Abstract
Background
The Da Vinci Robotic Surgical System has positioned itself as a tool that improves the ergonomics of the surgeon, facilitating dissection in confined spaces and enhancing the surgeon’s skills. The technical aspects for successful bile duct repair are well-vascularized ducts, tension-free anastomosis, and complete drainage of hepatic segments, and all are achievable with robotic-assisted approach.
Methods
This was a retrospective study of our prospectively collected database of patients with iatrogenic bile duct injury who underwent robotic-assisted Roux-en-Y hepaticojejunostomy. Pre-, intra-, and short-term postoperative data were analyzed.
Results
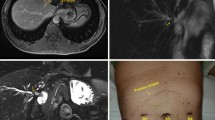
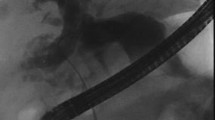
A total of 30 consecutive patients were included. The median age was 46.5 years and 76.7% were female. Neo-confluences with section of hepatic segment IV were performed in 7 patients (those classified as Strasberg E4). In the remaining 23, a Hepp-Couinaud anastomosis was built. There were no intraoperative complications, the median estimated blood loss was 100 mL, and the median operative time was 245 min. No conversion was needed. The median length of stay was 6 days and the median length of follow-up was 8 months. The overall morbidity rate was 23.3%. Two patients presented hepaticojejunostomy leak. No mortality was registered.
Conclusion
Robotic surgery is feasible and can be safely performed, with acceptable short-term results, in bile duct injury repair providing the advantages of minimally invasive surgery. Further studies with larger number of cases and longer follow-up are needed to establish the role of robotic assisted approaches in the reconstruction of BDI.




Similar content being viewed by others
References
De Santibañes E, Palavecino M, Ardiles V, Pekolj J (2006) Bile duct injuries: management of late complications. Surg Endosc 20(11):1648–1653. https://doi.org/10.1007/s00464-006-0491-8
Mercado MA, Franssen B, Domínguez I, Arriola-Cabrera JC, Ramírez-del Val F, Elnecavé-Olaiz A, Arámburo-Garcia R, García A (2011) Transition from a low-to a high-volume center bile duct repair: changes in technique and improved outcome. HPB (Oxford) 13(11):767–773. https://doi.org/10.1111/j.1477-2574.2011.00356.x
Chapa-Azuela O, Ortiz-Higareda V, Etchegaray-Dondé A, Cruz-Martínez R, Hernández-Mejía BI (2013) Tratamiento quirúrgico de las lesiones iatrogénicas de la vía biliar. Rev Med Hosp Gen Mex 76(1):7–14
Liu Y, Yao X, Li S, Liu W, Liu L, Liu J (2014) Comparison of therapeutic effects of laparoscopic and open operation for con- genital choledochal cysts in adults. Gastroenterol Res Pract 2014:670260
Ng JL, Salim MT, Low Y (2014) Mid-term outcomes of laparoscopic versus open choledochal cyst excision in a tertiary paediatric hospital. Ann Acad Med Singap 43(4):220–224
Aguirre-Olmedo I, Cuendis-Velázquez A, Morales-Chávez CE, Torres-Ruiz MF, Rojano-Rodríguez ME, Cárdenas-Lailson LE (2013) Laparoscopic choledochoduodenostomy as an optional treatment choledocholithiasis. Cir Cir 81(2):118–124
Chander J, Mangla V, Vindal A, Lal P, Ramteke VK (2012) Laparoscopic choledochoduodenostomy for biliary stone disease: a single-center 10-year experience. J Laparoendosc Adv Surg Tech A 22(1):81–84. https://doi.org/10.1089/lap.2011.0366
Kondratiuk OP, Khil’ko IO, Kondratiuk VA, Kravchenko DA (2014) Laparoscopic hepaticojejunostomy in patients with inoperable tumour of pancreatic head. Klin Khir 4:64–65
Cuendis-Velázquez A, Morales-Chávez C, Aguirre-Olmedo I, Torres-Ruiz F, Rojano-Rodríguez M, Fernández-Álvarez L, Cárdenas-Lailson E, Moreno-Portillo M (2016) Laparoscopic hepaticojejunostomy after bile duct injury. Surg Endosc 30(3):876–882. https://doi.org/10.1007/s00464-015-4282-y
Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60(1):39–45. https://doi.org/10.1016/S0090-4295(02)01717-X
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–125
Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM (2009) “Sideways”: result of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg 249(3):426–434. https://doi.org/10.1097/SLA.0b013e31819a6b2e
Hepp J, Couinaud C (1956) Approach to and use of the left hepatic duct in reparation of the common bile duct. Presse Med 64(41):947–948
Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA (2003) Acute bile duct injury. The need for a high repair. Surg Endosc 17(9):1351–1355. https://doi.org/10.1007/s00464-002-8705-1
Mercado MA, Orozco H, de la Garza L, Lopez-Martinez LM, Contreras A, Guillen-Navarro E (1999) Biliary duct injury: partial segment IV resection for intrahepatic reconstruction of biliary lesions. Arch Surg 134(9):1008–1010. https://doi.org/10.1001/archsurg.134.9.1008
Strasberg SM, Picus DD, Drebin JA (2001) Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg 5(3):266–274. https://doi.org/10.1016/S1091-255X(01)80047-0
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Macedo FI, Casillas VJ, Davis JS, Levi JU, Sleeman D (2013) Biliary-colonic fistula caused by cholecystectomy bile duct injury. Hepatobiliary Pancreat Dis Int 12(4):443–445. https://doi.org/10.1016/S1499-3872(13)60070-3
Prasad A, De S, Mishra P, Tiwari A (2015) Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. World J Gastroenterol 21(6):1703–1706. https://doi.org/10.3748/wjg.v21.i6.1703
Giulianotti PC, Quadri P, Durgam S, Bianco FM (2017) Reconstruction/repair of iatrogenic biliary injuries, is the robot offering a new option? Short clinical report. Ann Surg 267(1):e7–e9. https://doi.org/10.1097/SLA.0000000000002343
Schwenk W, Hasse O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 20(3):CD003145
Zhang Y, Chen XM, Sun DL (2014) Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World J Surg Oncol 12(1):327. https://doi.org/10.1186/1477-7819-12-327
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2014) Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. World J Gastroenterol 20(46):17626–17634. https://doi.org/10.3748/wjg.v20.i46.17626
Bablekos GD, Michaelides SA, Analitis A, Charalabopoulos KA (2014) Effects of laparoscopic cholecystectomy on lung function: a systematic review. World J Gastroenterol 20(46):17603–17617. https://doi.org/10.3748/wjg.v20.i46.17603
Gonzalez-Ciccarelli LF, Quadri P, Daskalaki D, Milone L, Gangemi A, Giulianotti PC (2016) Robotic approach to hepatobiliary surgery. Chirurg 88(Suppl 1):19–28
Ismael HN, Cox S, Cooper A, Narula N, Aloia T (2017) The morbidity and mortality of hepaticojejunostomies for complex bile duct injuries: a multi-institutional analysis of risk factors and outcomes using NSQIP. HPB (Oxford) 19(4):352–358. https://doi.org/10.1016/j.hpb.2016.12.004
Iannelli A, Paineau J, Hamy A, Schneck AS, Schaaf C, Gugenheim J (2013) Primary versus delayed repair for bile duct injuries sustained during cholecystectomy: results of a survey of the association Francaise de Chirurgie. HPB (Oxford) 15(8):611–616. https://doi.org/10.1111/hpb.12024
Boerma A, Rauws EA, Keulemans YC, Bergman JJ, Obertop H, Huibregtse K, Gouma DJ (2001) Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg 234(6):750–757. https://doi.org/10.1097/00000658-200112000-00006
Walsh RM, Henderson JM, Vogt DP, Brown N (2007) Long-term outcome of biliary reconstruction for bile duct injuries from laparoscopic cholecystectomies. Surgery 142(4):450–456. https://doi.org/10.1016/j.surg.2007.07.008
Savader SJ, Lillemoe KD, Prescott CA, Winick AB, Venbrux AC, Lund GB, Mitchell SE, Cameron JL, Osterman FA Jr (1997) Laparoscopic cholecystectomy-related bile duct injuries: a health and financial disaster. Ann Surg 225(3):268–273. https://doi.org/10.1097/00000658-199703000-00005
Dageforde LA, Landman MP, Feurer ID, Poulose B, Pinson CW, Moore DE (2012) A cost-effectiveness analysis of early vs late reconstruction of iatrogenic bile duct injuries. J Am Coll Surg 214(6):919–927. https://doi.org/10.1016/j.jamcollsurg.2012.01.054
Wormer BA, Dacey KT, Williams KB, Bradley JF 3rd, Walters AL, Augenstein VA, Stefanidis D, Heniford BT (2014) The first nationwide evaluation of robotic general surgery: a regionalized, small but safe start. Surg Endosc 28(3):767–776. https://doi.org/10.1007/s00464-013-3239-2
Acknowledgments
We thank Dr. Florencio de la Concha Bermejillo, who helped in the edition of this paper, as well as all the referring surgeons who trusted our team for the treatment of their patients.
Author information
Authors and Affiliations
Contributions
Drs. Adolfo Cuendis-Velázquez, Orlando Bada-Yllán, Mario Trejo-Ávila, Enrique Rosales-Castañeda, Andrés Rodríguez-Parra, Alberto Moreno-Ordaz, Eduardo Cárdenas-Lailson, Martin Rojano-Rodríguez, Carlos Sanjuan-Martínez, and Mucio Moreno-Portillo contributed equally in study conception and design, acquisition of data, analysis and interpretation of data drafting of manuscript, and critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Cuendis-Velázquez, A., Bada-Yllán, O., Trejo-Ávila, M. et al. Robotic-assisted Roux-en-Y hepaticojejunostomy after bile duct injury. Langenbecks Arch Surg 403, 53–59 (2018). https://doi.org/10.1007/s00423-018-1651-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1651-8