Abstract
In 2015, we wrote a review in The Journal of Neurology summarizing the field of autoantibody-associated neurological diseases. Now, in 2023, we present an update of the subject which reflects the rapid expansion and refinement of associated clinical phenotypes, further autoantibody discoveries, and a more detailed understanding of immunological and neurobiological pathophysiological pathways which mediate these diseases. Increasing awareness around distinctive aspects of their clinical phenotypes has been a key driver in providing clinicians with a better understanding as to how these diseases are best recognized. In clinical practice, this recognition supports the administration of often effective immunotherapies, making these diseases ‘not to miss’ conditions. In parallel, there is a need to accurately assess patient responses to these drugs, another area of growing interest. Feeding into clinical care are the basic biological underpinnings of the diseases, which offer clear pathways to improved therapies toward enhanced patient outcomes. In this update, we aim to integrate the clinical diagnostic pathway with advances in patient management and biology to provide a cohesive view on how to care for these patients in 2023, and the future.
Similar content being viewed by others
Introduction
Since our last review of autoimmune encephalitis due to neuroglial surface targeted (NSAbs) antibodies [1], nascent research into these disorders has taken significant phenotypic, therapeutic, and biological strides. These immunotherapy-responsive conditions are typically associated with autoantibodies which target the extracellular domain of a central nervous system (CNS) cell surface protein. By contrast, most of the, predominantly paraneoplastic, syndromes characterized by ‘onconeuronal’ antibodies (Hu, Yo, Ma, Ri, and CV2/CRMP5) directed against intracellular antigens show a limited response to immunotherapy [2, 3]. Due to their inherent treatability, this review predominantly focuses on the ‘not to miss’ NSAb-mediated conditions. It also provides brief updates on two more recently described conditions associated with antibodies against the intracellular targets, glial fibrillary-associated protein (GFAP) and kelch-like protein 11 (KLH-11), both of which also show evidence of immunotherapy responsiveness.
In terms of advances, there has been further crystallization of the phenotypes of many of these disorders as well as examples of phenotypic expansion (clinical features of the most common forms are summarized in Fig. 1). Ongoing efforts to improve clinical descriptions aim to facilitate prompt diagnosis and institution of early treatment, which is proven to benefit patients [4, 5]. In parallel, we have learnt more about how patients fare in the longer term, the issues they face in their recovery, and the steps we can take to provide the best possible outcome for them. To this end, there are some innovative immunotherapeutics on the horizon and in clinical trials. In addition, significant progress has been made into understanding the immunological mechanisms underlying autoantibody production in these conditions and how these autoantibodies interact with their antigenic targets to induce neuronal dysfunction. These advances have created potential therapeutic opportunities to intervene directly in disease pathogenesis. Herein, we integrate these clinical and translational observations and explore how they have progressed the field.
Advances in phenotype. Heatmap illustrating the frequency of autoantibody-associated encephalitis syndromes with frequencies of features from rare or unknown (0 = teal) to common (4 = red). LGI1: leucine-rich glioma-inactivated 1. NMDAR: N-methyl-d-aspartate receptor. CASPR2 contactin-associated protein-like 2, MOG myelin oligodendrocyte protein, GABABR γ-aminobutyric acid B receptor, GABAAR γ-aminobutyric acid A receptor, AMPAR α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor, mGluR5 metabotropic glutamate receptor 5, GlyR glycine receptor, Sez6L2 SEZ6L2, seizure-related 6 homolog like 2, DNER delta/Notch-like epidermal growth factor-related receptor, GAD65 glutamic acid decarboxylase (65 kDa isoform), ANNA 1/2 anti-nuclear neuronal autoantibody type ½, PCA Purkinje cell cytoplasmatic autoantibodies, KLHL11 kelch-like protein 11, AK5 adenylate kinase 5, GFAP Glial Fibrillary acid protein
Leucine-rich glioma-inactivated 1 (LGI1)
Patients with LGI1-antibodies represent the commonest form of autoimmune encephalitis, which likely remains under-recognized due to its frequently insidious onset, the subtle focal seizures and its predilection for elderly males, a demographic not traditionally considered to have a primary autoimmune basis for their disease. These patients most commonly present with frequent, focal seizures [6], often the pathognomonic faciobrachial dystonic seizures (FBDS), discussed in more detail in our previous review. Other ictal semiologies have medial temporal lobe predominance and comprise bradycardia, thermal changes [7] or autonomic features such as piloerection [8]. All of these are preferentially sensitive to immunotherapies over anti-seizure medications (ASM).
Crucially, focal seizures precede limbic encephalitis (LE) in around 75% of cases, presenting an opportunity to alter the natural history of the disease [9,10,11]. The natural history of LGI1-antibody encephalitis appears to be the invariable progression from seizures alone to an established LE [4], with prominent memory disturbance, frequent and ASM-resistant seizures and psychiatric disturbances [12, 13]. As patients progress clinically, their paraclinical investigations become increasingly abnormal, whereas patients with LGI1-antibodies and FBDS alone typically do not have abnormal investigations [4, 12, 13]. Thereafter, increasing cognitive impairment parallels the accumulation of abnormal investigation findings, including hippocampal hyperintensities on T2-weighted MRI, ictal EEG abnormalities, and serum hyponatraemia, due to syndrome of inappropriate anti-diuretic hormone secretion (SIADH). Patients who develop LE are at risk of hippocampal atrophy associated with a fixed memory deficit with concomitant long-term disability [14, 15]. It is this, and a number of other residual cognitive deficits noted in these patients [16], which are potentially avoidable; it appears that early immunotherapy, particularly with corticosteroids [4, 17], may prevent the progression from FBDS to LE. This may be because immunotherapies are the mainstay of treatment for these seizures, and are far more effective than ASMs, or because they have an independent effect on altering disease progression. Overall, these findings emphasize the importance of neurologists being aware of the focal seizures as an early, treatable clinical presentation.
Another striking feature of patients with LGI1-antibodies is that around 25% exhibit adverse reactions toward certain first generation ASMs, specifically carbamazepine and phenytoin, including life-threatening Stevens–Johnson spectrum reactions [4]. This clinical observation led to the suspicion of a potential human leukocyte antigen (HLA) association in this patient group, as discussed below.
Contactin-associated protein-like 2 (CASPR2)
Patients with CASPR2-antibody-mediated neurological symptoms more often have symptoms affecting the peripheral nervous system, when compared to those with LGI1-antibodies. This was originally appreciated in the form of neuromyotonia (NMT), with peripheral nerve hyperexcitability, which manifests with cramps, stiffness, and fasciculations [18]. NMT can be seen in isolation or in combination with LE, along with a spectrum of prominent autonomic and sleep disturbance in the eponymous Morvan’s syndrome. In Morvan’s syndrome, CASPR2- and LGI1-antibodies often coexist in individual patients [19]. However, most patients with CASPR2-antibodies present with LE but without NMT. This LE can occur with ataxia, other movement disorders and neuropathic pain as additional features [19,20,21,22]. Although, as seen very rarely in patients with NMDAR-antibodies, patients with CASPR2-antibodies can infrequently have mono/oligo-symptomatic presentations: for example, isolated epilepsy, ataxia, or cognitive impairment [12, 19, 23].
Recent work has highlighted that movement disorders can be seen in ~ 35% of patients with CASPR2-antibodies, versus 4% with LGI1-antibodies [24]. A variety of movement disorders are appreciated including prominent ataxia, myoclonus, and tremor, as well as some more distinctive subtypes, including episodic ataxia, paroxysmal orthostatic segmental myoclonus of the legs, and continuous segmental spinal myoclonus [24, 25]. These create a significant, sometimes clinically challenging, overlap with functional neurological presentations.
Seizure semiology in patients with CASPR2-antibodies at presentation are predominantly focal (70%), with impaired awareness and limited motor components, or even limited to sensory seizures. Around 50% of patients go on to develop bilateral tonic clonic seizures later in their illness [26].
The pain in patients with CASPR2-antibodies has been recently detailed [27]. Significant, typically neuropathic, pain can be seen in 52% of patients with CASPR2-antibodies, compared to only 19% of patients with LGI1-antibodies. Patients were found to have normal nerve conduction studies but reduced intraepidermal nerve fiber densities. Pain in those with CASPR2-antibodies responded less well to immunotherapy than in LGI1-antibody patients, identifying an important unmet need in the current immunotherapy regimes. In vitro work demonstrated serum CASPR2-antibodies bound unmyelinated human sensory neurons and rat dorsal root ganglia, offering a biological substrate for the pain. In a cohort focusing on acquired neuromyotonia, secondary to either LGI1- and CASPR2- (plus now likely clinically irrelevant double-negative VGKC-) antibodies, pain was reported by patients as a common feature [28].
N-methyl-d-aspartate receptor-antibody encephalitis (NMDAR-AbE)
In NMDAR-AbE, neuropsychiatric symptoms are often preceded by viral prodromal symptoms, such as headache, fever, myalgia, and coryza, which usual occur around 4-14 days prior to disease onset. This is followed by an acute neuropsychiatric presentation with subsequent seizures and cognitive impairment. Around 1–4 weeks later, patients commonly develop a characteristic movement disorder [29], dysautonomia, and coma [30], which often precipitate intensive-care unit admission.
These features of NMDAR-AbE have been endophenotyped in further detail, highlighting some distinctive characteristics. Studies of the associated movement disorder show that it is a common feature, can be the presenting sign in children and adolescents [5], and, along with the neuropsychiatric symptoms, can be prolonged, continuing for a median of 112.5 days in this cohort [31]. Descriptions of the NMDAR-AbE-associated movement disorder by expert raters required a wide range of descriptors to capture its full phenomenology, characterized as an unusual combination of stereotypies, chorea, and dystonia not classically observed together in the other movement disorders [31, 32].
The prominent psychiatric symptoms associated with NMDAR-AbE are often the initial features of this illness in adults [30], with as many as 77% of patients first presenting to psychiatrists in some early series [33]. A systematic review encompassing 464 patients with NMDAR-AbE demonstrated the complexity of NMDAR-AbE-associated psychopathology, with the otherwise unusual combination of behavioral (68%), psychotic (67%), and mood (47%) features coexisting in individual patients. This constellation was not effectively captured by individual DSM-V or ICD-10 criteria for primary psychiatric syndromes [34]. In the future, we anticipate these studies, and similar studies expanding on this work, will aid clinicians in even earlier identification and treatment of this condition. This is likely to assist clinicians in starting treatment even prior to the availability of autoantibody results, something which is becoming our common practice and is associated with improved patient outcomes [5].
A long-standing clinical question concerns whether NMDAR-AbE can present as isolated psychiatric syndrome. This hypothesis seems attractive, since glutamatergic dysfunction is considered key to schizophrenia pathogenesis and disruption of NMDAR signaling via a variety of modalities capable of producing psychotic symptoms [35]. Furthermore, serum NMDAR-Abs were detected in patients with early, or first episode, presentations of psychosis [35]. However, some conflicting results have been published, with some investigators finding (typically small) differences between the prevalence of serum NMDAR-antibodies in patients with first-episode psychosis and controls [36,37,38], and others finding no differences [39, 40]. These studies, in turn, have propagated several more comparisons, which exhibit important differences in assay methodologies, timing of sample collection, and materials tested. While methodological differences may largely account for the heterogeneity in study findings, overall, it appears that CSF NMDAR-antibodies, ideally tested using a combination of tissue immunochemistry and live cell-based assays, provide very specific (albeit not 100%) diagnostic information. Indeed, positivity for this combination has not been found in large series of patients with schizophrenia [41] or first-episode psychosis [42, 43]. Overall, these studies suggest that while mono- and oligo-symptomatic NMDAR-AbE presentations (such as early forms of psychosis) may occur, typically in relapsing NMDAR-AbE, they represent the vast minority of cases. Rather, in most presentations, an abrupt onset together with the canonical diffuse and multimodal clinical features described above should be considered as the core features of NMDAR-AbE.
γ-Aminobutyric acid A receptor (GABAA-R)
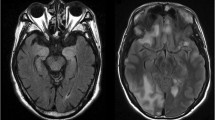
Patients with GABAA-R antibodies are more recently described. Early series described patients presenting with prominent seizures, which can be a potential cause of treatment resistant status epilepticus requiring intensive care. Patients were also frequently found to have memory impairment, disorientation, and psychiatric features [44, 45]. More recent series emphasize that, compared to other neuronal-surface antibody (NSAb)-associated encephalitides, the MRI imaging is abnormal in around 80% of cases [46] and is, in our experience, a highly specific diagnostic feature. Most patients have widely distributed, cortical–subcortical T2/FLAIR hyperintensities in predominantly the temporal or frontal lobes with limited diffusion restriction and are dynamic, responding to immunotherapy and relapses [47]. These imaging findings can be a clue to guide early autoantibody testing and administration of immunotherapies in the correct clinical context.
IgLON5
Much interest was generated from the description of patients with antibodies to IgLON5 [48], principally because this was the first NSAb-associated disease with a prominent and intriguing overlap between a neurodegenerative and immune-mediated disease. The clinical tempo and phenotype of patients with IgLON5-antibodies favor neurodegeneration, confirmed with prominent tau deposition on neuropathology. However, the autoantibodies target the extracellular domain of a neuronal protein, suggesting direct causality. The clinical presentation includes early prominent sleep disorders in REM and non-REM stages with dream re-enactment, stridor, a complex set of movement disorders, dysautonomia, and bulbar involvement. An important mimic, although reasonably consistently differentiated given the nature of the sleep disorder, is progressive supranuclear palsy [49]. Similar to the NMDAR-AbE movement disorder, that of IgLON5-antibodies spans a wide variety of clinical phenomenologies, including gait instability, chorea, bradykinesia, dystonia, tremor, myoclonus, hyperekplexia, and cramps/fasciculations [50, 51].
In these patients, a combination of bulbar, respiratory, and autonomic involvement may explain why many of the initially reported cases died suddenly and unexpectedly, and progressed to autopsy. These patients were initially felt not to respond to immunotherapy [48], consistent with a dominant neurodegenerative disorder. However, more optimistically, later series, the largest of which contained 53 patients, have demonstrated that 75% of treated patients show some response to immunotherapies, including first- and second-line agents [50, 52]. Our clinical experience has been of temporary unequivocal partial improvement or stabilization with the first-line immunotherapies, which is then followed by occasional stabilization but, more commonly, subsequent deteriorations, which can be very challenging to manage. Hence, in this condition, it remains to be observed whether suppression of the probable immunological effector limb is sufficient to halt, or even reverse, the longer-term disease process.
Myelin oligodendrocyte protein (MOG)
MOG antibody-associated disorder (MOGAD) was originally identified as a CNS demyelinating disorder in patients with neuromyelitis optica (NMO) without aquaporin-4 (AQP4) antibodies [53, 54]. Typical patients were reported to have either optic neuritis or myelitis or a combination, including a near-synchronous onset of both. More recently, around 50% of cases with acute disseminated encephalomyelitis (ADEM) have been shown to have MOG-antibodies, and these antibodies are also detected in patients who have cortical encephalitis with leptomeningeal inflammation [55,56,57,58]. Patients with cortical encephalitis secondary to MOGAD most often present with seizures, which often have a focal unilateral limb onset before becoming generalized, as well as headache, fever, and occasional signs of cerebral irritation, such as confusion, lethargy, and memory impairment [56, 57, 59].
In MOGAD cortical encephalitis, MRI reveal focal cortical FLAIR hyperintensities with some associated sulcal FLAIR hyperintensity and meningeal enhancement. CSF pleocytosis is seen in most patients with this syndrome, often without oligoclonal bands or other biochemical signs of inflammation [56, 57, 59]. The histopathology of MOGAD cortical encephalitis demonstrates subpial lesions with perivenous demyelination, which are also seen in cases of acute disseminated encephalomyelitiss [59, 60], as well as microglial reactivity and inflammatory infiltrates in the meninges or around blood vessels [59]. The syndrome often responds highly effectively to corticosteroids with or without other first-line immunotherapies. Yet, relapses are seen in up to 40% of cases, leaving unanswered questions about whether repeat corticosteroid courses, steroid-sparing agents, or rituximab should be considered more routinely in management of the first episode.
GFAP
GFAP-antibodies have recently been described in a group of immunotherapy-responsive syndromes, often with meningoencephalomyelitis as the classical, overarching manifestation [61]. In the largest series to date (n = 102) [62], a viral prodrome was seen in the majority, 94% had either meningitis, encephalitis or myelitis, around 30% had concurrent AQP4- or NMDAR-antibodies, and around 30% had an underlying neoplasia. GFAP-antibody testing in the CSF is key to establishing the disease diagnosis and, as GFAP is an intracellular protein, these antibodies are likely biomarkers of an underlying process rather than being directly pathogenic [63].
As a diagnostic aide, MRI imaging is almost always abnormal in this condition [62, 64]. Characteristic brain contrast enhancement identified a linear, radial perivascular pattern through the periventricular white matter, though there can also be leptomeningeal enhancement. In the spinal cord, there is often longitudinally extensive myelitis with central enhancement. In addition, contrast enhancement is observed in around two-thirds of cases. CSF constituents are abnormal in the majority, with a lymphocyte pleocytosis (mean cell count 80 /ul), raised protein, and oligoclonal bands present in ~ 50% of cases. EEG can be abnormal with generalized slowing. Patients respond variably to treatment, but 73% with a meningoencephalomyelitis were shown to respond to the first-line immunotherapies, while the second-line agents were needed in refractory or relapsing cases, which should also prompt a more detailed search for neoplasms [62,63,64]. One key question is whether the frequent coexistence of GFAP-antibodies with antibodies of other reactivities suggests that GFAP-antibodies are an epiphenomenon generated as part of epitope spread or are an indication of pathogenic GFAP-directed T-cell immunity.
KLH-11
Antibodies to KLHL-11 were described in 2019 in a small series of patients with testicular seminoma and a rhomboencephalitis lacking the Ma-2 antibodies classically expected in this context [65]. Interestingly, the neurological syndrome preceded the seminoma diagnosis in 9 of 13 patients (69%). A larger retrospective series showed this antibody only in men, presenting with a rhomboencephalitis: 83% were associated with evidence of a testicular germ cell tumors (including radiological spontaneous regression) and there was suggestion of an over-representation of HLA-DQB1*02:01 and HLA-DRB1*03:01 alleles [66]. A 58% response to immunotherapy ± cancer treatment indicated that autoantibodies to this intracellular antigen may show treatment responses.
In contrast, a different cohort study reported an equal sex distribution but a similar association with tumors (72%), which were predominantly benign teratomas of the testis but also seminomas or mixed germ cell tumors. Clinically, 41% had an ataxic or brainstem predominant syndrome and this subgroup was enriched for a tumor association (85%) [67].
In summary, this novel antibody should be tested in patients, especially men, presenting with brainstem symptoms or ataxia and, if positive, should trigger a high suspicion for a tumor as well as a trial of immunotherapy. Further work is required to understand fully the immunobiology of KLHL-11 encephalitis.
Advances in the underlying immunobiology
Since their original clinical descriptions, our understanding of the immunobiology of the diseases summarized in the previous section has advanced considerably [68]. Selected highlights are provided below and summarized in Fig. 2.
Immunological Aspects. A The generation of antigen-specific T cells involves antigen presentation by professional antigen-presenting cells (APC) including dendritic cells, macrophages, and B cells. The APC take up antigens and process them into MHC II-antigen complexes, which are displayed on the cell surface. At the “immunological synapse” between APC and T cell, classically three signals are exchanged: The first signal is the T-cell receptor (TCR)–MHCII complex interaction; the second signal is transmitted via other surface proteins (e.g., CD80/86 and CD28) and the third include soluble factors (e.g., various cytokines), which help polarize T-cell subtypes. Adapted from Roche et al. [69] and Sharabi et al. [70]. B T and B cells interact tightly to generate soluble autoantibodies. Cognate T-cell encounters enable B cells to mature into IgM producing, short-lived plasma cells (SLPC), often bypassing germinal centres (GC). The GC response results in higher affinity antibodies and immunological memory. Activated B cells undergo clonal expansion and somatic hypermutation, and the latter matures and improves the strength of the B cell for its antigen. The resulting memory B cells and plasmablasts exit the GC and home to their survival niches as long-lived plasma cells (LLPC). Adapted from Sun et al. [68] and Zografou et al. [71] and Stebegg et al. [72]
In the periphery
Two key goals in all autoantibody-mediated diseases are to accurately describe the immunological compartments where self-targeted B-cell receptors (BCRs; the B-cell surface bound antibody) are generated and escape mechanisms of immune tolerence, and to understand mechanisms by which the autoantibody response is propagated. Both show clear relevance to the selection of therapeutics and are often modeled by two broad immunological schemata [73, 74]. The first suggests that, throughout disease, ongoing germinal center reactions generate autoantigen-reactive B and antibody-secreting cells. The other, somewhat opposing, model is of a remote breakdown in tolerance which, via a brief germinal center reaction, produces long-lived plasma cells (LLPC), which likely reside in bone marrow or CNS niches. This second model is thought to be how lifelong immunity is acquired from childhood vaccinations and, from a therapeutic perspective, is important as LLPCs are non-proliferative and do not express CD20. Therefore, these cells are theoretically insensitive to drugs, such as azathioprine, mycophenolate mofetil, or rituximab. By studying peripheral blood mononuclear cells (PBMCs) from patients with NMDAR-AbE, Makuch et al. [75] were able to demonstrate that patient circulating B cells frequently generate NMDAR-reactive antibodies, at levels proportional to the corresponding patient’s serum NMDAR-antibody titres. This suggested an ongoing immunological process, and argued against predominantly LLPC-driven mechanisms. Similarly, NMDAR-reactive IgMs were found in the patient sera at many timepoints during the course of the disease, again supporting evidence of ongoing, active immune reactions. In addition, the key tumor association in this condition, an ovarian teratoma, pointed more directly toward the presence of active germinal centers. Teratoma tissue contained dense clusters of B and T cells, with the NR1 (‘immunodominant’) autoantigen in close apposition to follicular dendritic cells, lymphatic structures, and high endothelial vasculature [76]. These observations were consistent with the presence of an intratumoral tertiary lymphoid structure, with germinal center-like capacity. Furthermore, in culture, it has been shown that these lymphocytes had the capacity to produce NMDAR-specific antibodies. This provided evidence of an active, NMDAR-focused, tumor-based germinal center reaction in NMDAR-AbE.
However, only around 30% of patients with NMDAR-AbE have ovarian teratomas. Hence, the search for germinal centers was extended with a pioneering approach to directly sample lymphocytes from patient cervical lymph nodes [76], which represent the likely anatomical site of CNS lymphatic drainage [77]. Culture of these lymphocytes was found to produce NMDAR-IgG, particularly in patients with higher serum NMDAR-antibody levels and the highest levels of the germinal center marker CXCL13 [76]. Taken together, both patient cervical lymph nodes and ovarian teratomas provide evidence of active NMDAR-antibody generating germinal center reactions.
In a related disease, neuromyelitis optica spectrum disorders (NMOSD) associated with aquaporin-4 antibodies, there is evidence to suggest that patients may have an intrinsic predisposition to the entry of autoantigen-reactive B cells into germinal centers. Naïve B cells (which are not thought to enter germinal centers) from patients but not healthy controls were found to carry AQP4-reactivities. This finding suggests that naïve B cells, newly emerging from the bone marrow, may contribute a proportion of the ongoing immune response in patients [78]. It remains to be ascertained whether this can be confirmed in future studies and whether this principle translates to autoimmune encephalitis.
Germinal centers are noted for their ability to imprint BCRs with somatic hypermutations, which classically both increase antibody affinities and generate diverse epitopes. Indeed, peripheral autoantigen-reactive B cells in patients with LGI1-antibody encephalitis identified heterogenous and abundant patterns of hypermutation, targeting of multiple epitopes within the two major domains of LGI1, and found that some LGI1-reactive monoclonal antibodies with high affinity BCRs were able to cause pathology when injected into mice [79]. Again, and taken together with the fundamental observation that these LGI1-reactive memory B cells were detected in the periphery, these findings all support a role for germinal centers in producing these autoreactive B cells.
The evaluation of a biological role for germinal centers is made even more clinically relevant by a recent therapeutic observation. While several studies had suggested that lymph nodes are often resistant to rituximab, an immunotherapeutic agent directed against CD20 [80, 81], a study of fine-needle aspirations in humans identified marked sensitivity of cervical lymph -node B cells to rituximab, with a lymph-node specific reduction in autoantibody levels [82].
Germinal centers involve direct interactions of B and T cells and, in diseases whose core feature is autoantibody production, CD4 T cells are particularly implicated as key helpers of—cell activation, division, and differentiation. Class II HLA molecules are involved in presenting peptide antigens to CD4 + helper T cells. Hence, it appears biologically intuitive that strong class II HLA association have been identified in some autoantibody-mediated diseases, especially in patients with antibodies to LGI1, CASPR2, and IgLON5 [83,84,85]. The HLA-DRB1*07:01 gene is carried by ~ 95% of patients with LGI1-antibodies, and homozygosity is associated with a doubling of risk, a dose–response suggesting causality [86]. Around 50% of patients with CASPR2-antibodies carry a specific HLA allele, DRB1*11:01, which increases to ~ 90% in patients with CASPR2-antibodies in the context of limbic encephalitis. In addition, ~ 90% of patients with IgLON5-antibodies carry both HLA-DRB1*10:01 and HLA-DQB1*05:01 alleles. These collective genetic findings indicate that individual antigens bind to specific HLA alleles which are a crucial step in the development of their respective autoantibody-mediated conditions. These HLA associations are also in keeping with in vitro data, which suggested that conditions mimicking T-cell help were most likely to lead to specific antibody production [75, 78].
However, most autoantibody-mediated diseases lack strong HLA associations and so these genetic links do not appear necessary for generation of all autoantibodies, suggesting that alternative immunological mechanisms await discovery.
In the CNS
If and how the peripheral immune response migrates to the CNS is another intriguing, and therapeutically relevant, question. The log-fold higher absolute levels of autoantibodies in serum versus the CSF might suggest that the autoantibody generation begins in the periphery. However, when normalized for total IgG levels in each compartment, intrathecal synthesis is often apparent: this is a biochemical measure which suggests the presence of autoantigen-reactive B cells in the CSF.
One study, elegantly proving this concept, cloned and expressed individual BCRs from the CSF memory and antibody-secreting B cells in patients with NMDAR-AbE [87]. Around 10% of BCRs were found to react to NMDARs and their mutational patterns showed both immunoglobulin class switching and somatic hypermutation, suggesting that these B cells had undergone affinity maturation within a germinal center. However, intriguingly, a minority were non-mutated and essentially germline encoded, perhaps indicating a more fundamental genetic predisposition to this rare illness. The same group studied CSF B cells in patients with LGI1- and GABAAR-antibody encephalitis [88], and found a high frequency of highly mutated autoantigen-reactive BCRs in both conditions [89]. While these collective studies have identified abundant intrathecal autoantigen-reactive B cells, the directionality of these cells is unknown. Yet, BCRs expanded in CSF clones do appear to be found within the BCR repertoire of peripheral B cells, suggesting a dynamic exchange between B cells in these two compartments [90]. Cross-sectional study designs in further subjects, especially when untreated, could aim to address these questions in the future.
Advances in the underlying neurobiology
Alongside advances in our understanding around the immunological mechanisms which give rise to these pathogenic antibodies, advances have also been made in how these antibodies mediate their effects to cause such clinically characteristic phenotypes (Fig. 3).
Advances in neurobiology. A In NMDAR-antibody encephalitis. Under physiological conditions, NMDARs are organized in post-synaptic clusters and stabilized by ephrin B2 (EphB2). Autoantibodies in NMDAR-antibody encephalitis disrupt the interaction between NMDARs and EphB2, causing a lateral dispersion of the receptors (left panel). They also cross-link NMDARs causing their internalization through endocytosis (right panel). Adapted from Ladépêche et al. [91]. B In LGI1- and CASPR2-antibody diseases. Patient symptoms are likely caused by modulation of AMPARs and VGKCs. LGI1-antibodies disrupt binding of LGI1 to ADAM22/23, which reduces post-synaptic AMPA receptors, thus resulting in hyperexcitability. In CASPR2-antibody encephalitis, patient antibodies potentially disrupt the VGKC–contactin–CASPR2 complex, leading to altered excitability. Adapted from Van Sonderen et al. [92]
In NMDAR-AbE, antibodies are reported to bind the extracellular amino-terminal domain of the NR1 subunit. Patient serum and CSF have been shown in vitro to reduce the size of NMDAR clusters giving rise to impaired glutamatergic signaling. This effect is reversible and resolves on removal of the NMDAR-antibodies [87, 93]. The reduction of NMDAR cluster density is likely driven by two phenomena: internalization of NMDARs and their lateral dispersion from key synaptic signaling areas. Internalisation occurs secondary to antibody-mediated endocytosis, due to cross linking of NMDARs. Lateral dispersion may be driven by disruption of the interaction between NMDARs and Ephrin-B2, a receptor tyrosine kinase which binds and phosphorylates NMDARs [94, 95]. Infusion of Ephrin-B2 into animal models of NMDAR-AbE antagonises this effect, with rescue of the clinical phenotype and preservation of NMDAR cluster density [96].
In LGI1- and CASPR2-antibody encephalitis, there is an evolving neuroscientific understanding of the role of AMPA receptors in disease manifestations. Murine mutation of LGI1 impairs AMPAR signaling, likely via disruption of the presynaptic Kv1.1 potassium channels ADAM23 and post-synaptic ADAM22-AMPA receptor complexes [97]. In vitro and in vivo data demonstrated that LGI1-antibodies disrupt the binding of LGI1 to ADAM22/23, leading to a reduction of post-synaptic AMPA receptors with consequent excess network excitability and seizures [98]. More recent work has shown patient-derived LGI1-directed monoclonal antibodies target different domains of LGI1 and can disrupt binding of LGI1 to ADAM22/23 differentially, with resultant impaired long-term potentiation in animal models [79]. In CASPR2-antibody encephalitis, evidence from animal models suggests that similar mechanisms are in operation, with silencing of CASPR2 either genetically or with autoantibodies resulting in altered AMPA receptor function and subsequent disruption of cortical excitatory transmission [99].
Advances in management
The management of patients with autoimmune encephalitis is an area informed by expert observations, retrospective observational studies and only one randomized controlled trial. This paucity of classically perceived ‘high quality’ evidence is driven mostly by the relatively scarcity of these conditions and the appropriate onus on early treatment, meaning that studies of interventions are necessarily contaminated by administration of prior immunotherapies. Nevertheless, studies examining treatment interventions and patient outcomes have made considerable progress over the last few years.
Patient outcomes
Understanding longer term issues which patients encounter continues to be an area of active research with important everyday implications. For example, in NMDAR-AbE, it is widely accepted that treatments are generally highly effective. However, detailed neuropsychological assessments at long-term follow-up have demonstrated that ~ 80% of patients had moderate-to-severe cognitive impairment, with prominent deficits in executive function and memory. This challenges the current perception of this disease as showing a complete response to immunotherapy. Furthermore, poor cognitive outcomes were correlated with late treatments, more severe disease and longer duration of acute illness; making the case again for earlier recognition and aggressive treatment [100]. In pediatric NMDAR-AbE [101], attention and fatigue represent key persistent deficits which correlate with quality of life, suggesting that a younger and more neuroplastic brain is insufficient to protect against this disease effect. Similar observations were made in patients with LGI1-antibody encephalitis [102]. Despite good outcomes based on the widely employed modified Rankin Scale, around 80% of patients showed deficits in cognition, mood or fatigue, with only 15% able to return to work. Even the more disease-specific score, Clinical Assessment Scale in Autoimmune Encephalitis (CASE), only revealed a limited quantitative improvement in the patients, perhaps as this scale may be especially valuable in patients with NMDAR-antibody encephalitis over other forms of autoimmune encephalitis [103]. Taken together, these studies suggest that we should collectively consider these to be partially immunotherapy-responsive conditions in which our management currently remains far from ideal. In future studies, more needs to be done to optimize these long-term outcomes for this patient group.
Monitoring disease
Perhaps surprisingly for diseases conceptualized to have autoantibodies as the main pathological effectors, autoantibody levels are only imperfectly correlated with disease severity, both between and within patients [104, 105]. Therefore, the question arises: how do we accurately monitor patients? Improved monitoring would yield two clear benefits. First, the ability to predict a recrudescence in disease activity, which could be pre-emptively treated. Second, to help provide a rationale for escalating immunotherapies in view of the ongoing disability demonstrated in the above studies. There are several emerging candidates.
Some of these candidates are immunological in nature. For example, in NMOSD, there was a switch of IgG subclasses and increased production of AQP4-specific IgMs around the time of relapses, implying that these features are consistent with new germinal center activity associated with relapses [82]. Also, CXCL13, a chemoattractant reported to mediate recruitment to and retention of B cells within the CSF, has been associated with a limited response to therapy, more clinical relapses and as a biological correlate of intrathecal NMDAR-antibody synthesis [106].
Others reflect damage to the cells targeted by the autoantibodies. In NMOSD, glial fibrillary acidic protein (GFAP) is an emerging biomarker. GFAP is a cytoskeletal protein specifically expressed in astrocytes, which are the cellular targets of pathogenic AQP4 antibodies. Serum GFAP levels are elevated in NMOSD versus healthy controls and other demyelinating diseases and, within patients, elevated GFAP correlates with relapses, relapse severity, and disease severity, and may predict the propensity to relapse at disease onset [107,108,109]. Furthermore, there is emerging evidence that neurofilament-light chain measurement in CSF is modestly elevated at presentation in LGI1-, CASPR2-, and NMDAR-AbE, but its prospective predictive value remains unproven [110, 111].
Finally, a recent study in five patients highlighted that direct assessments of the target autoantigen may represent a promising approach. Using a PET ligand which targets activated NMDARs, it was observed that patients recovering from NMDAR-AbE showed a reduction in NMDAR density which correlated with time from disease onset. One patient, who was both furthest into their recovery and had no detectable NMDAR-antibodies, had NMDAR densities equivalent to controls [112]. Hence, imaging tools might be useful to monitor in vivo recovery and could inform longer term treatment decisions.
These are all potentially exciting tools. However, currently, none offer well-validated prospective clinical predictive values, and we continue to rely on clinical judgment to direct patient follow-up.
Immunotherapy
Corticosteroids
Cortisol is the endogenous corticosteroid, produced from cholesterol in the adrenal gland, and acts predominantly on glucocorticoid receptors. Synthetic corticosteroids, including prednisolone, methylprednisolone, and dexamethasone, are selected based on a high glucocorticoid preference. The exact mechanisms by which corticosteroids treat autoimmune CNS conditions is unclear but likely to rely on a combination of their pleotropic abilities to decrease blood–brain barrier permeability [113], rapidly suppress (within minutes) transcription of genes encoding pro-inflammatory cytokines, chemokines and cell adhesion molecules [114], repression of key immunomodulatory transcription factors (e.g., NF-κB and AP-1) [115], suppression of myeloid cell function, and induction of apoptosis in lymphocytes [116]. Due to their clear benefits on cognition and seizure frequency in observational studies, corticosteroids are the most frequently employed the first-line treatment for patients [4, 17]. Corticosteroid dosing and weaning regimes vary hugely between physicians treating these conditions and, in our experience, depends on the autoantibody underlying the disorder. For example, in NMDAR-AbE, we have been successful in corticosteroid induction without tapering, but in LGI1-AbE, we have observed that this approach precipitates relapses, often necessitating prolonged courses of corticosteroids in this condition. Unfortunately, corticosteroid side effects are myriad and include insomnia, diabetes mellitus, hypertension, osteopenia, avascular necrosis, muscle atrophy, and psychiatric disorders. Many of these side effects are related to duration of treatment and dose, and particularly affect the more elderly patients, the main group affected by LGI1-antibody encephalitis.
The choice of corticosteroid is also not closely scrutinized in studies, with prednisolone and methylprednisolone empirically reached for on a neurological ward. However, evidence exists that dexamethasone remains at a higher concentration in the CNS for a longer duration [117], as well as having higher glucocorticoid efficacy and less mineralocorticoid activity. Hence, an ongoing challenge is to establish optimum steroid treatment regimens and mitigate many of these common adverse effects.
PLEX, IVIG, and Immunoadsorption
PLEX and IVIG are well-established treatments in autoimmune encephalitis and are often used as first-line immunotherapies [4, 118]. There is some evidence that the addition of PLEX to corticosteroids and IVIG offers superior efficacy [119]. Often, there are logistical factors which inform the use of either IVIG or PLEX, including the scarcity of human immunoglobulins, unwillingness from some patients to accept human blood products, access to PLEX, patient ability to tolerate PLEX, including vascular access issues. Nevertheless, IVIG is the only treatment for autoimmune encephalitis with proven efficacy in a randomized controlled trial [120]. Yet, the effect size was small in absolute terms and only just reached significance by comparison to placebo. In our clinical practice, IVIG is very rarely used, as PLEX appears both to generate striking and rapid improvements in many patients and can be performed through peripheral cannulation, making it both efficacious and de-risking it significantly.
As an alternative to PLEX, immunoadsorption was able to clear autoantibodies from both the serum (97%) and CSF (64%) within 4 days and sustained reductions in autoantibody levels seen at 4 weeks, and was associated with improvement in 86% of patients with NSAbs [121]. Furthermore, immunoadsorption offers the opportunity to spare patients exposure to transfusion products when compared with plasma exchange.
Steroid sparing agents
The use of agents, such as methotrexate, azathioprine, and mycophenolate mofetil, is influenced by a variety of factors. For example, patients with NMDAR-AbE are often treated with pulsed corticosteroids and PLEX, with a low threshold to escalate to second-line agents, such as rituximab or cyclophosphamide. First- plus second-line therapies can induce prolonged remission in as many as ~ 95% of cases, leaving little role for the use of steroid-sparing agents. Reported relapse rates are higher in patients with LGI1- and CASPR2-antibody-mediated diseases, particularly if corticosteroids are tapered too quickly. Hence, steroid-sparing agents are employed more often in this context. However, in our experience, relapses remain most strongly related to a shorter taper of steroids despite the use of steroid-sparing agents [10].
Monoclonal antibodies
As mentioned previously, the chimeric monoclonal antibody directed against the B-cell marker CD20, rituximab, is widely used in autoimmune encephalitis, most commonly at the earliest time points in NMDAR-AbE [122], but also later in the disease course of patients with autoantibodies against LGI1, CASPR2, and GAD. In the largest retrospective cohort study to date, patients with CASPR2-antibody diseases and NMDAR-AbE showed improvements with rituximab, whereas patients with LGI1-antibodies improved similarly with administration of other immunotherapies [122]. Relapse rate was 13% in controls and 5% in cases following rituximab treatment in a pooled analysis of 228 patients with antibodies to NMDAR, CASPR2 and LGI1. Improved treatment efficacy was observed with its early administration [122]. The overall perceived efficacy of rituximab may suggest a limited role for LLPCs in disease propagation. A clinical trial of Ocrelizumab, a humanized anti-CD20, in autoimmune encephalitis failed to meet target enrollment and was discontinued. Recently, inebilizumab, a CD19-targeted monoclonal antibody, has received FDA approval in NMOSD based on a randomized controlled trial of 230 participants [123]. An infection signature in patients with prior rituximab use was noted following treatment with inebilizumab: 18% serious infection vs 10% with no prior rituximab use (though not statistically significant), and so, further evaluation in this setting is ongoing [124]. This drug is being trialed in NMDAR-AbE based on the biological rationale that CD19 is expressed on more B-lineage cells than CD20, both earlier and later in developmental stages.
Novel immunotherapies
Given the significant side effect profile of steroids, the lack of a clear role for steroid-sparing agents and our growing knowledge of the underlying immunology of these conditions, it is fortunate that new and more targeted treatments are on the horizon. IL-6 receptor monoclonal antibodies have been used in autoimmune encephalitis refractory to rituximab with encouraging observational results [125]. A humanized IL-6 monoclonal, already approved for use in NMOSD, is currently being assessed in a clinical trial of patients with autoimmune encephalitis secondary to NMDAR- and LGI1-antibodies (https://clinicaltrials.gov/ct2/show/NCT05503264). Bortezomib is a proteasome inhibitor. As the proteosome is most active in antibody-secreting plasma cells, which express very little CD20, it is being trialed in refractory cases of autoimmune encephalitis, where both first- and second-line treatments have failed (https://clinicaltrials.gov/ct2/show/NCT03993262). Finally, monoclonal antibodies directed against the neonatal Fc receptor, FcRN, are being trialed in these conditions. The FcRN constitutively recycle IgG to preserve its half-life. Hence, their blockade markedly reduces antibody levels. These drugs have shown benefits in myasthenia gravis and are currently being trialed in LGI1-antibody encephalitis (https://clinicaltrials.gov/ct2/show/NCT04875975).
Conclusions
Since 2015, the field of autoimmune encephalitis has witnessed a number of advances in our understanding of the underlying biology and the correlation of this with more refined clinical observations. Our hope is that by the time of our next review, the use of early, targeted immunotherapies is commonplace in these conditions and has had an appreciable impact on the long-term outcomes of patients. To integrate the emerging biological insights with our progress around patient-relevant outcomes and the limitations of currently available therapies, the field now needs to embrace experimental medicine approaches. Some classical clinical trials are underway but may be hampered by difficulty recruiting immunotherapy-naïve patients. Nevertheless, a large pipeline of exciting new treatments will likely enter clinical trials in the near future. If incorporated with further dissection of the underlying biology, these trials are likely to provide a foundation for patient treatments over the next decade.
Data availability
No new data were generated in this manuscript.
References
Varley J, Vincent A, Irani SR (2015) Clinical and experimental studies of potentially pathogenic brain-directed autoantibodies: current knowledge and future directions. J Neurol 262:1081–1095
Leypoldt F, Wandinger KP (2014) Paraneoplastic neurological syndromes. Clin Exp Immunol 175:336–348
McKeon A, Pittock SJ (2011) Paraneoplastic encephalomyelopathies: pathology and mechanisms. Acta Neuropathol 122:381–400
Thompson J, Bi M, Murchison AG et al (2018) The importance of early immunotherapy in patients with faciobrachial dystonic seizures. Brain 141:348–356
Titulaer MJ, McCracken L, Gabilondo I et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165
Aurangzeb S, Symmonds M, Knight RK, Kennett R, Wehner T, Irani SR (2017) LGI1-antibody encephalitis is characterised by frequent, multifocal clinical and subclinical seizures. Seizure 50:14–17
Jacob S, Irani SR, Rajabally YA et al (2008) Hypothermia in VGKC antibody-associated limbic encephalitis. J Neurol Neurosurg Psychiatry 79:202–204
Rocamora R, Becerra JL, Fossas P et al (2014) Pilomotor seizures: an autonomic semiology of limbic encephalitis? Seizure 23:670–673
van Sonderen A, Thijs RD, Coenders EC et al (2016) Anti-LGI1 encephalitis: clinical syndrome and long-term follow-up. Neurology 87:1449–1456
Irani SR, Stagg CJ, Schott JM et al (2013) Faciobrachial dystonic seizures: the influence of immunotherapy on seizure control and prevention of cognitive impairment in a broadening phenotype. Brain 136:3151–3162
Irani SR, Michell AW, Lang B et al (2011) Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol 69:892–900
Irani SR, Alexander S, Waters P et al (2010) Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan’s syndrome and acquired neuromyotonia. Brain 133:2734–2748
Lai M, Huijbers MG, Lancaster E et al (2010) Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. The Lancet Neurology 9:776–785
Malter MP, Frisch C, Schoene-Bake JC et al (2014) Outcome of limbic encephalitis with VGKC-complex antibodies: relation to antigenic specificity. J Neurol 261:1695–1705
Butler CR, Miller TD, Kaur MS et al (2014) Persistent anterograde amnesia following limbic encephalitis associated with antibodies to the voltage-gated potassium channel complex. J Neurol Neurosurg Psychiatry 85:387–391
Bettcher BM, Gelfand JM, Irani SR et al (2014) More than memory impairment in voltage-gated potassium channel complex encephalopathy. Eur J Neurol 21:1301–1310
Rodriguez A, Klein CJ, Sechi E et al (2022) LGI1 antibody encephalitis: acute treatment comparisons and outcome. J Neurol Neurosurg Psychiatry 93:309–315
Shillito P, Molenaar PC, Vincent A et al (1995) Acquired neuromyotonia: evidence for autoantibodies directed against K+ channels of peripheral nerves. Ann Neurol 38:714–722
Irani SR, Pettingill P, Kleopa KA et al (2012) Morvan syndrome: clinical and serological observations in 29 cases. Ann Neurol 72:241–255
Gadoth A, Pittock SJ, Dubey D et al (2017) Expanded phenotypes and outcomes among 256 LGI1/CASPR2-IgG-positive patients. Ann Neurol 82:79–92
van Sonderen A, Arino H, Petit-Pedrol M et al (2016) The clinical spectrum of Caspr2 antibody-associated disease. Neurology 87:521–528
Klein CJ, Lennon VA, Aston PA et al (2013) Insights from LGI1 and CASPR2 potassium channel complex autoantibody subtyping. JAMA Neurol 70:229–234
Lancaster E, Huijbers MG, Bar V et al (2011) Investigations of caspr2, an autoantigen of encephalitis and neuromyotonia. Ann Neurol 69:303–311
Govert F, Abrante L, Becktepe J et al (2022) Distinct movement disorders in contactin-associated-protein-like-2 antibody associated autoimmune encephalitis. Brain 146(2):657–667
Damato V, Balint B, Kienzler AK, Irani SR (2018) The clinical features, underlying immunology, and treatment of autoantibody-mediated movement disorders. Movement Disord 33:1376–1389
Garrido Sanabria ER, Zahid A, Britton J et al (2022) CASPR2-IgG-associated autoimmune seizures. Epilepsia 63:709–722
Ramanathan S, Tseng M, Davies AJ et al (2021) Leucine-rich glioma-inactivated 1 versus Contactin-associated protein-like 2 antibody neuropathic pain: clinical and biological comparisons. Ann Neurol 90:683–690
Vincent A, Pettingill P, Pettingill R et al (2018) Association of leucine-rich glioma inactivated protein 1, Contactin-associated protein 2, and Contactin 2 antibodies with clinical features and patient-reported pain in acquired neuromyotonia. JAMA Neurol 75:1519–1527
Kleinig TJ, Thompson PD, Matar W et al (2008) The distinctive movement disorder of ovarian teratoma-associated encephalitis. Movement Disord 23:1256–1261
Irani SR, Bera K, Waters P et al (2010) N-methyl-d-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133:1655–1667
Varley JA, Webb AJS, Balint B et al (2018) The Movement disorder associated with NMDAR antibody-encephalitis is complex and characteristic: an expert video-rating study. J Neurol Neurosurg Psychiatry 90(6):724–726
Mohammad SS, Fung VS, Grattan-Smith P et al (2014) Movement disorders in children with anti-NMDAR encephalitis and other autoimmune encephalopathies. Movement Disord 29:1539–1542
Dalmau J, Gleichman AJ, Hughes EG et al (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098
Al-Diwani A, Handel A, Townsend L et al (2019) The psychopathology of NMDAR-antibody encephalitis in adults: a systematic review and phenotypic analysis of individual patient data. Lancet Psychiatry 6:235–246
Moghaddam B, Javitt D (2012) From revolution to evolution: the glutamate hypothesis of schizophrenia and its implication for treatment. Neuropsychopharmacology 37:4–15
Pathmanandavel K, Starling J, Merheb V et al (2015) Antibodies to surface dopamine-2 receptor and N-methyl-d-aspartate receptor in the first episode of acute psychosis in children. Biol Psychiat 77:537–547
Zandi MS, Irani SR, Lang B et al (2011) Disease-relevant autoantibodies in first episode schizophrenia. J Neurol 258:686–688
Lennox BR, Palmer-Cooper EC, Pollak T et al (2017) Prevalence and clinical characteristics of serum neuronal cell surface antibodies in first-episode psychosis: a case-control study. Lancet Psychiatry 4:42–48
Dahm L, Ott C, Steiner J et al (2014) Seroprevalence of autoantibodies against brain antigens in health and disease. Ann Neurol 76:82–94
Steiner J, Teegen B, Schiltz K, Bernstein HG, Stoecker W, Bogerts B (2014) Prevalence of N-methyl-d-aspartate receptor autoantibodies in the peripheral blood: healthy control samples revisited. JAMA Psychiat 71:838–839
Oviedo-Salcedo T, de Witte L, Kumpfel T et al (2018) Absence of cerebrospinal fluid antineuronal antibodies in schizophrenia spectrum disorders. Br J Psychiatry 212:318–320
Guasp M, Gine-Serven E, Maudes E et al (2021) Clinical, neuroimmunologic, and CSF investigations in first episode psychosis. Neurology 97:e61–e75
Theorell J, Ramberger M, Harrison R et al (2021) Screening for pathogenic neuronal autoantibodies in serum and CSF of patients with first-episode psychosis. Transl Psychiatry 11:566
Pettingill P, Kramer HB, Coebergh JA et al (2015) Antibodies to GABAA receptor α1 and γ2 subunits: clinical and serologic characterization. Neurology 84:1233–1241
Petit-Pedrol M, Armangue T, Peng X et al (2014) Encephalitis with refractory seizures, status epilepticus, and antibodies to the GABAA receptor: a case series, characterisation of the antigen, and analysis of the effects of antibodies. Lancet Neurol 13:276–286
Spatola M, Petit-Pedrol M, Simabukuro MM et al (2017) Investigations in GABA(A) receptor antibody-associated encephalitis. Neurology 88:1012–1020
Deng B, Cai M, Qiu Y et al (2022) MRI characteristics of autoimmune encephalitis with autoantibodies to GABAA receptor: a case series. Neurol (R) Neuroimmunol Neuroinflamm 9:e1158
Sabater L, Gaig C, Gelpi E et al (2014) A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol 13:575–586
Gaig C, Graus F, Compta Y et al (2017) Clinical manifestations of the anti-IgLON5 disease. Neurology 88:1736–1743
Honorat JA, Komorowski L, Josephs KA et al (2017) IgLON5 antibody: neurological accompaniments and outcomes in 20 patients. Neurol (R) Neuroimmunol Neuroinflamm 4:e385
Gaig C, Compta Y, Heidbreder A et al (2021) Frequency and characterization of movement disorders in anti-IgLON5 disease. Neurology 97:e1367–e1381
Gruter T, Mollers FE, Tietz A et al (2023) Clinical, serological and genetic predictors of response to immunotherapy in anti-IgLON5 disease. Brain 146:600–611
Reindl M, Waters P (2019) Myelin oligodendrocyte glycoprotein antibodies in neurological disease. Nat Rev Neurol 15:89–102
O’Connor KC, McLaughlin KA, De Jager PL et al (2007) Self-antigen tetramers discriminate between myelin autoantibodies to native or denatured protein. Nat Med 13:211–217
Fujimori J, Takai Y, Nakashima I et al (2017) Bilateral frontal cortex encephalitis and paraparesis in a patient with anti-MOG antibodies. J Neurol Neurosurg Psychiatry 88:534–536
Ogawa R, Nakashima I, Takahashi T et al (2017) MOG antibody-positive, benign, unilateral, cerebral cortical encephalitis with epilepsy. Neurol (R) Neuroimmunol Neuroinflamm 4:e322
Budhram A, Mirian A, Le C, Hosseini-Moghaddam SM, Sharma M, Nicolle MW (2019) Unilateral cortical FLAIR-hyperintense lesions in anti-MOG-associated Encephalitis with Seizures (FLAMES): characterization of a distinct clinico-radiographic syndrome. J Neurol 266:2481–2487
Banwell B, Bennett JL, Marignier R et al (2023) Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: international MOGAD panel proposed criteria. Lancet Neurol 22:268–282
Valencia-Sanchez C, Guo Y, Krecke KN et al (2022) Cerebral cortical encephalitis in MOGAD. Ann Neurol 93:297–302
Takai Y, Misu T, Kaneko K et al (2020) Myelin oligodendrocyte glycoprotein antibody-associated disease: an immunopathological study. Brain 143:1431–1446
Fang B, McKeon A, Hinson SR et al (2016) Autoimmune glial fibrillary acidic protein astrocytopathy: a novel meningoencephalomyelitis. JAMA Neurol 73:1297–1307
Flanagan EP, Hinson SR, Lennon VA et al (2017) Glial fibrillary acidic protein immunoglobulin G as biomarker of autoimmune astrocytopathy: analysis of 102 patients. Ann Neurol 81:298–309
Dubey D, Hinson SR, Jolliffe EA et al (2018) Autoimmune GFAP astrocytopathy: prospective evaluation of 90 patients in 1 year. J Neuroimmunol 321:157–163
Long Y, Liang J, Xu H et al (2018) Autoimmune glial fibrillary acidic protein astrocytopathy in Chinese patients: a retrospective study. Eur J Neurol 25:477–483
Mandel-Brehm C, Dubey D, Kryzer TJ et al (2019) Kelch-like protein 11 antibodies in seminoma-associated paraneoplastic encephalitis. N Engl J Med 381:47–54
Dubey D, Wilson MR, Clarkson B et al (2020) Expanded clinical phenotype, oncological associations, and immunopathologic insights of paraneoplastic Kelch-like protein-11 encephalitis. JAMA Neurol 77:1420–1429
Maudes E, Landa J, Munoz-Lopetegi A et al (2020) Clinical significance of Kelch-like protein 11 antibodies. Neurol (R) Neuroimmunol Neuroinflamm 7:e666
Sun B, Ramberger M, O’Connor KC, Bashford-Rogers RJM, Irani SR (2020) The B cell immunobiology that underlies CNS autoantibody-mediated diseases. Nat Rev Neurol 16:481–492
Roche PA, Furuta K (2015) The ins and outs of MHC class II-mediated antigen processing and presentation. Nat Rev Immunol 15:203–216
Sharabi A, Tsokos MG, Ding Y, Malek TR, Klatzmann D, Tsokos GC (2018) Regulatory T cells in the treatment of disease. Nat Rev Drug Discover 17:823–844
Zografou C, Vakrakou AG, Stathopoulos P (2021) Short- and long-lived autoantibody-secreting cells in autoimmune neurological disorders. Front Immunol 12:686466
Stebegg M, Kumar SD, Silva-Cayetano A, Fonseca VR, Linterman MA, Graca L (2018) Regulation of the germinal center response. Front Immunol 9:2469
Bernasconi NL, Traggiai E, Lanzavecchia A (2002) Maintenance of serological memory by polyclonal activation of human memory B cells. Science 298:2199–2202
Radbruch A, Muehlinghaus G, Luger EO et al (2006) Competence and competition: the challenge of becoming a long-lived plasma cell. Nat Rev Immunol 6:741–750
Makuch M, Wilson R, Al-Diwani A et al (2018) N-methyl-d-aspartate receptor antibody production from germinal center reactions: therapeutic implications. Ann Neurol 83:553–561
Al-Diwani A, Theorell J, Damato V et al (2022) Cervical lymph nodes and ovarian teratomas as germinal centres in NMDA receptor-antibody encephalitis. Brain 145:2742–2754
Da Mesquita S, Fu Z, Kipnis J (2018) The meningeal lymphatic system: a new player in neurophysiology. Neuron 100:375–388
Wilson R, Makuch M, Kienzler AK et al (2018) Condition-dependent generation of aquaporin-4 antibodies from circulating B cells in neuromyelitis optica. Brain 141:1063–1074
Ramberger M, Berretta A, Tan JMM et al (2020) Distinctive binding properties of human monoclonal LGI1 autoantibodies determine pathogenic mechanisms. Brain 143:1731–1745
Kamburova EG, Koenen HJ, Borgman KJ, ten Berge IJ, Joosten I, Hilbrands LB (2013) A single dose of rituximab does not deplete B cells in secondary lymphoid organs but alters phenotype and function. Am J Transplant 13:1503–1511
Ramwadhdoebe TH, van Baarsen LGM, Boumans MJH et al (2019) Effect of rituximab treatment on T and B cell subsets in lymph node biopsies of patients with rheumatoid arthritis. Rheumatology 58:1075–1085
Damato V, Theorell J, Al-Diwani A et al (2022) Rituximab abrogates aquaporin-4-specific germinal center activity in patients with neuromyelitis optica spectrum disorders. Proc Natl Acad Sci USA 119:e2121804119
Binks S, Varley J, Lee W et al (2018) Distinct HLA associations of LGI1 and CASPR2-antibody diseases. Brain 141:2263–2271
van Sonderen A, Roelen DL, Stoop JA et al (2016) Anti-LGI1 encephalitis is strongly associated with HLA-DR7 and HLA-DRB4. Ann Neurol 81:193–198
Kim TJ, Lee ST, Moon J, et al. (2017) Anti-LGI1 Encephalitis is Associated with Unique HLA Subtypes. Ann Neurol 81:183–192
Peris Sempere V, Muniz-Castrillo S, Ambati A et al (2022) Human Leukocyte Antigen Association Study Reveals DRB1*04:02 Effects Additional to DRB1*07:01 in Anti-LGI1 Encephalitis. Neurol (R) Neuroimmunol Neuroinflamm 9:e1140. https://doi.org/10.1212/NXI.0000000000001140
Kreye J, Wenke NK, Chayka M et al (2016) Human cerebrospinal fluid monoclonal N-methyl-d-aspartate receptor autoantibodies are sufficient for encephalitis pathogenesis. Brain 139:2641–2652
Kreye J, Wright SK, van Casteren A et al (2021) Encephalitis patient-derived monoclonal GABAA receptor antibodies cause epileptic seizures. J Exp Med 218
Kornau HC, Kreye J, Stumpf A et al (2020) Human cerebrospinal fluid monoclonal LGI1 autoantibodies increase neuronal excitability. Ann Neurol 87:405–418
Lehmann-Horn K, Irani SR, Wang S et al (2020) Intrathecal B-cell activation in LGI1 antibody encephalitis. Neurol R Neuroimmunol Neuroinflamm 7:e669
Ladépêche L, Planagumà J, Thakur S, Suárez I, Hara M, Borbely JS, Sandoval A, Laparra-Cuervo L, Dalmau J, Lakadamyali M (2018) NMDA receptor autoantibodies in autoimmune encephalitis cause a subunit-specific nanoscale redistribution of NMDA receptors. Cell Rep 23:3759–3768
Van Sonderen A, Petit-pedrol M, Dalmau J, Titulaer MJ (2017) The value of LGI1, Caspr2 and voltage-gated potassium channel antibodies in encephalitis. Nature Publishing Group, p 13
Hughes EG, Peng X, Gleichman AJ et al (2010) Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci 30:5866–5875
Mikasova L, De Rossi P, Bouchet D et al (2012) Disrupted surface cross-talk between NMDA and Ephrin-B2 receptors in anti-NMDA encephalitis. Brain 135:1606–1621
Nolt MJ, Lin Y, Hruska M et al (2011) EphB controls NMDA receptor function and synaptic targeting in a subunit-specific manner. J Neurosci 31:5353–5364
Planagumà J, Haselmann H, Mannara F et al (2016) Ephrin-B2 prevents N-methyl-d-aspartate receptor antibody effects on memory and neuroplasticity. Ann Neurol 80:388–400
Fukata Y, Lovero KL, Iwanaga T et al (2010) Disruption of LGI1-linked synaptic complex causes abnormal synaptic transmission and epilepsy. Proc Natl Acad Sci USA 107:3799–3804
Ohkawa T, Fukata Y, Yamasaki M et al (2013) Autoantibodies to epilepsy-related LGI1 in limbic encephalitis neutralize LGI1-ADAM22 interaction and reduce synaptic AMPA receptors. J Neurosci 33:18161–18174
Fernandes D, Santos SD, Coutinho E et al (2019) Disrupted AMPA receptor function upon genetic- or antibody-mediated loss of autism-associated CASPR2. Cereb Cortex 29:4919–4931
Heine J, Kopp UA, Klag J, Ploner CJ, Pruss H, Finke C (2021) Long-term cognitive outcome in anti-N-methyl-d-aspartate receptor encephalitis. Ann Neurol 90:949–961
de Bruijn M, Aarsen FK, van Oosterhout MP et al (2018) Long-term neuropsychological outcome following pediatric anti-NMDAR encephalitis. Neurology 90:e1997–e2005
Binks SNM, Veldsman M, Easton A et al (2021) Residual fatigue and cognitive deficits in patients after leucine-rich glioma-inactivated 1 antibody encephalitis. JAMA Neurol 78:617–619
Lim JA, Lee ST, Moon J et al (2019) Development of the clinical assessment scale in autoimmune encephalitis. Ann Neurol 85:352–358
Gresa-Arribas N, Titulaer MJ, Torrents A et al (2014) Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol 13:167–177
Arino H, Armangue T, Petit-Pedrol M et al (2016) Anti-LGI1-associated cognitive impairment: presentation and long-term outcome. Neurology 87:759–765
Leypoldt F, Hoftberger R, Titulaer MJ et al (2015) Investigations on CXCL13 in anti-N-methyl-d-aspartate receptor encephalitis: a potential biomarker of treatment response. JAMA Neurol 72:180–186
Watanabe M, Nakamura Y, Michalak Z et al (2019) Serum GFAP and neurofilament light as biomarkers of disease activity and disability in NMOSD. Neurology 93:e1299–e1311
Aktas O, Smith MA, Rees WA et al (2021) Serum glial fibrillary acidic protein: a neuromyelitis optica spectrum disorder biomarker. Ann Neurol 89:895–910
Chang X, Huang W, Wang L et al (2021) Serum neurofilament light and GFAP are associated with disease severity in inflammatory disorders with aquaporin-4 or myelin oligodendrocyte glycoprotein antibodies. Front Immunol 12:647618
Day GS, Yarbrough MY, Kortvelyessy P et al (2021) Prospective quantification of CSF biomarkers in antibody-mediated encephalitis. Neurology 96:e2546–e2557
Nissen MS, Ryding M, Nilsson AC et al (2021) CSF-neurofilament light chain levels in NMDAR and LGI1 encephalitis: a national cohort study. Front Immunol 12:719432
Galovic M, Al-Diwani A, Vivekananda U et al (2022) In vivo N-methyl-d-aspartate receptor (NMDAR) density as assessed using positron emission tomography during recovery from NMDAR-antibody encephalitis. JAMA Neurol
Bebawy JF (2012) Perioperative steroids for peritumoral intracranial EDEMA: a review of mechanisms, efficacy, and side effects. J Neurosurg Anesthesiol 24:173–177
Stellato C (2004) Post-transcriptional and nongenomic effects of glucocorticoids. Proc Am Thorac Soc 1:255–263
Coutinho AE, Chapman KE (2011) The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 335:2–13
Wust S, van den Brandt J, Tischner D et al (2008) Peripheral T cells are the therapeutic targets of glucocorticoids in experimental autoimmune encephalomyelitis. J Immunol 180:8434–8443
Balis FM, Lester CM, Chrousos GP, Heideman RL, Poplack DG (1987) Differences in cerebrospinal fluid penetration of corticosteroids: possible relationship to the prevention of meningeal leukemia. J Clin Oncol 5:202–207
Shin YW, Lee ST, Park KI et al (2018) Treatment strategies for autoimmune encephalitis. Ther Adv Neurol Disord 11:1756285617722347
Zhang Y, Huang HJ, Chen WB, Liu G, Liu F, Su YY (2021) Clinical efficacy of plasma exchange in patients with autoimmune encephalitis. Ann Clin Transl Neurol 8:763–773
Dubey D, Britton J, McKeon A et al (2020) Randomized placebo-controlled trial of intravenous immunoglobulin in autoimmune LGI1/CASPR2 epilepsy. Ann Neurol 87:313–323
Dogan Onugoren M, Golombeck KS, Bien C et al (2016) Immunoadsorption therapy in autoimmune encephalitides. Neurol (R) Neuroimmunol Neuroinflamm 3:e207
Thaler FS, Zimmermann L, Kammermeier S et al (2021) Rituximab treatment and long-term outcome of patients with autoimmune encephalitis: real-world evidence from the GENERATE registry. Neurol (R) Neuroimmunol Neuroinflamm 8:e1088
Cree BAC, Bennett JL, Kim HJ et al (2019) Inebilizumab for the treatment of neuromyelitis optica spectrum disorder (N-MOmentum): a double-blind, randomised placebo-controlled phase 2/3 trial. Lancet 394:1352–1363
Flanagan EP, Levy M, Katz E et al (2022) Inebilizumab for treatment of neuromyelitis optica spectrum disorder in patients with prior rituximab use from the N-MOmentum study. Mult Scler Relat Disord 57:103352
Lee WJ, Lee ST, Moon J et al (2016) Tocilizumab in autoimmune encephalitis refractory to rituximab: an institutional cohort study. Neurotherapeutics 13:824–832
Funding
This research was funded in whole or in part by a senior clinical fellowship from the Medical Research Council [MR/V007173/1], Wellcome Trust Fellowship [104079/Z/14/Z], BMA Research Grants- Vera Down grant (2013) and Margaret Temple (2017), Epilepsy Research UK (P1201), the Fulbright UK-US commission (MS-Society research award) and by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript (AAM) version arising from this submission. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
SRI has received honoraria and/or research support from UCB, Immunovant, MedImmun, Roche, Janssen, Cerebral therapeutics, ADC therapeutics, Brain, CSL Behring, and ONO Pharma, and receives licensed royalties on patent application WO/2010/046716 entitled 'Neurological Autoimmune Disorders’, and has filed two other patents, currently without licencees (“Diagnostic method and therapy”: WO2019211633 and US-2021-0071249-A1; PCT application WO202189788A1) and “Biomarkers” (PCT/GB2022/050614 and WO202189788A1).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Varley, J.A., Strippel, C., Handel, A. et al. Autoimmune encephalitis: recent clinical and biological advances. J Neurol 270, 4118–4131 (2023). https://doi.org/10.1007/s00415-023-11685-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11685-3