Abstract
Objective
To identify factors that patients consider when choosing between future in-person, video, or telephone visits.
Background
Telemedicine has been rapidly integrated into ambulatory neurology in response to the COVID-19 pandemic.
Methods
Ambulatory neurology patients at a single center were contacted via telephone to complete: (1) a survey quantifying likelihood of scheduling a future telemedicine visit, and (2) a semi-structured qualitative interview following their visit in March 2021. Data were processed using the principles of thematic analysis.
Results
Of 2493 visits, 39% assented to post-visit feedback; 74% were in-person visits and 13% video and telephone. Patients with in-person visits were less likely than those with video and telephone visits to “definitely” consider a future telemedicine visit (36 vs. 59 and 62%, respectively; p < 0.001). Patients considered five key factors when scheduling future visits: “Pros of Visit Type,” “Barriers to Telemedicine,” “Situational Context,” “Inherent Beliefs,” and “Extrinsic Variables.” Patients with telemedicine visits considered convenience as a pro, while those with in-person visits cited improved quality of care. Accessibility and user familiarity were considered barriers to telemedicine by patients with in-person and telephone visits, whereas system limitations were prevalent among patients with video visits. Patients agreed that stable conditions can be monitored via telemedicine, whereas physical examination warrants an in-person visit. Telemedicine was inherently considered equivalent to in-person care by patients with telephone visits. Awareness of telemedicine must be improved for patients with in-person visits.
Conclusion
Across visit types, patients agree that telemedicine is convenient and effective in many circumstances. Future care delivery models should incorporate the patient perspective to implement hybrid models where telemedicine is an adjunct to in-person visits in ambulatory neurology.
Similar content being viewed by others
Introduction
Although telestroke has existed since the mid-2000s, telemedicine in ambulatory neurology evolved rapidly in March 2020 [1,2,3]. In our facility, telemedicine was the only option for ambulatory care during the first 8 weeks of the COVID-19 pandemic. As mask mandates and social distancing guidelines were instituted, in-person visits were reintroduced. For the first time, amidst a persistent global health crisis, patients were given the option of scheduling in-person, video, or telephone visits. By March 2021, a hybrid model of care incorporating both in-person and telemedicine visits became common at many institutions in the US [4].
Previous studies have discussed numerous patient-reported benefits of telemedicine. Telemedicine eliminates commute time and cost, which is especially beneficial for patients traveling long distances to access subspecialty care [5,6,7]. Telemedicine also benefits patients with limited access to transportation, mobility concerns, and caregiver dependence [8]. However, barriers to telemedicine exist. At the pandemic’s outset, problematic Internet connection or poor audio/video quality was commonly reported among patients who completed video visits, and unfamiliarity with technology was more prevalent among patients who completed telephone visits [9]. Older, male, and Black patients, as well as those with Medicare or Medicaid insurance were less likely to schedule video visits [10]. While telemedicine’s use has increased, it is unknown whether these barriers persist and if they are presently influencing patients’ decisions regarding future visit type.
Healthcare will likely embrace a new normal with both in-person and telemedicine care. Some have even suggested that telemedicine services could be offered as an alternative to traditional in-person visits [11]. However, the extent of telemedicine’s expansion depends on many factors, including insurance coverage, provider resources, impact on patient outcomes, and patient preferences. The current study focuses on the latter, aiming to identify specific factors that patients consider when selecting future visit type and to determine whether these factors differ among patients who completed in-person, video, and telephone visits. A qualitative study was designed to understand the patient perspective at a time in the COVID-19 pandemic when three visit types (e.g., in-person, telephone, and video) were available. The goal of this study was to use the patient perspective to explore approaches to future care delivery models.
Methods
Design
A sequential mixed methods study was conducted including: (1) a telephone survey that quantified the type of visit and likelihood of scheduling a future telemedicine visit, and (2) a semi-structured, qualitative interview to determine the factors that influence patients’ decisions regarding future visit type.
Ethics
This study was reviewed and approved by the Wake Forest School of Medicine institutional review board (IRB#00065375). It was classified as Expedited Category 5, and it met criteria for a waiver of consent and a waiver of HIPAA authorization.
Intervention
By March 2021, telemedicine had been integrated into care delivery in the Department of Neurology at Atrium Health Wake Forest Baptist. When scheduling future appointments, patients were given the option to choose between in-person, video, or telephone visits.
All patients who completed an ambulatory in-person, video, or telephone visit in March 2021 were contacted within 4 months of their appointment in chronologic order. One of the nine team members (C.O., S.T., K.P., S.C., R.M., E.F., A.A., K.A.S., G.B.) contacted each patient once by telephone and did not leave a voicemail. Quantitative and qualitative feedback were obtained from verbally assenting patients. Among patients who had cognitive impairments or were young children, feedback was provided by an immediate caregiver or legal guardian who was present at the visit.
Quantitative methods
Assenting participants were asked two multiple choice questions to quantify: (1) the type of telemedicine visit, and (2) whether the patient would consider a future telemedicine visit (4-point Likert: [4] would definitely want a future telemedicine visit; [3] might consider; [2] would only consider if required; and [1] would not consider). Proportions of responses were analyzed between patients with in-person, video, and telephone visits via a two-sided Fisher’s exact test with predetermined statistical significance of α < 0.05.
Qualitative methods
During the interview, patients with in-person visits were asked, “If you were aware that telemedicine visits were an option prior to scheduling this in-person visit, would you have preferred a telemedicine visit and why?” Telemedicine patients were asked, “Would you have preferred an in-person visit and why?” Patient responses were documented verbatim and analyzed via Strauss and Corbin’s constant comparative method for thematic analysis.
An initial codebook was developed by two study facilitators (C.O., S.T.). They independently coded 50 patient responses and then debriefed to compare codes, discuss discrepancies, add or amend codes, and revise the codebook. Remaining discrepancies were resolved after further discussion with the primary study facilitator (R.E.S.). This process was successively repeated until data saturation in analysis was established at 150 patient responses. One study facilitator (C.O.) coded the remaining patient responses and discussed nuances (with S.T., R.E.S.) to ensure code accuracy. The frequency of individual codes were calculated according to visit type (% of total in-person, video, and telephone responses). Codes were then analyzed for thematic redundancies and organized into meta-themes (% of total codes) and representative sub-themes (% of meta-theme). These themes were compared according to in-person, video, or telephone visit types.
Data availability
The data that support study findings are available upon request.
Results
Demographics
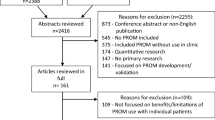
In March 2021, 2493 patients completed either an in-person, video, or telephone ambulatory visit. Contact was successfully made with 51% of patients (n = 1273); 39% assented (n = 962). Of the 962 assenting participants, 99% completed the quantitative survey (n = 951), and 96% assented to the qualitative interview (n = 924). Twelve visits were unable to be stratified (i.e., the visit started with video and transitioned to telephone) and thus were excluded from the analyses.
The patients who chose not to participate (n = 311) provided the following reasons: unavailable or busy (53%), no recollection of the specific telemedicine visit (6%), language barrier (5%), postponement of visit (2%), transition to a palliative care facility or nursing home (2%), deceased (2%), privacy concerns (1%), or disinterest due to participation in an alternative feedback survey (1%). Other patients were unable to communicate and the caregiver answering the call was not present at the appointment (9%). There were instances where no reasoning was provided (13%), the call was disconnected (3%), or the call was dropped (2%).
The mean age of all assenting participants was 44.7 ± 24.6 years. Most patients were identified as Caucasian (79%) or African American (14%); 559 were identified as female (58%) (Table 1). Participants’ average age and sex differed across visit type: participants who completed video visits were younger than those who completed both in-person and telephone visits (33 years vs. 46 and 49 years, respectively, p < 0.0001); participants who completed telephone visits were more likely to be female than those who completed in-person visits (68 vs. 56%, p = 0.018). Race did not significantly differ across visit types. Non-participants (n = 1531) included those who were not successfully contacted (n = 1220) or those who did not consent (n = 311). Non-participants had similar demographics (Table 1).
Quantitative study results
When stratified by visit type (n = 939), patients with in-person visits were less likely than patients with video and telephone visits to “definitely” consider a future telemedicine visit (36 vs. 59 and 62%, respectively; p < 0.001) (Fig. 1).
Patient responses to Question 2 of the quantitative telephone survey stratified by patient-reported visit type (in-person: n = 939; video: n = 120; telephone: n = 120). A significant difference (p < 0.01*) was found between the (1) patients who had in-person and video visits and (2) patients who had in-person and telephone visits who would “definitely” consider a future telemedicine visit
Qualitative study results
Five major themes (meta-themes) were identified as factors that patients consider when selecting future visit type: (1) “Pros of Visit Type,” (2) “Barriers to Telemedicine,” (3) “Situational Context,” (4) “Inherent Beliefs,” and (5) “Extrinsic Factors.” Each meta-theme subsequently comprised three to four sub-themes.
Factors that patients with in-person visits consider when selecting future visits
When selecting a future visit type, patients who completed in-person visits predominantly described “Pros of Visit Type” (Table 2). Patients were most likely to acknowledge elimination of commute time and associated cost as a pro of telemedicine (8% of total in-person responses), followed by several pros of in-person visits: improved communication (7%), improved quality of care (5%), and greater personability of the provider (5%). Patients deliberated these pros of visit types, stating, “We have a long drive, so…we would do it [virtually],” and “I just like it in-person because…you get a better sense of what’s going on and communicate better.” Patients completing in-person visits also frequently commented on “Barriers to Telemedicine.” The most prevalent barriers were user limitations such as the challenge of keeping children engaged (2%) and unfamiliarity with telemedicine (2%). Unfamiliarity was expressed by statements such as, “I’m old school—I like to see the doctor in-person.”
Forty-five percent of responses described “Situational Context,” or situations that are best suited for different visit types. In-person visits were preferred when a physical examination is required (10%), for worsening symptoms (5%), for an initial visit with an unknown diagnosis (4%), or for instances when a patient perceived their diagnosis to be more severe (e.g., Parkinson’s, ALS, or pediatric epilepsy; 4%). Telemedicine was preferred when patients did not require an in-person service (such as adjustments to deep brain stimulator settings; 6%) or for follow-up visits of stable conditions (5%).
Nine percent of in-person responses described “Inherent Beliefs.” At times, patients noted a lack of preference between telemedicine and in-person visits (2%), stating that telemedicine’s utility depends on their specific needs without providing further detail (3%). Other patients shared their belief that in-person visits are superior to telemedicine visits, in which case, they would only consider telemedicine as a last resort (2%). For instance, “If an in-person visit was not an option, then I would have done a telehealth appointment.”
Seven percent of responses cited “Extrinsic Variables” such as lack of awareness about telemedicine visits (5%).
Factors that patients with telemedicine visits consider when selecting future visits
For patients who completed a telemedicine visit, the most commonly reported “Pros of Visit Type” was convenience of telemedicine, yet greater personability of the physician at in-person visits was also frequently acknowledged (6% of video and 7% of telephone) (Table 3). Convenience included the elimination of commute time and cost (12% for both visit types) and the ease for patients with limited mobility (3% for both). One patient’s spouse remarked, “Telephone was fine because it takes a lot of work with the wheelchair to get into the office now.” Others commented, “I just felt it [the video visit] was not as personable. There’s something about being face-to-face. Even though we can still see each other, it is not the same.”
“Situational Context” was highly considered by patients with telemedicine visits (40% of video responses and 39% of telephone). Patients commented on telemedicine’s utility for: follow-up of stable conditions (5% for both), annual visits (2% and 3%), or instances where in-person services were not needed (6 and 3%, respectively). In-person visits were preferred for worsening symptoms (7% and 16%) or physical examination (10% and 11%). Patients often emphasized physical examination as a driving factor for in-person visits: “If there was something that I felt needed to be physically examined, then we would come in.”
Within “Inherent Beliefs” (12% of video responses and 14% of telephone) some patients commented that telemedicine offers an equivalent quality of care to in-person visits (3% and 4%), with no general preference for visit type (4% for both). One patient remarked, “It did not matter one way or the other. She was just as effective on video.” Patients also commented that the use of telemedicine may “depend on what the appointment was for” (2% and 3%).
Both visit types were influenced by “Extrinsic Variables” such as alternate decision-makers (1% for both). One patient said, “I did not choose [the video visit]. That’s just what they [clinic staff] told me.”
Video versus telephone visits: comparison of factors that patients consider
Although telemedicine patients similarly emphasized convenience as a “Pros of Visit Type,” patients who completed video visits were more likely to acknowledge a broader spectrum of convenience. They recognized convenience for full-time employees, students, and parents, as well as decreased wait time at a telemedicine appointment. A parent stated, “[the patient] is a student, so I do not want to take him out of school for one day. This way, he only misses a little [bit of school].” The only form of convenience that patients with telephone visits noted more frequently than video was telemedicine’s elimination of transportation needs. One patient said, “Right now, I do not have a vehicle, so [telemedicine] is a lot easier.” Patients who completed telephone visits were also more likely to value safety compared to video: “With everything going on [COVID], I would have preferred it over the phone. I feel safer.”
For “Barriers to Telemedicine,” reliance on self-reported symptoms and system limitations including poor Internet connection were more frequently cited as barriers to video visits. For instance, “The reception is not always good on the video call. Sometimes, it lags, or the call drops, you know? I just think it’s easier to come in-person.” Comparatively, user limitations, especially unfamiliarity with technology, were cited as barriers among telephone users. The belief that telemedicine is difficult for children due to distractibility was a user limitation unique to video visits. Accessibility challenges including need for assistance with technology and insurance coverage were more prevalent among telephone users.
When considering “Situational Context,” patients with telephone visits were more likely to prefer in-person visits for severe or undiagnosed conditions. These patients choose in-person visits for worsening or recurring symptoms. One patient described, “If I had another episode, I’d like to see the doctor in-person.” They were also more likely to consider in-person visits for a physical examination (76% vs. 54% of sub-theme). In comparison, patients who completed video visits considered multiple indications for in-person visits beyond worsening symptoms: initial visits with a new provider when a diagnosis is unknown, severe diagnosis, or for service requirements such as Botox.
Patients who completed telephone visits held “Inherent Beliefs” that telemedicine and in-person visits are equivalent in quality of care, physical exam, and effective communication. Patients with video visits were more likely to express indifference between visit types, indicating that telemedicine is a suitable alternative to in-person visits specifically during the pandemic. For example, “In these circumstances [COVID-19 pandemic], I get it.”
For “Extrinsic Variables” patients who completed video visits were more likely to choose telemedicine based on availability (i.e., if the virtual appointment was offered sooner than in-person).
In-person versus video visits: comparison of factors that patients consider
Responses between patients with in-person and video visits differed most within sub-themes of: (1) “Pros of Visit Type,” (2) “Barriers to Telemedicine,” and (3) “Inherent Beliefs.” Overall, patients with video visits were more likely to consider convenience as a “Pros of Visit Type” (61% vs. 39% of meta-theme). Of all responses that pertain to convenience of telemedicine, patients with in-person visits were more likely to cite a specific form of convenience: the elimination of transportation needs, commute time, and cost. “Barriers to Telemedicine” greatly differed between these two visit types. Patients with video visits considered system limitations such as unreliable Internet connection, whereas patients with in-person visits considered user limitations such as unfamiliarity with technology. Importantly, patients with in-person visits report decreased accessibility—most prominently the lack of access to a telehealth device. In terms of “Inherent Beliefs,” patients with video visits reported more indifference when selecting visit type. Aside from these differences, patients agreed within sub-themes of “Situational Context,” finding telemedicine visits best for follow-up appointments. In-person visits were preferred for annual appointments, instances when in-person services are needed, or instances when a physical examination is required.
In-person versus telephone visits: comparison of factors that patients consider
Responses between patients with in-person and telephone visits differed most within sub-themes of: (1) “Pros of Visit Type,” (2) “Situational Context,” and (3) “Inherent Beliefs.” Patients with telephone visits were most likely to value safety as a “Pros of Visit Type” (15% vs. 6%). Within “Situational Context,” they were also more likely to select in-person visits for severe or undiagnosed conditions. Patients with in-person visits were far more likely to prefer an in-person encounter for initial visits with a new provider, for severe diagnoses, or for situations where in-person services or Botox were required. They cited instances where traditional benefits of telemedicine do not apply (e.g., patient lives or works in close proximity to the clinic, or patient feels safe at in-person visits due to COVID-19 vaccination and sanitary protocols). Patients with telephone visits were more likely to cite the “Inherent Belief” that telemedicine and in-person visits provide an equivalent quality of care, whereas patients with in-person visits reported that telemedicine should only be used as a last resort. Patients of both visit types agreed that barriers are prevalent, especially the user limitation of unfamiliarity with telemedicine.
Discussion
This study envisions an optimal future care model by investigating specific factors that patients consider when choosing between video, telephone, and in-person ambulatory neurology visits (Fig. 2). Overall, patients who completed video visits value convenience and support when selecting future visit type, while patients who completed telephone visits strongly emphasized safety. Comparatively, patients who completed in-person visits value confidence and trust. Barriers to telemedicine were cited among patients who completed all visit types, but they were most prevalent among patients who completed in-person visits due to unfamiliarity with virtual platforms and lack of access to telehealth devices. Perhaps not surprisingly, patients with in-person visits were least likely to consider future telemedicine visits, and they were significantly older than patients who completed video visits. Despite these differences, patients of all visit types agreed that in-person visits are best suited for severe conditions or visits that may require in-person services, while telemedicine is better for monitoring stable conditions. This patient perspective will be imperative to the integration of telemedicine in future care delivery models.
Patients with in-person visits strongly value confidence and trust. These patients were most likely to inherently believe that in-person visits are safe in spite of COVID-19, reflecting their trust in public health policies and their value of physical interaction with a provider. Quality of care, provider personability, and improved communication at in-person visits are important in building trust in their physician; however, this trust cannot always be established via telemedicine. Some patients who completed in-person visits were agreeable to utilizing telemedicine in specific situations (due to the benefit of elimination of commute time and cost); but others believed that in-person care delivery will always be superior. These mixed opinions may explain the lower quantitative preference for future telemedicine visits by patients who completed an in-person visit. Patients with in-person visits report a greater need for in-person services (e.g., DBS programming, Botox injections, or diagnostic studies such as nerve conduction testing), which could also skew satisfaction as these needs cannot be accomplished remotely. The quantitative findings emphasize that these patients’ permanent need for in-person services will outweigh any “pro” that telemedicine can offer.
Alternatively, patients with in-person visits may not consider future telemedicine visits due to user limitations. These patients were most likely to cite their unfamiliarity with telemedicine, explaining, “It [an in-person visit] is how I’ve always done it.” This may be related to the significantly older age of patients who completed in-person visits compared to those who completed video visits. A recent study found that patients reported lower success rates with their telephone visit when it was an initial consultation, suggesting that familiarity with the virtual medium may limit satisfaction [12]. Previously, familiarity has been shown to improve with the utilization of web-based applications that support appointment scheduling, online consultation, test result follow-up, prescription completion, medication delivery, and most importantly, health insurance coverage [13]. To continue telemedicine’s integration in ambulatory neurology, familiarity must be addressed among patients who traditionally choose in-person visits in order to build confidence and trust in virtual care.
Responses from patients with video visits reveal that their decisions are most influenced by values of convenience and support. The significantly younger age of these patients is consistent with the high number of responses citing convenience for full-time employees, students, and working parents. This exemplifies how video users value a broader spectrum of convenience, beyond the elimination of commute time and cost, which was highly prevalent among all visit types. Additionally, these patients were least likely to cite convenience due to elimination of transportation needs, and they were least likely to cite barriers of lack of access to a telehealth device or need for technological assistance. These findings may suggest that younger patients who completed video visits face fewer socioeconomic barriers than patients who completed telephone or in-person visits. They are perhaps the most familiar with technology, as system limitations (rather than user limitations) were most apparent among patients with video visits. Because these younger patients represent our future patient cohort, their identification of system limitations to telemedicine adoption reinforce that even if familiarity and access improve over time, high-speed Internet connection will be essential to telemedicine’s permanent integration. Previous studies have shown that a significant portion of American homes do not have Internet access, including those of underrepresented minorities, rural residents, older individuals, and those with Medicaid or Medicare insurance [14]. To prevent telemedicine from worsening these existing healthcare disparities, policies must focus on improving Internet access in addition to addressing availability of telehealth equipment and user unfamiliarity.
Beyond illuminating the aforementioned differences in accessibility and user limitations, responses from patients with telephone visits reveal a pronounced emphasis on safety. Patients who completed telephone visits are comfortable using telemedicine for future follow-up visits and annual appointments with an established provider. This is likely due to the benefit of avoiding potential COVID-19 exposures, which was especially important to immunosuppressed neurological patients. However, patients who completed telephone visits had very clear indications for selecting in-person visit types during situations when safety is compromised. When the risk of declining health outweighs telemedicine benefits, these patients seek evaluation of their worsening symptoms via an in-person neurologic exam. In these circumstances, the perception of improved personability during in-person conversations may contribute to feelings of improved safety. The lack of visual cues inherent to telephone visits limits non-verbal communication and dampens the reassurance of hands-on physical examination. Future outcomes studies will be needed to assess the patient’s ability to accurately predict when in-person examination is necessary, as there may be instances when a patient cannot perceive subtle changes in neurologic function. Alternatively, telemedicine may expand to include web-based tools that add objective data to the virtual neurologic exam. For example, mobile applications that aid in visual field assessments or wearable devices that monitor parameters of gait to predict disease progression have been studied [15, 16]. Such tools will also require further investigation in order to delineate whether they yield differences in patient outcomes compared to in-person assessments.
Outcome studies may also help to modify preexisting negative inherent beliefs about telemedicine. In this study, patients with in-person visits report that telemedicine is inferior to in-person visits and should only be utilized only as a last resort, while patients with video visits believe that telemedicine is a suitable alternative to in-person visits, and patients with telephone visits consider quality of care to be equivalent across visit types. Future studies that thoroughly investigate patient definitions of quality of care, as well as medically relevant outcomes such as emergency department visits and hospital admissions, for example, may promote consensus in inherent beliefs across visit types.
Proposed solutions
High physician satisfaction with telemedicine has been shown to support its adoption [17]. Thus, increasing physician comfort with telehealth technology may promote acknowledgement of its efficacy and usefulness, encouraging physicians to inform patients of this service. Physician training on communication strategies that facilitate the virtual patient-physician relationship may help to establish equivalent personability and communication, qualities that our patients suggested were benefits of in-person visits. Moving forward, the responsibility of patient awareness should be shared among physicians, insurance providers, and administrative staff. Online portals can support scheduling via a decision tree to guide selection of appropriate visit type based on diagnosis or current situation, which may optimize telemedicine’s use for follow-up visits of stable, less severe conditions. One study suggests that these “Situational Factors” such as stability and severity may influence visit satisfaction, as patients and neurologists were more likely to perceive that their visit goals were achieved when the telemedicine visit was a follow-up consultation as opposed to a new visit [12]. To improve access, administrative staff, caregivers, and travel nurses can provide support with technology to attenuate user limitations. Additional broadband mapping studies aimed at expanding accessibility will be necessary to overcome system limitations—a primary barrier to our current and future patients. Furthermore, development of telemedicine centers, utilization of libraries and other public spaces, and creation of state and federal partnerships with Internet service providers may address Internet access issues more broadly [18].
Strengths and limitations
The timing of this study is a strength for several reasons. Shortly after the completion of this study, availability of telephone visits was reduced at our institution due to reimbursement concerns. This study was therefore conducted during a critical period when all three visit types were offered equally and fully reimbursed, meaning that financial bias was unlikely confounding patient preferences, strengthening the reliability of the results. Additionally, this study was performed prior to the emergence of the COVID-19 delta-variant when percent of vaccinated individuals were increasing and COVID-19-related hospitalizations were declining. This period of time is ideal for evaluating the patient preference, as general knowledge surrounding COVID-19 was well disseminated, and patients were able to logically explain their decision-making process regarding visit type. A final strength includes the validity of the “Barriers to Telemedicine” data that pertains to technology. In comparison to the early pandemic period when telemedicine was novel, patients had become increasingly familiar with virtual platforms, and software updates had improved user-friendliness and functionality. Therefore, this study offers a more accurate depiction of long-term technology barriers. Rather than reflecting singular negative experiences where connections were “glitchy,” patient responses depict instances where technology prevented selection of a future telemedicine visit: “I prefer telephone over video only because I live in a rural area, and the virtual video conference freezes.”
Although the large number of study participants represented a clinically diverse population, responses were increasingly subject to recall bias over time. Patients contacted near the beginning of the study were responding within 1 month of their neurology visit, whereas patients contacted near the end of the study were responding within 3–4 months of their visit (Table 1). Because visit type was determined during the quantitative interview and used to stratify qualitative responses, some responses may have been incorrectly stratified. Additionally, 12 patient responses were excluded due to the inability to stratify them by visit type (their appointment started as a video visit and transitioned to a telephone visit). As these patients may have been more likely to report a negative experience with telemedicine, selection bias is possible. Similarly, assenting participants (39%, n = 962/2493) may be more likely to report extreme positive or negative opinions and thus may not adequately represent the neurology patient population. It is also possible that patients who chose in-person, video, and telephone visits differ from each other, introducing source bias. However, the large number of assenting participants minimizes these possibilities. Lastly, our institution does not “room” patients with telemedicine visits (e.g., mental health screenings, fall risk assessment, or medication review), which may have influenced qualitative responses related to “thoroughness” or quality of medical care. As the study population is restricted to a single academic institution, it may not be generalizable to all ambulatory neurology practices.
Conclusions
The optimal role and future success of telemedicine in our healthcare system is contingent upon understanding the patient perspective. Physicians, insurance companies, healthcare institutions, and all levels of government must continue to center the patient voice as telemedicine policies and care delivery models are developed. Physicians must also continue to build experience with telemedicine as their perspectives are invaluable to a future hybrid model. In this study, patients describe their ideal future care model as one that is flexible and offers both telemedicine and in-person visits. Patients consistently report that telephone and video visits are best for follow-up care of stable conditions, while in-person visits are preferred for declines in baseline health or instances where in-person services (physical neurological examination, diagnostic or treatment services) are necessary. Telemedicine barriers of accessibility and technological limitations—especially Internet connection—must be addressed, and providers must continue to emphasize communication and personability. Future outcomes studies are needed to ensure quality of care is consistent regardless of visit type.
References
Schwamm LH, Holloway RG, Amarenco P et al (2009) A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American heart association/American stroke association. Stroke 40(7):2616–2634. https://doi.org/10.1161/STROKEAHA.109.192360
Powers WJ, Rabinstein AA, Ackerson T et al (2018) 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 49(3):e46–e110. https://doi.org/10.1161/STR.0000000000000158
Adeoye O, Nystrom KV, Yavagal DR et al (2019) Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American stroke association. Stroke 50(7):e187–e210. https://doi.org/10.1161/STR.0000000000000173
Scaglione T, Kuzbyt B (2021) Tinnitus management: the utilization of a hybrid telehealth and in-person delivery model. Semin Hear 42(2):115–112. https://doi.org/10.1055/s-0041-1731692
Kruse CS, Krowski N, Rodriguez B et al (2017) Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. https://doi.org/10.1136/bmjopen-2017-016242
Wechsler LR, Tsao JW, Levine SR et al (2013) Teleneurology applications: report of the telemedicine work group of the american academy of neurology. Neurology 80(7):670–676. https://doi.org/10.1212/WNL.0B013E3182823361
Wechsler LR (2015) Advantages and limitations of teleneurology. JAMA Neurol 72(3):349–354. https://doi.org/10.1177/1357633X15589534
Hatcher-Martin JM, Adams JL, Anderson ER et al (2020) Telemedicine in neurology: telemedicine work group of the American academy of neurology update. Neurology 94(1):30–38. https://doi.org/10.1212/WNL.0000000000008708
Olszewski C, Thomson S, Strauss L et al (2021) Patient experiences with ambulatory telehealth in neurology: results of a mixed methods study. Neurol Clin Pract. https://doi.org/10.1212/CPJ.0000000000001072
Strowd RE, Strauss L, Graham R et al (2020) Rapid implementation of outpatient teleneurology in rural appalachia: barriers and disparities. Neurol Clin Pract. https://doi.org/10.1212/CPJ.0000000000000906
Reider-Dermer MM, Eliashiv D (2018) Expanding the use of telemedicine in neurology: a Pilot Study. J Manuf Technol Manag 7(2):46–50. https://doi.org/10.7309/jmtm.7.2.6
Nakornchai T, Conci E, Hensiek A et al (2021) Clinician and patient experience of neurology telephone consultations during the COVID-19 pandemic. Postgrad Med J. https://doi.org/10.1136/postgradmedj-2021-141234
Tang Y, Xing Y, Cui L et al (2020) Neurology practice during the COVID-19 outbreak and post-pandemic era: experiences and challenges. Eur J Neurol. https://doi.org/10.1111/ene.14445
Amin K, Rae M, Ramirez G et al. (2020) How might internet connectivity affect health care access? Kaiser family foundation health system tracker. https://www.healthsystemtracker.org/chart-collection/how-might-internet-connectivity-affect-health-care-access/#item-start. Accessed 8 Oct 2021
Ko MW, Busis NA (2020) Tele-neuro-ophthalmology: vision for 20/20 and beyond. J Neuroophthamol. https://doi.org/10.1097/WNO.0000000000001038
Sola-Valls N, Blanco Y, Sepulveda M et al (2015) Walking function in clinical monitoring of multiple sclerosis by telemedicine. J Neurol. https://doi.org/10.1007/s00415-015-7764-x
Kissi J, Dai B, Dogbe CSK (2019) Predictive factors of physicians’ satisfaction with telemedicine services acceptance. Health Inform J 26(3):1866–1880. https://doi.org/10.1177/1460458219892162
DeGuzman PB, Bernacchi V, Cupp CA et al (2020) Beyond broadband: digital inclusion as a driver of inequities in access to rural cancer care. J Cancer Surviv 14:643–652. https://doi.org/10.1007/s11764-020-00874-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Carly Olszewski has no relevant financial or non-financial interests to disclose. Sharon Thomson has no relevant financial or non-financial interests to disclose. Kelly Pring has no relevant financial or non-financial interests to disclose. Siobhan Cox has no relevant financial or non-financial interests to disclose. Rebecca Merrill has no relevant financial or non-financial interests to disclose. Emily Fishman has no relevant financial or non-financial interests to disclose. Alexander Ambrosini has no relevant financial or non-financial interests to disclose. K. Alexander Soltany has no relevant financial or non-financial interests to disclose. Gabby Bognet has no relevant financial or non-financial interests to disclose. Dr. Lauren D. Strauss has no relevant financial or non-financial interests to disclose. Rachel Graham has no relevant financial or non-financial interests to disclose. Dr. Amy Guzik has no relevant financial or non-financial interests to disclose. Dr. Roy E. Strowd serves as a consultant for Monteris Medical Inc., Novocure, and Nanobiotix. He receives an editorial stipend as Deputy Section Editor of the Resident and Fellow Section of Neurology® and has received research/grant support from the American Academy of Neurology, American Society for Clinical Oncology, Southeastern Brain Tumor Foundation, and Jazz Pharmaceuticals.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Olszewski, C., Thomson, S., Pring, K. et al. A comparison of telemedicine and in-person neurology visits: what are the factors that patients consider when selecting future visit type?. J Neurol 269, 5022–5037 (2022). https://doi.org/10.1007/s00415-022-11149-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11149-0