenectomy for cancer. J Am Coll Surg 221(2):367–379 e364. https://doi.org/10.1016/j.jamcollsurg.2015.02.019
Zhou Y, Lin J, Wang W, Chen H, Deng X, Peng C, Cheng D, Shen B (2019) Should a standard lymphadenectomy include the No. 9 lymph nodes for body and tail pancreatic ductal adenocarcinoma? Pancreatology 19(3):414–418. https://doi.org/10.1016/j.pan.2019.03.005
Huebner M, Kendrick M, Reid-Lombardo KM, Que F, Therneau T, Qin R, Donohue J, Nagorney D, Farnell M, Sarr M (2012) Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg 16(5):920–926. https://doi.org/10.1007/s11605-012-1853-2
Zheng ZJ, Wang MJ, Tan CL, Chen YH, Ping J, Liu XB (2020) Prognostic impact of lymph node status in patients after total pancreatectomy for pancreatic ductal adenocarcinoma: a strobe-compliant study. Medicine (Baltimore) 99(8):e19327. https://doi.org/10.1097/MD.0000000000019327
Lau MK, Davila JA, Shaib YH (2010) Incidence and survival of pancreatic head and body and tail cancers: a population-based study in the United States. Pancreas 39(4):458–462. https://doi.org/10.1097/MPA.0b013e3181bd6489
Ruess DA, Makowiec F, Chikhladze S, Sick O, Riediger H, Hopt UT, Wittel UA (2015) The prognostic influence of intrapancreatic tumor location on survival after resection of pancreatic ductal adenocarcinoma. BMC Surg 15:123. https://doi.org/10.1186/s12893-015-0110-5
Moon HJ, An JY, Heo JS, Choi SH, Joh JW, Kim YI (2006) Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Pancreas 32(1):37–43. https://doi.org/10.1097/01.mpa.0000194609.24606.4b
Parikh PY, Lillemoe KD (2015) Surgical management of pancreatic cancer--distal pancreatectomy. Semin Oncol 42(1):110–122. https://doi.org/10.1053/j.seminoncol.2014.12.010
Strasberg SM, Drebin JA, Linehan D (2003) Radical antegrade modular pancreatosplenectomy. Surgery 133(5):521–527. https://doi.org/10.1067/msy.2003.146
Chang YR, Han SS, Park SJ, Lee SD, Yoo TS, Kim YK, Kim TH, Woo SM, Lee WJ, Hong EK (2012) Surgical outcome of pancreatic cancer using radical antegrade modular pancreatosplenectomy procedure. World J Gastroenterol 18(39):5595–5600. https://doi.org/10.3748/wjg.v18.i39.5595
Park HJ, You DD, Choi DW, Heo JS, Choi SH (2014) Role of radical antegrade modular pancreatosplenectomy for adenocarcinoma of the body and tail of the pancreas. World J Surg 38(1):186–193. https://doi.org/10.1007/s00268-013-2254-8
Collard M, Marchese T, Guedj N, Cauchy F, Chassaing C, Ronot M, Dokmak S, Soubrane O, Sauvanet A (2019) Is routine splenectomy justified for all left-sided pancreatic cancers? Histological reappraisal of splenic hilar lymphadenectomy. Ann Surg Oncol 26(4):1071–1078. https://doi.org/10.1245/s10434-018-07123-8
Onesti JK, Chung MH, Jain DH, Stafford MM, Attawala PP (2013) A review of splenic pathology in distal pancreatectomies. Pancreatology 13(6):625–628. https://doi.org/10.1016/j.pan.2013.10.006
Navez J, Marique L, Hubert C, Van Laethem JL, Komuta M, Maris C, D'Haene N, Navez B, Closset J (2020) Distal pancreatectomy for pancreatic neoplasia: is splenectomy really necessary? A bicentric retrospective analysis of surgical specimens. HPB (Oxford). doi:https://doi.org/10.1016/j.hpb.2020.01.016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors or any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Erdem, S., Bolli, M., Müller, S.A. et al. Role of lymphadenectomy in resectable pancreatic cancer. Langenbecks Arch Surg 405, 889–902 (2020). https://doi.org/10.1007/s00423-020-01980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01980-2