Abstract
Background
Ophthalmodynamometric studies can provide useful clinical information regarding glaucoma, cerebrospinal fluid pressure, and vascular disease but are affected by variable reproducibility and unknown calibration of force in terms of intraocular pressure (IOP). The aim of this study was to calculate calibration factors and identify key design principles using three different types of ophthalmodynamometers.
Methods
We constructed a modified ophthalmodynamometer named OcuDyn using a large contact lens inside a ring force transducer with continuous signal acquisition and averaging. OcuDyn and Sisler ophthalmodynamometers were applied to isolated pig eyes which were cannulated and connected to a fluid reservoir and a pressure transducer to measure induced IOP at increasing force application. Using these two devices and a Meditron ophthalmodynamometer, we measured the minimum ophthalmodynamometric force (ODF) required to induce pulsation in the hemi-veins and diastolic retinal artery of each eye in glaucoma patient volunteers and family members.
Results
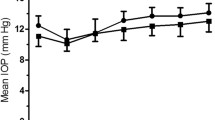
Blood pressure was measured with the sphygmomanometer cuff held at eye level. In pigs, the relationship between induced IOP and ODF was strong (minimum r > 0.98, p < 0.001). In humans, the pressure increment (blood pressure – baseline IOP) correlated highly with human arterial ODF (r = 0.83, n = 75, p < 0.001, mean slope 0.32). Mean coefficients of variation were 12.4% (n = 66) for veins and 5.6% (n = 39) for arteries in diastole; these results did not differ significantly with those from the Meditron but were significantly lower than results with the Sisler (20%, p = 0.0014).
Conclusions
Linearity between induced IOP and ODF is strong, suggesting that calibration of 0.32 mmHg/g for OcuDyn or using two point blood pressure measures allows for valid interpolation. The better optics of the Meditron and OcuDyn result in more repeatable end-point determination and outweigh benefits conferred by signal averaging or slit lamp mounting. We calculate calibration factors of 0.89 mmHg/arbitrary unit for Meditron and 0.82 mmHg/g for Sisler. These factors may be useful in the estimation of ocular vascular, orbital, and cerebrospinal fluid pressures.




Similar content being viewed by others
References
Firsching R, Schutze M, Motschmann M, Behrends-Baumann W (2000) Venous ophthalmodynamometry: a noninvasive method for assessment of intracranial pressure. J Neurosurg 93:33–36
Firsching R, Schutze M, Motschmann M, Behrens-Baumann W, Meyer-Schwickerath R (1998) Non-invasive measurement of intracranial pressure. Lancet 351:523–524
Querfurth HW, Arms SW, Lichy CM, Irwin WT, Steiner T (2004) Prediction of intracranial pressure from noninvasive transocular venous and arterial hemodynamic measurements: a pilot study. Neurocrit Care 1:183–194
Jonas JB, Pfeil K, Chatzikonstantinou A, Rensch F (2008) Ophthalmodynamometric measurement of central retinal vein pressure as surrogate of intracranial pressure in idiopathic intracranial hypertension. Graefes Arch Clin Exp Ophthalmol 246:1059–1060
Beaumont PE, Kang HK (1994) Ophthalmodynamometry and corticosteroids in central retinal vein occlusion. Aust NZ J Ophthalmol 22:271–274
Jonas JB (2004) Ophthalmodynamometric measurement of orbital tissue pressure in thyroid-associated orbitopathy. Acta Ophthalmol Scand 82:239
Jonas JB, Kaltakji F (2008) Ophthalmodynamometry and ischemic ophthalmopathy. Graefes Arch Clin Exp Ophthalmol 246:783–784
Jonas JB, Harder B (2008) Central retinal artery and vein collapse pressure in giant cell arteritis versus nonarteritic anterior ischaemic optic neuropathy. Eye 22:556–558
Morgan WH, Hazelton ML, Azar SL, House PH, Yu DY, Cringle SJ, Balaratnasingam C (2004) Retinal venous pulsation in glaucoma and glaucoma suspects. Opthalmology 111:1489–1494
Jonas JB (2003) Central retinal artery and vein collapse pressure in eyes with chronic open-angle glaucoma. Br J Ophthalmol 87:949–951
Jonas JB (2003) Reproducibility of ophthalmodynamometric measurements of central retinal artery and vein collapse pressure. Br J Ophthalmol 87:577–579
Sisler HA (1972) Optical-corneal pressure ophthalmodynamometer. Am J Ophthalmol 74:987–988
Morgan WH, Balaratnasingam C, Hazelton ML, House PH, Cringle SJ, Yu DY (2005) The force required to induce hemivein pulsation is associated with the site of maximal field loss in glaucoma. Invest Ophthalmol Vis Sci 46:1307–1312
Jonas JB, Harder B (2007) Ophthalmodynamometric differences between ischemic vs nonischemic retinal vein occlusion. Am J Ophthalmol 143:112–116
Jonas JB (2004) Ophthalmodynamometric determination of the central retinal vessel collapse pressure correlated with systemic blood pressure. Br J Ophthalmol 88:501–504
Meyer-Schwickerath R, Stodtmeister R, Hartmann K (2004) Non-invasive determination of intracranial pressure. Physiological basis and practical procedure. Klin Monatsbl Augenheilkd 221:1007–1011
Lowe RD (1962) Calibration of Bailliart's ophthalmodynamometer. Arch Ophthalmol 67:424–427
Pierscionek BK, Ashkenazi I, Schachter J (2007) The effect of changing intraocular pressure on the corneal and scleral curvatures in the fresh porcine eye. Br J Ophthalmol 91:801–803
Bartholomew LR, Pang DX, Sam DA, Cavender JC (1997) Ultrasound biomicroscopy of globes from young adult pigs. Am J Vet Res 58:942–948
Morgan WH, Yu DY, Alder VA, Cringle SJ, Constable IJ (1998) Relation between pressure determined by ophthalmodynamometry and aortic pressure in the dog. Br J Ophthalmol 82:821–825
Fung YC (1984) Biodynamics: circulation. Springer, Berlin Heidelberg New York, pp 132–134
Feigl EO (1974) The arterial system. In: Ruch TD, Patton HD (eds) Physiology and biophysics; circulation, respiration and fluid balance. W B Saunders, Philadelphia, pp 117–125
Lovasik JV, Kothe AC, Kergoat H (1993) Comparison of noninvasive methods to derive the mean central retinal artery pressure in man. Optom Vis Sci 70:1005–1011
R Development Core Team. R: A language and environment for statistical computing. (2.7.1 (2008-06-23)). 2008. Vienna, Austria, R Foundation for Statistical Computing. http://cran.r-project.org/
Jonas JB (2004) Retinal arterial collapse pressure in eyes with retinal arterial occlusive diseases. Br J Ophthalmol 88:589
Morgan WH, Chauhan BC, Yu DY, Cringle SJ, Alder VA, House PH (2002) Optic disc movement with variations in intraocular and cerebrospinal fluid pressure. Inv Ophthalmol Vis Sci 43:3236–3242
Inoue R, Hangai M, Kotera Y, Nakanishi H, Mori S, Morishita S, Yoshimura N (2009) Three-dimensional high-speed optical coherence tomography imaging of lamina cribrosa in glaucoma. Ophthalmology 116:214–222
Morgan WH, Hazelton ML, Balaratnasingam C, Chan H, House PH, Barry CJ, Cringle SJ, Yu DY (2009) The association between retinal vein ophthalmodynamometric force change and optic disc excavation. Br J Ophthalmol 93:594–596
Acknowledgements
This work is supported by the National Health and Medical Research Council of Australia and the Australian Research Council Centre of Excellence in Vision Science. The authors wish to thank Dean Darcey for his invaluable assistance.
Financial relationship
One author (D. Ezekial) has a financial interest in contact lens manufacture. Two authors are supported by the National Health and Medical Research Council which also supported this work. The authors have full control of all primary data and they agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morgan, W.H., Cringle, S.J., Kang, M.H. et al. Optimizing the calibration and interpretation of dynamic ocular force measurements. Graefes Arch Clin Exp Ophthalmol 248, 401–407 (2010). https://doi.org/10.1007/s00417-009-1288-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1288-y