Abstract
Purpose
To compare anatomical and functional outcomes using brilliant blue G (BBG) vs triamcinolone acetonide (TA)-assisted ILM peeling in macular hole surgery (MHS).
Study design
Simple, comparative, retrospective, non-randomised, interventional single-centre study.
Methods
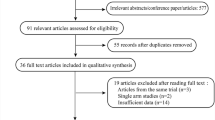
Ninety-four eyes of 94 patients with idiopathic macular holes (≥ stage 2) who underwent MHS at our centre were included. Patients with failed macular holes, post-traumatic macular holes, history of previous vitreoretinal surgery, high myopia (6 dioptres or more) or any other macular pathology potentially limiting visual acuity, such as diabetic retinopathy or age-related macular degeneration, were excluded. An OCT evaluation of hole status was followed by pars plana vitrectomy for each of these eyes. Those who underwent TA-assisted ILM peeling were considered as group 1 and those with BBG-assisted ILM peeling were considered as group 2. Primary outcome measures included anatomical hole closure and functional success in terms of change in visual acuity of ≥2 LogMAR lines. Various preoperative factors were also evaluated.
Results
Anatomical hole closure was achieved in 85 eyes (90.43%) and visual gain in 78 eyes (82.9%). Mean postoperative follow-up duration was 16.14 ± 1.95 months. No significant difference was found in anatomical and functional success between the two groups. Group 1 had a significantly higher incidence of postoperative glaucoma. Duration of symptoms of <12 months (p = 0.004) and preoperative visual acuity ≤1.0 LogMAR were related to anatomical success. However, greater visual gain was found in patients with chronic holes (≥12 months) (p = 0.046) and poor preoperative visual acuity (>1.0 LogMAR) (p = 0.001).
Conclusion
BBG-assisted ILM peeling offers an effective alternative to triamcinolone, with the added advantage of marked enhancement of vitreoretinal interface contrast with comparable hole closure rates and visual outcomes.

Similar content being viewed by others
References
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol 109:654–659
Kwok AK, Lai TY, Man-Chan W, Woo DC (2003) Indocyanine green assisted internal limiting membrane removal in stage 3 or 4 macular hole surgery. Br J Ophthalmol 87:71–74
Wendel RT, Patel AC, Kelly NE, Salzano TC, Wells JW, Novack GD (1993) Vitreous surgery for macular holes. Ophthalmology 100:1671–1676
Haritoglou C, Gass CA, Schaumberger M, Gandorfer A, Ulbig MW, Kampik A (2002) Long-term follow-up after macular hole surgery with internal limiting membrane peeling. Am J Ophthalmol 134:661–666
Smiddy WE, Feuer W, Cordahi G (2001) Internal limiting membrane peeling in macular hole surgery. Ophthalmology 108:1471–1476
Freeman WR, Azen SP, Kim JW, el-Haig W, Mishell DR, Bailey I (1997) Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol 115:11–21
Ruby AJ, Williams DF, Grand MG, Thomas MA, Meredith TA, Boniuk I, Olk RJ (1994) Pars plana vitrectomy for treatment of stage 2 macular holes. Arch Ophthalmol 112:359–364
Orellana J, Lieberman RM (1993) Stage III macular hole surgery. Br J Ophthalmol 77:555–558
Ryan EH Jr, Gilbert HD (1994) Results of surgical treatment of recent-onset full-thickness idiopathic macular holes. Arch Ophthalmol 112:1545–1553
Brooks HL Jr (2000) Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 107:1939–1948
Mester V, Kuhn F (2000) Internal limiting membrane removal in the management of full-thickness macular holes. Am J Ophthalmol 129:769–777
Margherio RR, Margherio AR, Williams GA, Chow DR, Banach MJ (2000) Effect of perifoveal tissue dissection in the management of acute idiopathic full-thickness macular holes. Arch Ophthalmol 118:495–498
Ando F, Sasano K, Ohba N, Hirose H, Yasui O (2004) Anatomic and visual outcome after indocyanine green-assisted peeling of the retinal internal limiting membrane in idiopathic macular hole surgery. Am J Ophthalmol 137:609–614
Morris R, Kuhn F, Witherspoon CD (1994) Hemorrhagic macular cysts. Ophthalmology 101:1
Liesenhoff O, Messmer EM, Pulur A, Kampik A (1996) Surgical management of complete macular foramina. Ophthalmologe 93:655–659
Uemoto R, Yamamoto S, Aoki T, Tsukahara I, Yamamoto T, Takeuchi S (2002) Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol 86:1240–1242
Rodrigues EB, Meyer CH, Kroll P (2005) Chromovitrectomy: a new field in vitreoretinal surgery. Graefes Arch Clin Exp Ophthalmol 243:291–293
Rodrigues EB, Penha FM, de Paula Fiod Costa E, Maia M, Dib E, Moraes M Jr, Meyer CH, Magalhaes O Jr, Melo GB, Stefano V, Dias AB, Farah ME (2010) Ability of new vital dyes to stain intraocular membranes and tissues in ocular surgery. Am J Ophthalmol 149:265–277
Rodrigues EB, Costa EF, Penha FM, Melo GB, Bottós J, Dib E, Furlani B, Lima VC, Maia M, Meyer CH, Höfling-Lima AL, Farah ME (2009) The use of vital dyes in ocular surgery. Surv Ophthalmol 54:576–617
Kumar A, Wagh VB, Prakash G, Nag TC, Prakash S et al (2005) Visual outcome and electron microscopic features of Indocyanine green-assisted internal limiting membrane peeling from macular hole of various etiologies. Indian J Ophthalmol 53:159–165
Kumar A, Prakash G, Singh RP (2002) Indocyanine green enhanced maculorrhexis in macular hole surgery. Indian J Ophthalmol 50:123–126
Rezai KA, Farrokh-Siar L, Ernest JT, van Seventer GA (2004) Indocyanine green induces apoptosis in human retinal pigment epithelial cells. Am J Ophthalmol 137:931–933
Meyer CH (2008) Toxicity of indocyanine green in vitreoretinal surgery. Vital dyes in vitreoretinal surgery. Dev Ophthalmol 42:69–81, Basel, Karger
Meyer CH (2008) Current concepts of Trypan blue in chromovitrectomy. Vital dyes in vitreoretinal surgery. Dev Ophthalmol 42:91–100, Basel, Karger
Li K, Wong D, Hiscott P, Stanga P, Groenewald C, McGalliard J (2003) Trypan blue staining of the internal limiting membrane and epiretinal membrane during vitrectomy: visual results and histopathological findings. Br J Ophthalmol 87:216–219
Perrier M, Sebag M (2003) Epiretinal membrane surgery assisted by Trypan blue. Am J Ophthalmol 135:909–911
Teba FA, Mohr A, Eckardt C, Wong D, Kusaka S, Joondeph BC, Feron EJ, Stalmans P, Van Overdam K, Melles GR (2003) Trypan blue staining in vitreoretinal surgery. Ophthalmology 110:2409–2412
Veckeneer M, van Overdam K, Monzer J, Kobuch K, van Marle W, Spekreijse H, van Meurs J (2001) Ocular toxicity study of Trypan blue injected into the vitreous cavity of rabbit eyes. Graefes Arch Clin Exp Ophthalmol 239:698–704
Jin Y, Uchida S, Yanagi Y, Aihara M, Araie M (2005) Neurotoxic effects of Trypan blue on rat retinal ganglion cells. Exp Eye Res 81:395–400
Rezai KA, Farrokh-Siar L, Gasyna EM, Ernest JT (2004) Trypan blue induces apoptosis in human retinal pigment epithelial cells. Am J Ophthalmol 138:492–495
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, Kubota T, Ishibashi T (2006) Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G assisted membrane peeling. Retina 26:631–636
Meyer CH (2008) Brilliant blue in vitreoretinal surgery. Vital dyes in vitreoretinal surgery. Dev Ophthalmol 42:115–125, Basel, Karger
Enaida H, Hisatomi T, Goto Y, Hata Y, Ueno A, Miura M, Kubota T, Ishibashi T (2006) Preclinical investigation of internal limiting membrane peeling and staining using intravitreal brilliant blue G. Retina 26:623–630
Tornambe PE, Poliner LS, Cohen RG (1998) Definition of macular hole surgery end points: elevated/open, flat/open, flat/closed. Retina 18:286–287
Kumagai K, Furukawa M, Ogino N, Uemura A, Demizu S, Larson E (2004) Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina 24:721–727
Abdelkader E, Lois N (2008) Internal limiting membrane peeling in vitreoretinal surgery. Surv Ophthalmol 53:368–396
Kwok AK, Lai TY, Wong VW (2005) Idiopathic macular hole surgery in Chinese patients: a randomised study to compare Indocyanine green-assisted internal limiting membrane peeling with no internal limiting membrane peeling. Hong Kong Med J 11:259–266
Smiddy WE, Flynn HW Jr (2004) Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol 137:525–537
Kwok AK, Li WW, Pang CP, Lai TY, Yam GH, Chan NR, Lam DS (2001) Indocyanine green staining and removal of internal limiting membrane in macular hole surgery: histology and outcome. Am J Ophthalmol 132:178–183
Yooh HS, Brooks HL, Capone A, L’Hernault NL, Grossniklaus HE (1996) Ultrastructural features of tissue removed during idiopathic macular hole surgery. Am J Ophthalmol 122:67–75
Da Mata AP, Burk SE, Riemann CD, Rosa RH Jr, Snyder ME, Petersen MR, Foster RE (2001) Indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for macular hole repair. Ophthalmology 108:1187–1192
Nomoto H, Shiraga F, Yamaji H, Fukuda K, Baba T, Takasu I, Ohtsuki H (2008) Macular hole surgery with triamcinolone acetonide-assisted internal limiting membrane peeling: one-year results. Retina 28:427–432
Horio N, Horiguchi M, Yamamoto N (2005) Triamcinolone-assisted internal limiting membrane peeling during idiopathic macular hole surgery. Arch Ophthalmol 123:96–99
Peyman GA, Cheema R, Conway MD, Fang T (2000) Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloid during pars plana vitrectomy. Retina 20:554–555
Shah GK, Rosenblatt BJ, Blinder KJ, Grand MG, Smith M (2005) Triamcinolone assisted internal membrane peeling. Retina 25:972–975
Shah GK, Rosenblatt BJ, Smith M (2004) Internal limiting membrane peeling using triamcinolone acetonide: histopathologic confirmation. Am J Ophthalmol 138:656–657
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J (1999) Macular hole surgery with internal limiting membrane peeling and intravitreous air. Ophthalmology 106:1392–1397
Funata M, Wendel RT, de la Cruz Z, Green WR (1992) Clinicopathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina 12:289–298
Kumar A, Sinha S, Gupta A (2010) Residual triamcinolone acetonide at macular hole after vitreous surgery. Indian J Ophthalmol 58:232–234
Fukukita M, Sasoh M, Matsubara H, Furuta M, Okawa C, Ito Y et al (2007) Triamcinolone acetonide remaining on the fovea after successful macular hole closure. Retina 27:122–123
Author information
Authors and Affiliations
Corresponding author
Additional information
No financial support has been received by any author, and none of the authors have proprietary interest in the subject matter presented.
Authors have full control of all primary data, and they agree to allow Graefe's Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Rights and permissions
About this article
Cite this article
Kumar, A., Gogia, V., Shah, V.M. et al. Comparative evaluation of anatomical and functional outcomes using brilliant blue G versus triamcinolone assisted ILM peeling in macular hole surgery in Indian population. Graefes Arch Clin Exp Ophthalmol 249, 987–995 (2011). https://doi.org/10.1007/s00417-010-1609-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-010-1609-1