Abstract
Purpose
Uveitis accounts for 10–15% of all cases of blindness in the developed world. Uveitic macular edema (UME) is a primary cause of permanent visual impairment in patients with uveitis. Because proinflammatory mediators elicit inflammation and lead to UME, we determined the profiles of proinflammatory mediators associated with complications, such as ME, in the vitreous humor of patients with panuveitis related to Behçet’s disease (BD) and sarcoidosis.
Methods
In this retrospective study, we enrolled 21 patients with uveitis, including 6 with BD and 15 with sarcoidosis, and 15 patients with idiopathic epiretinal membrane (iERM) at the Department of Ophthalmology, Kyushu University Hospital, between January 2008 and April 2016. Vitreous concentrations of 32 proinflammatory mediators, including cytokines and soluble receptors of tumor necrosis factor (TNF) and interleukin (IL)-6 families, were assessed using a bead-based multiplex assay and their association with clinical data was examined.
Results
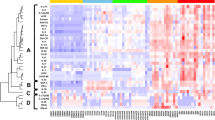
The levels of proinflammatory mediators, including a proliferation-inducing ligand (APRIL), B cell activating factor belonging to the TNF family (BAFF), soluble cluster of differentiation 30 (sCD30), soluble TNF receptor-1 (sTNFR1), sTNFR2, TNF-α, IL-6, and soluble IL-6 receptor-α (sIL-6Rα), were significantly higher in patients with uveitis. With regard to clinical parameters in patients with uveitis, vitreous levels of BAFF and sIL-6Rα were prominently elevated in patients with UME compared to in those without UME (P < 0.01, respectively).
Conclusions
Our results suggest that elevated vitreous levels of BAFF and sIL-6Rα are associated with the pathogenesis of UME in patients with panuveitis related to BD and sarcoidosis.


Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available from the corresponding author, A.T., upon reasonable request.
References
Massa H, Pipis SY, Adewoyin T, Vergados A, Patra S, Panos GD (2019) Macular edema associated with non-infectious uveitis: pathophysiology, etiology, prevalence, impact and management challenges. Clin Ophthalmol 13:1761–1777. https://doi.org/10.2147/OPTH.S180580
Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, Murray PI (2004) Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol 88:1159–1162. https://doi.org/10.1136/bjo.2003.037226
Dick AD, Tundia N, Sorg R, Zhao C, Chao J, Joshi A, Skup M (2016) Risk of ocular complications in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology 123:655–662. https://doi.org/10.1016/j.ophtha.2015.10.028
Koronis S, Stavrakas P, Balidis M, Kozeis N, Tranos PG (2019) Update in treatment of uveitic macular edema. Drug Des Dev Ther 13:667–680. https://doi.org/10.2147/DDDT.S166092
Accorinti M, Okada AA, Smith JR, Gilardi M (2019) Epidemiology of macular edema in uveitis. Ocul Immunol Inflamm 27:169–180. https://doi.org/10.1080/09273948.2019.1576910
Lardenoye CW, van Kooij B, Rothova A (2006) Impact of macular edema on visual acuity in uveitis. Ophthalmology 113:1446–1449. https://doi.org/10.1016/j.ophtha.2006.03.027
Munk MR, Kiss CG, Steiner I, Sulzbacher F, Roberts P, Kroh M, Montuoro A, Simader C, Schmidt-Erfurth U (2013) Systematic correlation of morphologic alterations and retinal function in eyes with uveitis-associated cystoid macular oedema during development, resolution and relapse. Br J Ophthalmol 97:1289–1296. https://doi.org/10.1136/bjophthalmol-2012-303052
Li YH, Hsu SL, Sheu SJ (2021) A review of local therapy for the management of cystoid macular edema in uveitis. Asia Pac J Ophthalmol (Phila) 10:87–92. https://doi.org/10.1097/APO.0000000000000352
Writing Committee for the Multicenter Uveitis Steroid Treatment T, Follow-up Study Research G, Kempen JH, Altaweel MM, Holbrook JT, Sugar EA, Thorne JE, Jabs DA (2017) Association between long-lasting intravitreous fluocinolone acetonide implant vs systemic anti-inflammatory therapy and visual acuity at 7 years among patients with intermediate, posterior, or panuveitis. JAMA 317:1993–2005. https://doi.org/10.1001/jama.2017.5103
Levin MH, Pistilli M, Daniel E, Gangaputra SS, Nussenblatt RB, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, Jabs DA, Levy-Clarke GA, Kempen JH, Systemic Immunosuppressive Therapy for Eye Diseases Cohort S (2014) Incidence of visual improvement in uveitis cases with visual impairment caused by macular edema. Ophthalmology 121(588–595):e581. https://doi.org/10.1016/j.ophtha.2013.09.023
Takeda A, Yanai R, Murakami Y, Arima M, Sonoda KH (2020) New insights into immunological therapy for retinal disorders. Front Immunol 11:1431. https://doi.org/10.3389/fimmu.2020.01431
Hassan M, Karkhur S, Bae JH, Halim MS, Ormaechea MS, Onghanseng N, Nguyen NV, Afridi R, Sepah YJ, Do DV, Nguyen QD (2019) New therapies in development for the management of non-infectious uveitis: a review. Clin Exp Ophthalmol 47:396–417. https://doi.org/10.1111/ceo.13511
Valentincic NV, de Groot-Mijnes JD, Kraut A, Korosec P, Hawlina M, Rothova A (2011) Intraocular and serum cytokine profiles in patients with intermediate uveitis. Mol Vis 17:2003–2010
van Kooij B, Rothova A, Rijkers GT, de Groot-Mijnes JD (2006) Distinct cytokine and chemokine profiles in the aqueous of patients with uveitis and cystoid macular edema. Am J Ophthalmol 142:192–194. https://doi.org/10.1016/j.ajo.2006.02.052
Vegas-Revenga N, Calvo-Rio V, Mesquida M, Adan A, Hernandez MV, Beltran E, Valls Pascual E, Diaz-Valle D, Diaz-Cordoves G, Hernandez-Garfella M, Martinez-Costa L, Calvo I, Atanes A, Linares LF, Modesto C, Gonzalez-Vela C, Demetrio-Pablo R, Aurrecoechea E, Cordero M, Dominguez-Casas LC, Atienza-Mateo B, Martin-Varillas JL, Loricera J, Palmou-Fontana N, Hernandez JL, Gonzalez-Gay MA, Blanco R (2019) Anti-IL6-receptor tocilizumab in refractory and noninfectious uveitic cystoid macular edema: multicenter study of 25 patients. Am J Ophthalmol 200:85–94. https://doi.org/10.1016/j.ajo.2018.12.019
Mesquida M, Drawnel F, Lait PJ, Copland DA, Stimpson ML, Llorenc V, Sainz de la Maza M, Adan A, Widmer G, Strassburger P, Fauser S, Dick AD, Lee RWJ, Molins B (2019) Modelling macular edema: the effect of IL-6 and IL-6R blockade on human blood-retinal barrier integrity in vitro. Transl Vis Sci Technol 8:32. https://doi.org/10.1167/tvst.8.5.32
Zahir-Jouzdani F, Atyabi F, Mojtabavi N (2017) Interleukin-6 participation in pathology of ocular diseases. Pathophysiology 24:123–131. https://doi.org/10.1016/j.pathophys.2017.05.005
Kunimi K, Usui Y, Asakage M, Maehara C, Tsubota K, Mitsuhashi R, Umazume A, Kezuka T, Sakai JI, Goto H (2020) Anti-TNF-alpha therapy for refractory uveitis associated with Behcet’s syndrome and sarcoidosis: a single center study of 131 patients. Ocul Immunol Inflamm 1-8.https://doi.org/10.1080/09273948.2020.1791346
Abu El-Asrar AM, Berghmans N, Al-Obeidan SA, Gikandi PW, Opdenakker G, Van Damme J, Struyf S (2020) Local cytokine expression profiling in patients with specific autoimmune uveitic entities. Ocul Immunol Inflamm 28:453–462. https://doi.org/10.1080/09273948.2019.1604974
Abu El-Asrar AM, Berghmans N, Al-Obeidan SA, Gikandi PW, Opdenakker G, Van Damme J, Struyf S (2020) Soluble cytokine receptor levels in aqueous humour of patients with specific autoimmune uveitic entities: sCD30 is a biomarker of granulomatous uveitis. Eye (Lond) 34:1614–1623. https://doi.org/10.1038/s41433-019-0693-7
Croft M, Siegel RM (2017) Beyond TNF: TNF superfamily cytokines as targets for the treatment of rheumatic diseases. Nat Rev Rheumatol 13:217–233. https://doi.org/10.1038/nrrheum.2017.22
International Study Group for Behcet’s Disease (1990) Criteria for diagnosis of Behcet’s disease. Lancet 335:1078–1080
Ohguro N, Sonoda KH, Takeuchi M, Matsumura M, Mochizuki M (2012) The 2009 prospective multi-center epidemiologic survey of uveitis in Japan. Jpn J Ophthalmol 56:432–435. https://doi.org/10.1007/s10384-012-0158-z
Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140:509–516
Takeda A, Yoshikawa H, Fukuhara T, Hikita S, Hijioka K, Otomo T, Arita R, Hisatomi T, Kimura K, Yoshida S, Kawano Y, Sonoda KH, Ishibashi T (2015) Distinct profiles of soluble cytokine receptors between B-cell vitreoretinal lymphoma and uveitis. Invest Ophthalmol Vis Sci 56:7516–7523. https://doi.org/10.1167/iovs.15-17465
Smith JR, Stempel AJ, Bharadwaj A, Appukuttan B (2016) Involvement of B cells in non-infectious uveitis. Clin Transl Immunol 5:e63. https://doi.org/10.1038/cti.2016.2
Mockel T, Basta F, Weinmann-Menke J, Schwarting A (2021) B cell activating factor (BAFF): Structure, functions, autoimmunity and clinical implications in Systemic Lupus Erythematosus (SLE). Autoimmun Rev 20:102736. https://doi.org/10.1016/j.autrev.2020.102736
Ueda-Hayakawa I, Tanimura H, Osawa M, Iwasaka H, Ohe S, Yamazaki F, Mizuno K, Okamoto H (2013) Elevated serum BAFF levels in patients with sarcoidosis: association with disease activity. Rheumatology (Oxford) 52:1658–1666. https://doi.org/10.1093/rheumatology/ket186
Saussine A, Tazi A, Feuillet S, Rybojad M, Juillard C, Bergeron A, Dessirier V, Bouhidel F, Janin A, Bensussan A, Bagot M, Bouaziz JD (2012) Active chronic sarcoidosis is characterized by increased transitional blood B cells, increased IL-10-producing regulatory B cells and high BAFF levels. PLoS ONE 7:e43588. https://doi.org/10.1371/journal.pone.0043588
Sumita Y, Murakawa Y, Sugiura T, Wada Y, Nagai A, Yamaguchi S (2012) Elevated BAFF levels in the cerebrospinal fluid of patients with neuro-Behcet’s disease: BAFF is correlated with progressive dementia and psychosis. Scand J Immunol 75:633–640. https://doi.org/10.1111/j.1365-3083.2012.02694.x
Lasave AF, You C, Ma L, Abusamra K, Lamba N, Valdes Navarro M, Meese H, Foster CS (2018) Long-term outcomes of rituximab therapy in patients with noninfectious posterior uveitis refractory to conventional immunosuppressive therapy. Retina 38:395–402. https://doi.org/10.1097/IAE.0000000000001563
Shabgah AG, Shariati-Sarabi Z, Tavakkol-Afshari J, Mohammadi M (2019) The role of BAFF and APRIL in rheumatoid arthritis. J Cell Physiol 234:17050–17063. https://doi.org/10.1002/jcp.28445
Gheita TA, Raafat H, Khalil H, Hussein H (2013) Serum level of APRIL/BLyS in Behcet’s disease patients: clinical significance in uveitis and disease activity. Mod Rheumatol 23:542–546. https://doi.org/10.1007/s10165-012-0694-x
Chen M, Lin X, Liu Y, Li Q, Deng Y, Liu Z, Brand D, Guo Z, He X, Ryffel B, Zheng SG (2014) The function of BAFF on T helper cells in autoimmunity. Cytokine Growth Factor Rev 25:301–305. https://doi.org/10.1016/j.cytogfr.2013.12.011
Quan R, Chen C, Yan W, Zhang Y, Zhao X, Fu Y (2020) BAFF blockade attenuates inflammatory responses and intestinal barrier dysfunction in a murine endotoxemia model. Front Immunol 11:570920. https://doi.org/10.3389/fimmu.2020.570920
Abu El-Asrar AM, Berghmans N, Al-Obeidan SA, Mousa A, Opdenakker G, Van Damme J, Struyf S (2016) The cytokine interleukin-6 and the chemokines CCL20 and CXCL13 are novel biomarkers of specific endogenous uveitic entities. Invest Ophthalmol Vis Sci 57:4606–4613. https://doi.org/10.1167/iovs.16-19758
Wolf J, Rose-John S, Garbers C (2014) Interleukin-6 and its receptors: a highly regulated and dynamic system. Cytokine 70:11–20. https://doi.org/10.1016/j.cyto.2014.05.024
Mustafi D, Do BK, Rodger DC, Rao NA (2020) Relationship of epiretinal membrane formation and macular edema development in a large cohort of uveitic eyes. Ocul Immunol Inflamm 1-7.https://doi.org/10.1080/09273948.2019.1704026
Nazari H, Dustin L, Heussen FM, Sadda S, Rao NA (2012) Morphometric spectral-domain optical coherence tomography features of epiretinal membrane correlate with visual acuity in patients with uveitis. Am J Ophthalmol 154(78–86):e71. https://doi.org/10.1016/j.ajo.2012.01.032
Lehpamer B, Moshier E, Pahk P, Goldberg N, Ackert J, Godbold J, Jabs DA (2014) Epiretinal membranes in uveitic macular edema: effect on vision and response to therapy. Am J Ophthalmol 157:1048–1055. https://doi.org/10.1016/j.ajo.2014.01.020
Tranos P, Scott R, Zambarakji H, Ayliffe W, Pavesio C, Charteris DG (2006) The effect of pars plana vitrectomy on cystoid macular oedema associated with chronic uveitis: a randomised, controlled pilot study. Br J Ophthalmol 90:1107–1110. https://doi.org/10.1136/bjo.2006.092965
Henry CR, Becker MD, Yang Y, Davis JL (2018) Pars plana vitrectomy for the treatment of uveitis. Am J Ophthalmol 190:142–149. https://doi.org/10.1016/j.ajo.2018.03.031
Wang KX, Denhardt DT (2008) Osteopontin: role in immune regulation and stress responses. Cytokine Growth Factor Rev 19:333–345. https://doi.org/10.1016/j.cytogfr.2008.08.001
Bassyouni IH, El-Wakd MM, Bassyouni RH (2013) Soluble levels of osteopontin in patients with Behcet’s disease: association with disease activity and vascular involvement. J Clin Immunol 33:361–367. https://doi.org/10.1007/s10875-012-9820-y
Kitamura M, Iwabuchi K, Kitaichi N, Kon S, Kitamei H, Namba K, Yoshida K, Denhardt DT, Rittling SR, Ohno S, Uede T, Onoe K (2007) Osteopontin aggravates experimental autoimmune uveoretinitis in mice. J Immunol 178:6567–6572. https://doi.org/10.4049/jimmunol.178.10.6567
Iwata D, Kitamura M, Kitaichi N, Saito Y, Kon S, Namba K, Morimoto J, Ebihara A, Kitamei H, Yoshida K, Ishida S, Ohno S, Uede T, Onoe K, Iwabuchi K (2010) Prevention of experimental autoimmune uveoretinitis by blockade of osteopontin with small interfering RNA. Exp Eye Res 90:41–48. https://doi.org/10.1016/j.exer.2009.09.008
Saas P, Boucraut J, Walker PR, Quiquerez AL, Billot M, Desplat-Jego S, Chicheportiche Y, Dietrich PY (2000) TWEAK stimulation of astrocytes and the proinflammatory consequences. Glia 32:102–107
Wiley SR, Winkles JA (2003) TWEAK, a member of the TNF superfamily, is a multifunctional cytokine that binds the TweakR/Fn14 receptor. Cytokine Growth Factor Rev 14:241–249. https://doi.org/10.1016/s1359-6101(03)00019-4
Icli A, Cure MC, Cure E, Arslan S, Unal M, Sakiz D, Ozucan M, Toker A, Turkmen K, Kucuk A (2018) Soluble tumor necrosis factor (TNF)-like weak inducer of apoptosis (Tweak) independently predicts subclinical atherosclerosis in Behcet’s disease. Acta Medica (Hradec Kralove) 61:86–92. https://doi.org/10.14712/18059694.2018.123
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS) through KAKENHI Grant Numbers JP18K09471 and JP21K09745 (grants C to AT) from the Ministry of Education, Science, Sports and Culture, Japan (Tokyo, Japan), and grants from Novartis Pharma Research Grants (AT; Tokyo, Japan), Alcon Pharma Research Grants (AT; Tokyo, Japan), and AMO Japan Research Grants (AT; Tokyo, Japan).
Author information
Authors and Affiliations
Contributions
Conceptualization: Atsunobu Takeda and Koh-Hei Sonoda; data curation: Atsunobu Takeda, Yusuke Murakami, and Toshio Hisatomi; formal analysis: Eiichi Hasegawa; investigation: Atsunobu Takeda, Keijiro Ishikawa, and Shoji Notomi; methodology: Atsunobu Takeda, Kazuhiro Kimura; project administration: Nobuyo Yawata and Koh-Hei Sonoda; writing – original draft preparation: Atsunobu Takeda; writing – review and editing: Nobuyo Yawata and Koh-Hei Sonoda; funding acquisition: Atsunobu Takeda; resources: Atsunobu Takeda, Kazuhiro Kimura, and Koh-Hei Sonoda; supervision: Koh-Hei Sonoda. All authors have read and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Kyushu University Institutional Review Board for Clinical Research and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This work was approved by the Kyushu University Institutional Review Board for Clinical Research. Written informed consent was obtained from all the participants before any study procedures or examinations were performed.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare no competing interests.
Disclaimer
The funding sources had no role in the design and conduct of the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takeda, A., Hasegawa, E., Yawata, N. et al. Increased vitreous levels of B cell activation factor (BAFF) and soluble interleukin-6 receptor in patients with macular edema due to uveitis related to Behçet’s disease and sarcoidosis. Graefes Arch Clin Exp Ophthalmol 260, 2675–2686 (2022). https://doi.org/10.1007/s00417-022-05600-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05600-1