Abstract
Purpose
Anastomotic leakage after resection of gastroesophageal junction cancer is a dangerous complication, and leakage rates have remained stable for decades. Perfusion is crucial for anastomotic healing, but traditional perfusion assessment is limited in a minimally invasive environment. New methods as indocyanine green fluorescence angiography (ICG-FA) have proven promising, but quantitative analysis has been challenging. This study aimed to demonstrate the feasibility and usability of real-time intraoperative quantitative fluorescence angiography (q-ICG) with a touchscreen tablet.
Methods
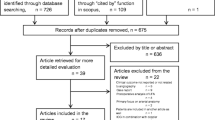
A software for q-ICG was previously developed and validated. Ten patients underwent perfusion assessment in white light (WL), with ICG-FA, and with q-ICG during Ivor-Lewis esophageal resection. The usability of the tablet-based software was tested with the System Usability Scale (SUS®). Furthermore, we investigated the differences in perfusion assessment as the distance from the conduit margin to a surgeon selected point of sufficient perfusion for anastomosis using the different modalities.
Results
Q-ICG was successful in all patients, with an excellent median SUS® of 82.5 (77.5–93.8). Significant differences in distances from the conduit margin to points of sufficient perfusion selected by the surgeons were found: ICG: WL = 14.1 mm (p = 0.048), q-ICG: WL = 32.08 mm (p < 0.001), and q-ICG: ICG = 17.95 mm (p = 0.002). Furthermore, significant differences of perfusion were found between the points, when q-ICG was performed retrospectively in the surgeon selected areas (p = 0.008–0.013).
Conclusion
Real-time intraoperative touchscreen-based q-ICG was feasible with excellent usability, and differences in sufficient perfusion points selected by the surgeons between modalities were found. Further studies should focus on clinical relevance and determine cutoff values associated with anastomotic leakage.



Similar content being viewed by others
References
Bollschweiler E, Wolfgarten E, Gutschow C, Holscher AH (2001) Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer 92:549–555
Hashimoto T, Kurokawa Y, Mori M, Doki Y (2018) Surgical treatment of gastroesophageal junction cancer. J Gastric Cancer 18:209–217. https://doi.org/10.5230/jgc.2018.18.e28
Markar S, Gronnier C, Duhamel A et al (2015) The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg 262:972–980. https://doi.org/10.1097/SLA.0000000000001011
Ohi M, Toiyama Y, Mohri Y, Saigusa S, Ichikawa T, Shimura T, Yasuda H, Okita Y, Yoshiyama S, Kobayashi M, Araki T, Inoue Y, Kusunoki M (2017) Prevalence of anastomotic leak and the impact of indocyanine green fluorescein imaging for evaluating blood flow in the gastric conduit following esophageal cancer surgery. Esophagus 14:351–359. https://doi.org/10.1007/s10388-017-0585-5
Irino T, Persson S, Lundell L et al (2018) Pulse oximetric assessment of anatomical vascular contribution to tissue perfusion in the gastric conduit. ANZ J Surg. https://doi.org/10.1111/ans.14399
Ishige F, Nabeya Y, Hoshino I, Takayama W, Chiba S, Arimitsu H, Iwatate Y, Yanagibashi H (2019) Quantitative assessment of the blood perfusion of the gastric conduit by indocyanine green imaging. J Surg Res 234:303–310. https://doi.org/10.1016/j.jss.2018.08.056
Karampinis I, Ronellenfitsch U, Mertens C et al (2017) Indocyanine green tissue angiography affects anastomotic leakage after esophagectomy. A retrospective, case-control study. Int J Surg 48:210–214. https://doi.org/10.1016/j.ijsu.2017.11.001
Kitagawa H, Namikawa T, Iwabu J, Fujisawa K, Uemura S, Tsuda S, Hanazaki K (2018) Assessment of the blood supply using the indocyanine green fluorescence method and postoperative endoscopic evaluation of anastomosis of the gastric tube during esophagectomy. Surg Endosc 32:1749–1754. https://doi.org/10.1007/s00464-017-5857-6
Nishikawa K, Fujita T, Yuda M et al (2018) Quantitative assessment of blood flow in the gastric conduit with thermal imaging for esophageal reconstruction. Ann Surg. https://doi.org/10.1097/SLA.0000000000003169
Zehetner J, DeMeester SR, Alicuben ET et al (2015) Intraoperative assessment of perfusion of the gastric graft and correlation with anastomotic leaks after esophagectomy. Ann Surg 262:74–78. https://doi.org/10.1097/SLA.0000000000000811
Ambrus R, Svendsen LB, Secher NH, Rünitz K, Frederiksen HJ, Svendsen MB, Siemsen M, Kofoed SC, Achiam MP (2017) A reduced gastric corpus microvascular blood flow during Ivor-Lewis esophagectomy detected by laser speckle contrast imaging technique. Scand J Gastroenterol 52:455–461. https://doi.org/10.1080/00365521.2016.1265664
Jansen SM, de Bruin DM, van Berge Henegouwen MI et al (2018) Optical techniques for perfusion monitoring of the gastric tube after esophagectomy: a review of technologies and thresholds. Dis Esophagus. https://doi.org/10.1093/dote/dox161
Kumagai Y, Hatano S, Sobajima J et al (2018) Indocyanine green fluorescence angiography of the reconstructed gastric tube during esophagectomy: efficacy of the 90-second rule. Dis Esophagus 31. https://doi.org/10.1093/dote/doy052
Degett TH, Andersen HS, Gogenur I (2016) Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: a systematic review of clinical trials. Langenbeck's Arch Surg 401:767–775. https://doi.org/10.1007/s00423-016-1400-9
Nerup N, Andersen HS, Ambrus R, Strandby RB, Svendsen MBS, Madsen MH, Svendsen LB, Achiam MP (2017) Quantification of fluorescence angiography in a porcine model. Langenbeck's Arch Surg 402:655–662. https://doi.org/10.1007/s00423-016-1531-z
Nerup N, Knudsen KBK, Ambrus R, Svendsen MBS, Thymann T, Ifaoui IBR, Svendsen LB, Achiam MP (2017) Reproducibility and reliability of repeated quantitative fluorescence angiography. Surg Technol Int 31:35–39
Nerup N, Ring LL, Strandby RB, Egeland C, Svendsen MBS, Hasselby JP, Willemoe GL, Hartmann B, Svendsen LB, Achiam MP (2018) Quantitative perfusion assessment of intestinal anastomoses in pigs treated with glucagon-like peptide 2. Langenbeck's Arch Surg 403:881–889. https://doi.org/10.1007/s00423-018-1718-6
Ronn JH, Nerup N, Strandby RB et al (2019) Laser speckle contrast imaging and quantitative fluorescence angiography for perfusion assessment. Langenbeck's Arch Surg 404:505–515. https://doi.org/10.1007/s00423-019-01789-8
Rolff HC, Ambrus RB, Belmouhand M et al (2017) Robot-assisted hybrid esophagectomy is associated with a shorter length of stay compared to conventional transthoracic esophagectomy: a retrospective study. Minim Invasive Surg 2017:6907896. https://doi.org/10.1155/2017/6907896
Brooke J (1996) SUS - a quick and dirty usability scale. Usability Eval Ind 189:4–7
Bangor A, Kortum PT, Miller JT (2008) An empirical evaluation of the system usability scale. Int J Hum Comput Interact 24:574–594. https://doi.org/10.1080/10447310802205776
Liljequist D, Elfving B, Skavberg Roaldsen K (2019) Intraclass correlation - a discussion and demonstration of basic features. PLoS One 14:e0219854. https://doi.org/10.1371/journal.pone.0219854
Paolucci I, Schwalbe M, Prevost GA, Lachenmayer A, Candinas D, Weber S, Tinguely P (2018) Design and implementation of an electromagnetic ultrasound-based navigation technique for laparoscopic ablation of liver tumors. Surg Endosc 32:3410–3419. https://doi.org/10.1007/s00464-018-6088-1
Barresi G, Deshpande N, Mattos LS et al (2013) Comparative usability and performance evaluation of surgeon interfaces in laser phonomicrosurgery. In: 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems. p 3610–3615
Ikeda Y, Niimi M, Kan S et al (2001) Clinical significance of tissue blood flow during esophagectomy by laser Doppler flowmetry. J Thorac Cardiovasc Surg 122:1101–1106. https://doi.org/10.1067/mtc.2001.117835
Acknowledgments
The authors sincerely thank all participating surgeons, anesthesiologists, nurses, and patients for their valuable effort. The study was sponsored by donations from private foundations, and we are deeply grateful to the Rigshospitalet Research Foundation, King Christian the X Foundation, and Aage and Johanne Louis-Hansen Foundation for their support. Sponsors had no role in study design, interpretation of results, or any other part of the study.
Author information
Authors and Affiliations
Contributions
Study conception and design: NN, MBSS, LBS, and MA. Acquisition of data: NN. Analysis and interpretation of data: NN, MBSS, LBS, and MA. Drafting of manuscript: NN. Critical revision of manuscript: NN, MBSS, LBS, and MA.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Danish Committee on Health Research Ethics (ID: H-18006334) and registered at clinicaltrials.gov (ID: NCT03671642) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nerup, N., Svendsen, M.B.S., Svendsen, L.B. et al. Feasibility and usability of real-time intraoperative quantitative fluorescent-guided perfusion assessment during resection of gastroesophageal junction cancer. Langenbecks Arch Surg 405, 215–222 (2020). https://doi.org/10.1007/s00423-020-01876-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01876-1