Abstract
Background
Deep-brain stimulation (DBS) programming for dystonia patients is a complex and time-consuming task.
Objective
To analyze whether programming a programming paradigm based on patient’s self-adjustment is practical, effective and time saving in dystonia.
Methods
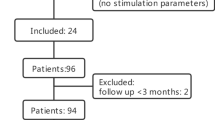
We retrospectively compared dystonia rating scales as well as the time necessary to optimize programming and the number of in-hospital visits in all patients (n = 102) operated at our center who used simple mode (SM) or advanced mode (AM) programming; the latter uses groups of different stimulation parameters and allows the patient and their caregiver to change stimulation groups at home, using the patient remote control.
Results
Both AM- and SM-allocated patients improved clinically to the same extent after DBS, as assessed by the Burke–Fahn–Marsden (BFM) and the Toronto Western Spasmodic Torticollis (TWSTRS) dystonia rating scales. All subscores improved after DBS without statistically significant differences in improvement between AM and SM (BFM: − 43% vs. − 53%, p = 0.569; TWSTRS: − 63% vs. − 72%, p = 0.781). AM and SM patients reached optimization within a similar median time [5.5 months (95% CI 4.6–6.3) for AM vs. 6.2 months (4.2–7.6) for SM, p = 0.674) but patients on advanced programming needed fewer in-hospital visits to achieve the same improvement [median of 5 visits (95% CI 4–7) for AM vs. 8 visits (7–9) for SM, p = 0.008].
Conclusions
Advanced DBS programming based on patient’s self-adjustment under the supervision of the treating physician is feasible, practical and significantly reduces consultation time in dystonia patients.



Similar content being viewed by others
References
Morgante F, Klein C (2013) Dystonia. Contin Lifelong Learn Neurol 19:1225–1241
Picillo M, Lozano AM, Kou N, Munhoz RP, Fasano A (2016) Programming deep brain stimulation for tremor and dystonia: the Toronto Western Hospital algorithms. Brain Stimul 9(3):438–452
Walsh RA, Sidiropoulos C, Lozano AM, Hodaie M, Poon Y-Y, Fallis M et al (2013) Bilateral pallidal stimulation in cervical dystonia: blinded evidence of benefit beyond 5 years. Brain 136(3):761–769
Moro E, LeReun C, Krauss JK, Albanese A, Lin J-P, Walleser Autiero S et al (2017) Efficacy of pallidal stimulation in isolated dystonia: a systematic review and meta-analysis. Eur J Neurol 24(4):552–560
Loher TJ, Capelle H-H, Kaelin-Lang A, Weber S, Weigel R, Burgunder JM et al (2008) Deep brain stimulation for dystonia: outcome at long-term follow-up. J Neurol 255(6):881–884
Vidailhet M, Jutras M-F, Grabli D, Roze E (2013) Deep brain stimulation for dystonia. J Neurol Neurosurg Psychiatry 84(9):1029–1042
FitzGerald JJ, Rosendal F, de Pennington N, Joint C, Forrow B, Fletcher C et al (2014) Long-term outcome of deep brain stimulation in generalised dystonia: a series of 60 cases. J Neurol Neurosurg Psychiatry 85(12):1371–1376
Volkmann J, Wolters A, Kupsch A, Müller J, Kühn AA, Schneider G-H et al (2012) Pallidal deep brain stimulation in patients with primary generalised or segmental dystonia: 5-year follow-up of a randomised trial. Lancet Neurol 11(12):1029–1038
Kupsch A, Benecke R, Müller J, Trottenberg T, Schneider G-H, Poewe W et al (2006) Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med 355(19):1978–1990
Meoni S, Fraix V, Castrioto A, Benabid AL, Seigneuret E, Vercueil L et al (2017) Pallidal deep brain stimulation for dystonia: a long term study. J Neurol Neurosurg Psychiatry 88(11):960–967
Stiggelbout AM, Van der Weijden T, De Wit MPT, Frosch D, Légaré F, Montori VM et al (2012) Shared decision making: really putting patients at the centre of healthcare. BMJ 344:e256
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P et al (2012) Shared decision making: a model for clinical practice. J Gen Intern Med 27(10):1361–1367
Elwyn G, Miron-Shatz T (2010) Deliberation before determination: the definition and evaluation of good decision making. Health Expect 13(2):139–147
Nijhuis FAP, Elwyn G, Bloem BR, Post B, Faber MJ (2018) Improving shared decision-making in advanced Parkinson’s disease: protocol of a mixed methods feasibility study. Pilot Feasibility Stud 4:94
Acknowledgements
We thank Dr. Sean Udow for the review of the English language.
Author information
Authors and Affiliations
Contributions
(1) Research project: A. conception, B. organization, C. execution; (2) statistical analysis: A. design, B. execution, C. review and critique; (3) manuscript: A. writing of the first draft, B. review and critique. JFB: 1B, 1C, 2A, 2B, 3A. MR: 1B, 1C, 3B. MRL: 1C, 3B. VP: 1C. RPM: 3B. MH: 1C, 3B. SKK: 1C, 3B. AML: 1C, 3B. PRB: 3B. AP: 2A, 2B, 3B. AF: 1A, 1B, 2C, 3B.
Corresponding author
Ethics declarations
Conflicts of interest
The manuscript has not been previously published and is not under review at any other journal. No other related work is under submission elsewhere. All the authors of the paper have participated to the study, revised the manuscript and approved the final version of the manuscript. There is no ghost writer. AF and AML received research funding and honoraria from Medtronic. The other authors (JFB, MR, MRL, VP, RPM, MH, SKK, PRB, and AP) have no disclosure of conflict of interest related to this work.
Ethical approval
The manuscript is a retrospective review from our Movement Disorders Center database and as such there was neither ethics committee nor patients’ consent specific to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bally, J.F., Rohani, M., Ruiz-Lopez, M. et al. Patient-adjusted deep-brain stimulation programming is time saving in dystonia patients. J Neurol 266, 2423–2429 (2019). https://doi.org/10.1007/s00415-019-09423-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09423-9