Abstract
Purpose
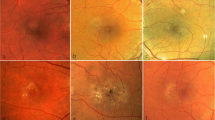
We aimed to examine the possible effects of the postmenopausal period on retinal and choroidal microvascular circulation using swept-source optical coherence tomography angiography (SS-OCTA).
Methods
This cross-sectional study included 45 eyes of 45 subjects in menstrual group and 40 eyes of 40 subjects in postmenopausal group. SS-OCTA was used for the assessment of vessel density (VD), foveal avascular zone (FAZ), choroidal thickness (CT), choriocapillaris VD, central macular thickness (CMT), nerve fiber layer thickness (RNFL), and ganglion cell layer (GCL) measurements.
Result
The VDs of the superficial capillary plexus (SCP) and deep capillary plexus (DCP) measurements were similar in both group. FAZ area was wider in postmenopausal group (0.305 mm2 (range, 0.212–0.498 mm2)) compared to menstrual group (0.271 mm2 (range, 0.131–0.464 mm2)) (p = 0.013). Choriocapillaris VD was significantly lower in postmenopausal group (p = 0.049). CT was thicker in the postmenopausal group, but with no statistically significant difference (p = 0.066). Central macular thickness, RNFL, and GCL were similar in both groups.
Conclusion
This is the first study in the literature to evaluate the retinochoroidal microcirculation in the menstrual and postmenopausal periods with SS-OCTA. We observed an increase in both superficial and deep FAZ area and a decrease in choroidal blood flow in the postmenopausal period. We think that this enlargement in the FAZ area may be related to the decreased amount of estrogen.


Similar content being viewed by others
Data availability
All data and materials are available from the supplementary material.
References
Allshouse A, Pavlovic J, Santoro N (2018) Menstrual cycle hormone changes associated with reproductive aging and how they may relate to symptoms. ObstetGynecolClin North Am 45:613–628. https://doi.org/10.1016/j.ogc.2018.07.004
Harlow SD, Gass M, Hall JE et al (2012) Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J ClinEndocrinolMetab 97:1159–1168. https://doi.org/10.1210/jc.2011-3362
De-Hita-Cantalejo C, Sánchez-González MC, Silva-Viguera C et al (2022) Efficacy of hyaluronic acid 0.3%, cyanocobalamin, electrolytes, and P-Plus in menopause patients with moderate dry eye disease. Graefes Arch ClinExpOphthalmol 260:529–535. https://doi.org/10.1007/s00417-021-05415-6
The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society (2020) Menopause. 27:976–92. https://doi.org/10.1097/GME.0000000000001609
Zhao D, Guallar E, Ouyang P et al (2018) Endogenous sex hormones and incident cardiovascular disease in post-menopausal women. J Am CollCardiol 71:2555–2566. https://doi.org/10.1016/j.jacc.2018.01.083
Welten SJGC, Onland-Moret NC, Boer JMA et al (2021) Age at menopause and risk of ischemic and hemorrhagic stroke. Stroke 52:2583–2591. https://doi.org/10.1161/STROKEAHA.120.030558
Jiang J, Cui J, Wang A et al (2019) Association between age at natural menopause and risk of type 2 diabetes in postmenopausal women with and without obesity. J ClinEndocrinolMetab 104:3039–3048. https://doi.org/10.1210/jc.2018-02310
Lu CB, Liu PF, Zhou YS et al (2020) Musculoskeletal pain during the menopausal transition: a systematic review and meta-analysis. Neural Plast 2020:8842110. https://doi.org/10.1155/2020/8842110
Younan C, Mitchell P, Cumming RG et al (2002) Hormone replacement therapy, reproductive factors, and the incidence of cataract and cataract surgery: the Blue Mountains Eye Study. Am J Epidemiol 155:997–1006. https://doi.org/10.1093/aje/155.11.997
Beebe DC, Holekamp NM, Shui YB (2010) Oxidative damage and the prevention of age-related cataracts. Ophthalmic Res 44:155–165. https://doi.org/10.1159/000316481
RudnickaAR JZ, Wormald R et al (2012) Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: a meta-analysis. Ophthalmol 119:571–580. https://doi.org/10.1016/j.ophtha.2011.09.027
Snow KK, Cote J, Yang W et al (2002) Association between reproductive and hormonal factors and age-related maculopathy in post-menopausal women. Am J Ophthalmol 134:842–848. https://doi.org/10.1016/S0002-9394(02)01755-5
Douglass A, Dattilo M, Feola AJ (2022) Evidence for menopause as a sex-specific risk factor for glaucoma. Cell MolNeurobiol. https://doi.org/10.1007/s10571-021-01179-z
Kaarniranta K, Machalinska A, Vereb Z et al (2015) Estrogen signalling in the pathogenesis of age-related macular degeneration. Curr Eye Res 40:226–233. https://doi.org/10.3109/02713683.2014.925933
Zhou L, Wang F, Wang L et al (2021) Quantitative assessment and determinants of foveal avascular zone in healthy volunteers. J Int Med Res 49:3000605211014994. https://doi.org/10.1177/03000605211014994
Agemy SA, Scripsema NK, Shah CM et al (2015) Retinal vascular perfusion density mapping using optical coherence tomography angiography in normals and diabetic retinopathy patients. Retina 35:2353–2363. https://doi.org/10.1097/IAE.0000000000000862
Chun LY, Silas MR, Dimitroyannis RC et al (2019) Differences in macular capillary parameters between healthy black and white subjects with Optical Coherence Tomography Angiography (OCTA). PLoS ONE 14:e0223142. https://doi.org/10.1371/journal.pone.0223142
Wang Q, Chan S, Yang JY et al (2016) Vascular density in retina and choriocapillaris as measured by optical coherence tomography angiography. Am J Ophthalmol 168:95–109. https://doi.org/10.1016/j.ajo.2016.05.005
Morales D, Wu A, Wu L (2021) The foveal avascular zone area in healthy eyes measured by ocular coherence tomography angiography using a full spectrum probabilistic algorithm. IntOphthalmol 41:2187–2196. https://doi.org/10.1007/s10792-021-01776-3
Tan CS, Lim LW, Chow VS et al (2016) Optical coherence tomography angiography evaluation of the parafoveal vasculature and its relationship with ocular factors. Invest Ophthalmol Vis Sci. 57:224–34. https://doi.org/10.1167/iovs.15-18869
Gómez-Ulla F, Cutrin P, Santos P et al (2019) Age and gender influence on foveal avascular zone in healthy eyes. Exp Eye Res 189:107856. https://doi.org/10.1016/j.exer.2019.107856
Nuzzi R, Scalabrin S, Becco A et al (2018) Gonadal hormones and retinal disorders: a review. Front Endocrinol (Lausanne) 9:66. https://doi.org/10.3389/fendo.2018.00066
Gupta PD, Johar K, Nagpal K et al (2005) Sex hormone receptors in the human eye. SurvOphthalmol 50:274–284. https://doi.org/10.1016/j.survophthal.2005.02.005
Ogueta SB, Schwartz SD, Yamashita CK et al (1999) Estrogen receptor in the human eye: influence of gender and age on gene expression. Invest Ophthalmol Vis Sci 40:1906–1911
Ding X, Li J, Zeng J et al (2011) Choroidal thickness in healthy Chinese subjects. Invest Ophthalmol Vis Sci 52:9555–9560. https://doi.org/10.1167/iovs.11-8076
Ataş M, Açmaz G, Aksoy H et al (2014) Evaluation of the macula, retinal nerve fiber layer and choroidthickness in postmenopausal women and reproductive-age women using spectral-domain optical coherence tomography. Prz Menopauzalny 13:36–41. https://doi.org/10.5114/pm.2014.41088
Wei WB, Xu L, Jonas JB et al (2013) Subfoveal choroidal thickness: the Beijing Eye Study. Ophthalmol 120:175–180. https://doi.org/10.1016/j.ophtha.2012.07.048
Margolis R, Spaide RF (2009) A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol 147:811–815. https://doi.org/10.1016/j.ajo.2008.12.008
Centofanti M, Bonini S, Manni G et al (2000) Do sex and hormonal status influence choroidal circulation? Br J Ophthalmol 84(7):786–787. https://doi.org/10.1136/bjo.84.7.786
Kavroulaki D, Gugleta K, Kochkorov A et al (2010) Influence of gender and menopausal status on peripheral and choroidal circulation. Acta Ophthalmol 88:850–853. https://doi.org/10.1111/j.1755-3768.2009.01607.x
Toker E, Yenice O, Akpinar I et al (2003) The influence of sex hormones on ocular blood flow in women. Acta Ophthalmol Scand 81:617–624. https://doi.org/10.1111/j.1395-3907.2003.00160.x
Altintaş O, Caglar Y, Yüksel N et al (2004) The effects of menopause and hormone replacement therapy on quality and quantity of tear, intraocular pressure and ocular blood flow. Ophthalmologica 218:120–129. https://doi.org/10.1159/000076148
Sullivan DA, Hammitt KM, Schaumberg DA et al (2012) Report of the TFOS/ARVO Symposium on global treatments for dry eye disease: an unmet need. Ocul Surf 10:108–116
Suzuki T, Minami Y, Komuro A et al (2017) Meibomian gland physiology in pre- and postmenopausal women. Invest Ophthalmol Vis Sci 58:763–771. https://doi.org/10.1167/iovs.16-20811
Affinito P, Di SpiezioSardo A, Di Carlo C et al (2003) Effects of hormone replacement therapy on ocular function inpostmenopause. Menopause 10:482–487. https://doi.org/10.1097/01.GME.0000063568.84134.35
Smith W, Mitchell P, Wang JJ (1997) Gender, oestrogen, hormone replacement and age-related macular degeneration: results from the Blue Mountains Eye Study. Aust N Z J Ophthalmol 25:13–15. https://doi.org/10.1111/j.1442-9071.1997.tb01745.x
Funding
The authors received no funding for the research, authorship, and/or publication of this article from any government or private institution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the Akdeniz University Faculty of Medicine (Approval Number: KAEK-973). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent to participate and publish
Informed consent for publication of their clinical details and/or clinical images was obtained from all individual participants included in the study. A copy of the consent form is available for review by the editor of this journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çetinkaya Yaprak, A., Erkan Pota, Ç. Comparison of retinochoroidal microvascular circulation in menstrual and postmenopausal periods using swept-source optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol 261, 367–373 (2023). https://doi.org/10.1007/s00417-022-05807-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05807-2