Abstract
Background
The purpose of this study was to determine age-dependent values for mean sensitivity, mean deviation, and loss variance for normal children age 6 through 13 years, using the Octopus 301 perimeter and the Tendency Oriented Perimetry 32 (TOP-32) program.
Methods
Healthy children from 6 through 13 years of age with a visual acuity of 20/20 OU and at least 60 arc seconds of stereopsis were recruited. They were tested on the Octopus 301 perimeter using the TOP-32 program, and each eye was tested twice during one session. Results for all four tests were averaged for each subject, and the average was used for statistical analysis. The main outcome measures were mean sensitivity, mean deviation, and loss variance by age. The test duration, learning and fatigue effects, and the influence of false positive responses on the average mean sensitivity were also analyzed.
Results
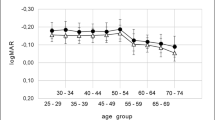
There were 142 subjects tested. Six-year-old children showed high intersubject variability and were excluded (N=23). The average age of the remaining 7- to 13-year-old cohort (N=119) was 9.8 ± 1.7 years. The average test duration was 2.9 ± 0.3 min. The average mean sensitivity was 28.7 ± 1.9 dB. The mean sensitivities for tests 1 through 4 were 28.14, 28.63, 28.96, and 28.92 dB, respectively. The average mean deviation was 0.4 ± 1.9 dB. The slope of the regression line for mean sensitivity vs age was −0.018 ± 0.165 dB/year, which was not significantly different from zero (two-tailed t test, p=0.83). The false positive catch trial rate was high (mean 26%) and was independent of age. When the data from subjects who had more than two false positive catch trial responses on any one test were eliminated, the mean sensitivity decreased to 28.3 ± 1.9 dB.
Conclusions
When testing patients age 7 through 13 years on the Octopus 301 perimeter using the TOP-32 program, comparison against the programmed normal mean sensitivity value for 20-year-old subjects (29.0 dB) is appropriate. During a sequence of four tests, both learning and fatigue effects are evident. The false positive response rate is naturally high regardless of age, and children should not be overencouraged to respond during testing.




Similar content being viewed by others
References
Barnard NA (1989) Kinetic outline perimetry as a technique for examining the visual fields of young children (letter). Ophthalmic Physiol Opt 9:463–464
Bengtsson B, Heijl A (1998) SITA Fast, a new rapid perimetric threshold test: description of methods and evaluation in patients with manifest and suspect glaucoma. Acta Ophthalmol Scand 76:431–437
Bengtsson B, Olsson J, Heijl A, Rootzen H (1997) A new generation of algorithms for computerized threshold perimetry, SITA. Acta Ophthalmol Scand 75:368–375
Brown SM, Morales J (2005) Short automated static perimetry in children with ocular abnormalities. Perimetry Update (in press)
Donahue SP, Porter A (2001) SITA visual field testing in children. J AAPOS 5:114–117
González de la Rosa M, Bron A, Morales J, Sponsel WE (1996) TOP perimetry: a theoretical evaluation (JERMOV abstract). Vision Res 36:88
Gonzales de la Rosa MG, Pinero AM, Hernandez MG (1999) Reproducibility of the TOP algorithm results versus those obtained with the bracketing procedure. Perimetry Update 52–58
Kremer I, Nissenkorn I, Lusky M, Yassur Y (1995) Late visual field changes following cryotherapy for retinopathy of prematurity stage 3. Br J Ophthalmol 79:267–269
Martinez A, Pareja A, Mantolan C, Sanchez M, Cordoves L, González de la Rosa M (1996) Results of tendency oriented perimetry (TOP) in a normal population. Vision Res 36:153 (JERMOV abstract)
Martinez Piñero A, Rodriguez J, Serrano M, González de la Rosa M (1998) Reproducibility and accuracy of tendency oriented perimetry (TOP). Invest Ophthalmol Vis Sci 39:S23 (ARVO abstract #95)
Mojon DS, Zulauf M (2003) Normal values of short-wavelength automated perimetry. Ophthalmologica 217:260–264
Morales J, Brown SM (2001) The feasibility of short automated static perimetry in children. Ophthalmology 108:157–162
Morales J, Weitzman ML, Gonzalez de la Rosa M (2000) Comparison between tendency oriented perimetry (TOP) and Octopus threshold perimetry. Ophthalmology 107:134–142
Mutlukan E, Damato BE (1993) Computerised perimetry with moving and steady fixation in children. Eye 7:554–561
Pareja Rios A, Arteaga Hernandez V, Gonazlez Hernandez M, Gonzalez de la Rosa M (2000) Efecto del uso de estímulos acústicos en perimetría. Arch Soc Canar Oftalmol 11:83–86
Quinn GE, Fea AM, Minguini N (1991) Visual fields in 4- to 10-year-old children using Goldmann and double-arc perimeters. J Pediatr Ophthalmol Strabismus 28:314–319
Quinn GE, Dobson V, Hardy RJ, Tung B, Phelps DL, Palmer EA (1996) Visual fields measured with double-arc perimetry in eyes with threshold retinopathy of prematurity from the cryotherapy for retinopathy of prematurity trial. The CRYO-Retinopathy of Prematurity Cooperative Group. Ophthalmology 103:1432–1437
Quinn GE, Miller DL, Evans JA, Tasman WE, McNamara JA, Schaffer DB (1996) Measurement of Goldmann visual fields in older children who received cryotherapy as infants for threshold retinopathy of prematurity. Arch Ophthalmol 114:425–428
Safran AB, Laffi GL, Bullinger A, Viviani P, de Weisse C, Desangles D, Tschopp C, Mermoud C (1996) Feasibility of automated visual field examination in children between 5 and 8 years of age. Br J Ophthalmol 80:515–518 (see comments)
Schwartz TL, Dobson V, Sandstrom DJ, van Hof-van Duin J (1987) Kinetic perimetry assessment of binocular visual field shape and size in young infants. Vision Res 27:2163–2175
Tschopp C, Safran AB, Viviani P, Bullinger A, Reicherts M, Mermoud C (1998) Automated visual field examination in children aged 5–8 years, Part I: experimental validation of a testing procedure. Vision Res 38:2203–2210
Tschopp C, Safran AB, Viviani P, Reicherts M, Bullinger A, Mermoud C (1998) Automated visual field examination in children aged 5–8 years, Part II: normative values. Vision Res 38:2211–2218
Tschopp C, Viviani P, Reicherts M, Bullinger A, Rudaz N, Mermoud C, Safran AB (1999) Does visual sensitivity improve between 5 and 8 years? A study of automated visual field examination. Vision Res 39:1107–1119
Wilson M, Quinn G, Dobson V, Breton M (1991) Normative values for visual fields in 4- to 12-year-old children using kinetic perimetry. J Pediatr Ophthalmol Strabismus 28:151–153 (discussion 154)
Acknowledgements
The authors wish to thank Hans Bebie, Ph.D., for assistance with data analysis and helpful critical review of the manuscript. Dr Bebie is a statistics consultant for Interzeag. We also wish to thank Dr Jose Morales for assistance with study design. This study was supported by a grant from Interzeag AG to the Occidental Pediatric Eye Research Fund at the Texas Tech University Health Sciences Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a grant from Interzeag AG, Berne, Switzerland, to the Occidental Pediatric Eye Research Fund. Mr Monhart is employed by Interzeag. No other author has a financial relationship with Interzeag. The authors have full control over the primary data and agree to allow the Journal to review the data if requested.
Rights and permissions
About this article
Cite this article
Brown, S.M., Bradley, J.C., Monhart, M.J. et al. Normal values for Octopus tendency oriented perimetry in children 7 through 13 years old. Graefe's Arch Clin Exp Ophthalmol 243, 886–893 (2005). https://doi.org/10.1007/s00417-005-1134-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-1134-9