Abstract
Purposes
Unfortunately, surgical site infections (SSIs) are a quite common complication and represent one of the major causes of postoperative morbidity and mortality, and may furthermore lead to enormous additional costs for hospitals and health care systems.
Methods
In order to determine the estimated costs due to SSIs, a MEDLINE search was performed to identify articles that provide data on economic aspects of SSIs and compared to findings from a matched case-control study on costs of SSIs after coronary bypass grafting (CABG) in a German tertiary care university hospital.
Results
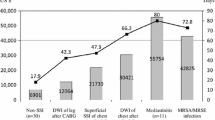
A total of 14 studies on costs were found. The additional costs of SSI vary between $3,859 (mean) and $40,559 (median). Median costs of a single CABG case in the recently published study were $49,449 (€36,261) vs. $18,218 (€13,356) in controls lacking infection (p < 0.0001). The median reimbursement from health care insurance companies was $36,962 (€27,107) leading to a financial loss of $12,482 (€9,154) each.
Conclusion
Costs of SSIs may almost triple the individual overall health care costs and those additional charges may not be sufficiently covered. Appropriate measures to reduce SSI rates must be taken to improve the patient’s safety. This should also diminish costs for health care systems which benefits the entire community.
Similar content being viewed by others
References
Gastmeier P et al (2005) Reduction of orthopaedic wound infections in 21 hospitals. Arch Orthop Trauma Surg 125:526–530
Gaynes RP et al (2001) Surgical site infection (SSI) rates in the United States, 1992–1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis 33(Suppl 2):S69–S77
Biscione FM (2009) Rates of surgical site infection as a performance measure: are we ready? World J Gastrointest Surg 1:11–15
Hollenbeak CS et al (2000) The clinical and economic impact of deep chest surgical site infections following coronary artery bypass graft surgery. Chest 118:397–402
Coskun D, Aytac J, Aydinli A, Bayer A (2005) Mortality rate, length of stay and extra cost of sternal surgical site infections following coronary artery bypass grafting in a private medical centre in Turkey. J Hosp Infect 60:176–179
Romaniszyn D et al (2006) Epidemiological and microbiological surveillance of surgical site infections in orthopedic unit. Ortop Traumatol Rehabil 8:639–645
Graf K et al (2010) Economic aspects of deep sternal wound infections. Eur J Cardiothorac Surg 37:893–896
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
McGarry SA, Engemann JJ, Schmader K, Sexton DJ, Kaye KS (2004) Surgical-site infection due to Staphylococcus aureus among elderly patients: mortality, duration of hospitalization, and cost. Infect Control Hosp Epidemiol 25:461–467
Herwaldt LA et al (2006) A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol 27:1291–1298
Anderson DJ et al (2007) Underresourced hospital infection control and prevention programs: penny wise, pound foolish? Infect Control Hosp Epidemiol 28:767–773
Sparling KW et al (2007) Financial impact of failing to prevent surgical site infections. Qual Manag Health Care 16:219–225
Olsen MA et al (2008) Hospital-associated costs due to surgical site infection after breast surgery. Arch Surg 143:53–60
Coello R et al (2005) Adverse impact of surgical site infections in English hospitals. J Hosp Infect 60:93–103
Monge JV, de Los Terreros SL Sainz, Diaz-Agero PC, Saa Requejo CM, Plana FN (2006) Excess length of stay attributable to surgical site infection following hip replacement: a nested case-control study. Infect Control Hosp Epidemiol 27:1299–1303
Pollard TC, Newman JE, Barlow NJ, Price JD, Willett KM (2006) Deep wound infection after proximal femoral fracture: consequences and costs. J Hosp Infect 63:133–139
Alfonso JL et al (2007) Are we really seeing the total costs of surgical site infections? A Spanish study. Wound Repair Regen 15:474–481
Penel N et al (2008) Additional direct medical costs associated with nosocomial infections after head and neck cancer surgery: a hospital-perspective analysis. Int J Oral Maxillofac Surg 37:135–139
Mokhtari A et al (2008) The cost of vacuum-assisted closure therapy in treatment of deep sternal wound infection. Scand Cardiovasc J 42:85–89
Weber WP et al (2008) Economic burden of surgical site infections at a European university hospital. Infect Control Hosp Epidemiol 29:623–629
Coskun D, Aytac J (2006) The decrease in healthcare-associated methicillin-resistant Staphylococcus aureus infections and savings from glycopeptide use. Infect Control Hosp Epidemiol 27:1131–1132
Hollenbeak CS, Alfrey EJ, Sheridan K, Burger TL, Dillon PW (2003) Surgical site infections following pediatric liver transplantation: risks and costs. Transpl Infect Dis 5:72–78
Upton A, Smith P, Roberts S (2005) Excess cost associated with Staphylococcus aureus poststernotomy mediastinitis. N Z Med J 118:1210, U1316
Lopez Gude MJ et al (2006) Case-control study of risk factors for mediastinitis after cardiovascular surgery. Infect Control Hosp Epidemiol 27:1397–1400
Lucet JC (2006) Surgical site infection after cardiac surgery: a simplified surveillance method. Infect Control Hosp Epidemiol 27:1393–1396
Braxton JH et al (2000) Mediastinitis and long-term survival after coronary artery bypass graft surgery. Ann Thorac Surg 70:2004–2007
Braxton JH et al (2004) 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg 16:70–76
Ridderstolpe L, Gill H, Granfeldt H, Ahlfeldt H, Rutberg H (2001) Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg 20:1168–1175
Ridderstolpe L, Gill H, Borga M, Rutberg H, Ahlfeldt H (2005) Canonical correlation analysis of risk factors and clinical outcomes in cardiac surgery. J Med Syst 29:357–377
Boyce JM, Potter-Bynoe G, Dziobek L (1990) Hospital reimbursement patterns among patients with surgical wound infections following open heart surgery. Infect Control Hosp Epidemiol 11:89–93
Tammelin A, Domicel P, Hambraeus A, Stahle E (2000) Dispersal of methicillin-resistant Staphylococcus epidermidis by staff in an operating suite for thoracic and cardiovascular surgery: relation to skin carriage and clothing. J Hosp Infect 44:119–126
Tammelin A, Hambraeus A, Stahle E (2001) Source and route of methicillin-resistant Staphylococcus epidermidis transmitted to the surgical wound during cardio-thoracic surgery. Possibility of preventing wound contamination by use of special scrub suits. J Hosp Infect 47:266–276
Barwolff S et al (2006) Reduction of surgical site infections after Caesarean delivery using surveillance. J Hosp Infect 64:156–161
Brandt C et al (2006) Reduction of surgical site infection rates associated with active surveillance. Infect Control Hosp Epidemiol 27:1347–1351
Bode LG et al (2010) Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 362:9–17
Munoz P et al (2008) Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J Hosp Infect 68:25–31
Halablab MA, Hijazi SM, Fawzi MA, Araj GF (2010) Staphylococcus aureus nasal carriage rate and associated risk factors in individuals in the community. Epidemiol Infect 138:702–706
Berthelot P et al (2010) Is nasal carriage of Staphylococcus aureus the main acquisition pathway for surgical-site infection in orthopaedic surgery? Eur J Clin Microbiol Infect Dis 29:373–382
Young LS, Winston LG (2006) Preoperative use of mupirocin for the prevention of healthcare-associated Staphylococcus aureus infections: a cost-effectiveness analysis. Infect Control Hosp Epidemiol 27:1304–1312
Bratzler DW, Houck PM (2004) Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis 38:1706–1715
Gagliotti C, Ravaglia F, Resi D, Moro ML (2004) Quality of local guidelines for surgical antimicrobial prophylaxis. J Hosp Infect 56:67–70
Niel-Weise BS, Wille JC, van den Broek PJ (2005) Hair removal policies in clean surgery: systematic review of randomized, controlled trials. Infect Control Hosp Epidemiol 26:923–928
Dizer B et al (2009) The effect of nurse-performed preoperative skin preparation on postoperative surgical site infections in abdominal surgery. J Clin Nurs 18:3325–3332
Segers P, de Jong AP, Spanjaard L, Ubbink DT, de Mol BA (2007) Randomized clinical trial comparing two options for postoperative incisional care to prevent poststernotomy surgical site infections. Wound Repair Regen 15:192–196
Bassi C et al (2010) Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg 252:207–214
Le TA et al (2007) Reduction in surgical site infections in neurosurgical patients associated with a bedside hand hygiene program in Vietnam. Infect Control Hosp Epidemiol 28:583–588
Anderson DJ et al (2008) Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol 29(Suppl 1):S51–S61
Robert Koch Institute (2007) Prevention of postoperative surgical wound infection: recommendations of the Hospital Hygiene and Infection Prevention Committee of the Robert Koch Institute. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50:377–393
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 20:250–278
Graf K et al (2009) Decrease of deep sternal surgical site infection rates after cardiac surgery by a comprehensive infection control program. Interact Cardiovasc Thorac Surg 9:282–286
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Graf, K., Ott, E., Vonberg, RP. et al. Surgical site infections—economic consequences for the health care system. Langenbecks Arch Surg 396, 453–459 (2011). https://doi.org/10.1007/s00423-011-0772-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0772-0