Abstract
Background
At the time of posterior subtenon infusion of triamcinolone acetonide (STI-TA) in patients with diabetic macular edema (DME), drug reflux of TA has sometimes been observed from the conjunctival incision site. We investigated the influence of this reflux on regression of DME and postoperative intraocular pressure (IOP).
Methods
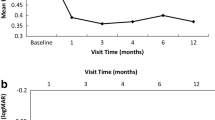
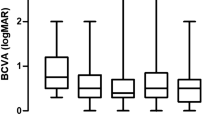
STI-TA was performed on one hundred and twenty-four eyes of 88 consecutive patients with DME. Eligible eyes were divided into two groups: those with observed drug reflux of TA and those without observed drug reflux of TA. Visual acuity (VA), foveal thickness (FT) and IOP were monitored in each eye for up to 12 weeks after STI-TA.
Results
STI-TA with drug reflux was observed in ten individual eyes of seven patients. These patients were significantly younger than those patients without observed drug reflux. After STI-TA, both improvement of VA and regression of FT in reflux(+) eyes were less than in reflux(-) eyes. Postoperative IOP elevation in reflux(+) eyes was much higher, and four of the ten eyes needed anti-glaucoma therapy. This was in contrast to three of the 118 eyes without drug reflux that required anti-glaucoma therapy.
Conclusions
At the time of STI-TA in DME, drug reflux of TA is a risk factor not only for insufficient reduction of edema, but also for postoperative IOP elevation.


Similar content being viewed by others
References
Moss SE, Klein R, Klein BEK (1988) The incidence of visual loss in a diabetic population. Ophthalmology 95:1340–1348
Jonas JB, Kreissig I, Sofker A, Degenring RF (2003) Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol 121:57–61, doi:10.1001/archopht.121.5.729
Massin P, Andren F, Haouchine B, Erginay A, Bergmann JF, Benosman R, Caulin C, Gaudric A (2004) Intravitreal triamcinolone acetonide for diabetic macular edema-Preliminary results of a prospective controlled trial-. Ophthalmology 111:218–225, doi:10.1016/j.ophtha.2003.05.037
Jonas JB, Degenring RF, Kreissig I, Akkoyun I, Kamppeter BA (2005) Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Ophthalmology 112:593–598, doi:10.1016/j.ophtha.2004.10.042
Moshfeghi DM, Kaiser PK, Scott IU, Sears JE, Benz M, Sinesterra JP, Kaiser RS, Bakri SJ, Maturi RK, Belmont J, Beer PM, Murray TG, Quiroz-Mercado H, Mieler WF (2003) Acute endophthalmitis following intravitreal triamcinolone acetonide injection. Am J Ophthalmol 136:791–796, doi:10.1016/S0002-9394(03)00483-5
Jonas JB, Spandau UH, Schlichtenbrede F (2008) Short-term complication of intravitreal injections of triamcinolone and bevacizumab. Eye 22:590–591, doi:10.1038/eye.2008.10
Cellini M, Pazzaglia A, Zamparini E, Leonetti P, Campos EC (2008) Intravitreal vs. subtenon triamcinolone acetonide for the treatment of diabetic cystoid macular edema. BMC Ophthalmol 8(5)
Choi YJ, Oh IK, Oh JR, Huh K (2006) Intravitreal versus posterior subtenon injection of triamciolone acetonide for diabetic macular edema. Korean J Ophthalmol 20:205–209
Bonini-Filho MA, Jorge R, Barbosa JC, Calucci D, Cardillo JA, Costa RA (2005) Intravitreal injection versus sub-tenon's infusion of triamcinolone acetonide for refractory diabetic macular edema: A randomized clinical trial. Invest Ophthalmol Vis Sci 46:3845–3849, doi:10.1167/iovs.05-0297
Lee CM, Olk J, Akduman L (2000) Combined modified grid and panretinal photocoagulation for diffuse diabetic macular edema and proliferative diabetic retinopathy. Ophthalmic Surg Lasers 31:292–300
Shimura M, Nakazawa T, Yasuda K, Shiono T, Nishida K (2007) Pretreatment of posterior subtenon injection of triamcinolone acetonide has beneficial effects for grid pattern photocoagulation against diffuse diabetic macular edema. Br J Ophthalmol 91:449–454, doi:10.1136/bjo.2006.106336
Shimura M, Yasuda K, Shiono T (2006) Posterior subtenon injection of triamcinolone acetonide prevents pan-retinal photocoagulation-induced visual dysfunction in patients with severe diabetic retinopathy and good vision. Ophthalmology 113:381–387, doi:10.1016/j.ophtha.2005.10.035
Lee SJ, Kim ES, Geroski DH, McCarey BE, Edelbauser HF (2008) Pharmacokinetics of intraocular drug delivery of oregon green 488-labeled triamcinolone by subtenon injection using ocular fluorophotometry in rabbit eyes. Invest Ophthalmol Vis Sci 49:4506–4514, doi:10.1167/iovs.08-1989
Inoue M, Takeda K, Morita K, Yamada M, Tanigawa Y, Oguchi Y (2004) Vitreous concentration of triamcinolone acetonide in human eyes after intravitreal or subtenon injection. Am J Ophthalmol 138:1046–1048, doi:10.1016/j.ajo.2004.05.028
Thomas ER, Wang J, Ege E, Mdsen R, Haisworth DP (2006) Intravitreal triamcinolone acetonide concentration after subtenon injection. Am J Ophthalmol 142:860–861, doi:10.1016/j.ajo.2006.05.023
Iwao K, Inatani M, Kawaji T, Koga T, Mawatari Y, Tanihara H (2007) Frequency and risk factors for intraocular pressure elevation after posterior sub-Tenon capsule triamcinolone acetonide injection. J Glaucoma 16:251–256, doi:10.1097/IJG.0b013e31802d696f
Hirooka K, Shiraga F, Tanaka S, Baba T, Mandai H (2006) Risk factors for elevated intraocular pressure after trans-tenon retrobulbar injection of triamcinolone. Jpn J Ophthalmol 50:235–238, doi:10.1007/s10384-005-0306-9
Rozsa FW, Reed DM, Scott KM, Pawar H, Moroi SE, Kijek TG, Krafchak CM, Othman MI, Vollrath D, Elner VM, Richards JE (2006) Gene expression profile of human trabecular meshwork cells in response to long-term dexamethasone exposure. Mol Vis 12:125–141
Clark AF, Wilson K, McCartney MD, Miggans ST, Kunkle M, Howe W (1994) Glucocorticoid-induced formation of cross-linked actin networks in cultured human trabecular meshwork cells. Invest Ophthalmol Vis Sci 35:281–194
Saadat F, Raji A, Zomorodian K, Eslami MB, Pezeahiki M, Khorramizadeh MR, Aalizadeh N (2003) Alteration in matrixmetalloproteinases (MMPS) activity in fibroblast cell line by dexamethasone: A possible mechanism in corticosteroid-induced glaucoma. Iran J Allergy Asthma Immunol 2:145–148
Coca-Prados M, Escribano J (2007) New perspectives in aqueous humor secretion and in glaucoma: the ciliary body as a multifunctional neuroendocrine gland. Prog Retin Eye Res 26:239–262, doi:10.1016/j.preteyeres.2007.01.002
Kaiser PK, Goldberg MF, Davis AA, Group. TAACS (2007) Posterior juxtascleral depot administration of anecortave acetate. Surv Ophthalmol 52:S62–S69, doi:10.1016/j.survophthal.2006.10.015
Inatani M, Iwao K, Kawaji T, Hirano Y, Ogura Y, Hirooka K, Shiraga F, Nakanishi Y, Yamamoto H, Negi A, Shimonagano Y, Sakamoto T, Shima C, Matsumura M, Tanihara H (2008) Intraocular pressure elevation after injection of triamcinolone acetonide: A multicenter retrospective case-control study. Am J Ophthalmol 145:676–681, doi:10.1016/j.ajo.2007.12.010
Meyer E, Ludatscher RM, Miller B, Lichtig C (1992) Connective tissue of the orbital cavity in retinal detachment: an ultrastructural study. Ophthalmic Res 24:365–371
Acknowledgements
The authors thank Dr. Norio Sugimoto in Theranostic Instruments Research Laboratories for technical support of statistical analyses, and also thank Dr. Dee Worman for English editing and useful comments. This study was supported by 2006-2008 scientific grants in aid for clinical research by NTT East Japan Tohoku Hospital
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary Interest None.
Rights and permissions
About this article
Cite this article
Shimura, M., Yasuda, K., Nakazawa, T. et al. Drug reflux during posterior subtenon infusion of triamcinolone acetonide in diffuse diabetic macular edema not only brings insufficient reduction but also causes elevation of intraocular pressure. Graefes Arch Clin Exp Ophthalmol 247, 907–912 (2009). https://doi.org/10.1007/s00417-009-1074-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1074-x