Abstract
Background
In patients with late-onset Pompe disease, progressive respiratory muscle weakness with predominantly diaphragmatic involvement is a frequent finding at later stages of the disease. Respiratory muscle training (RMT) is an established therapy option for patients with several neuromuscular disorders including Duchenne muscular dystrophy. Forced voluntary muscle contractions of inspiration and/or expiration muscles enhance ventilation by increasing respiratory coordination, endurance, and strength. Efficacy of RMT in LOPD is rarely examined, and the clinical studies performed are difficult to compare because of different training programs and protocols. This impedes a useful statement and recommendation about the safety and efficacy of respiratory muscle training.
Methods
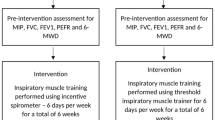
We conducted a monocentric unblinded single-arm pilot study in patients with LOPD to evaluate the safety and efficacy of inspiratory muscle training (IMT). The primary objective was to determine the efficacy of a 6-week repetitive IMT with a gradual increase of inspiratory resistance, measured by MIP (maximum inspiratory pressure) in the upright position. For statistical analysis, we used an A–B–C single subject design. The 6-week training-period A was followed by a 6-week non-training period B and an optional training period of 40 weeks in period C. The total study duration for the periods A, B and C was 52 weeks. Throughout the study, spirometry assessments (FCV, FEV1) and measurements of respiratory strength (MIP, MEP) were performed at defined time points, as well as capillary oximetry and capnometry, motor function test and patient’s questionnaires for quality of life and dyspnea, measured by St. George’s Respiratory Questionnaire (SGRQ) and MMRC-Dyspnea scale. For the cross-sectional comparison, a paired two-sided t test, and for the longitudinal comparison, a two-sample, two-sided t test were used. When data were not normally distributed, a Wilcoxon–Mann–Whitney test was added. Finally, the annual decline in FVC and FEV1 before and after IMT was compared.
Findings
11 subjects were included in this pilot study. Overall, IMT was well tolerated. In four subjects, a total of six adverse events related to the study procedures were noticed. Training compliance was excellent in the first weeks of training, but declined continuously in the extension period. There was a significant increase in our primary outcome measure MIP within the 6-week period of frequent IMT with a mean of 15.7% (p =0.024; d =0.402). A significant increase was also seen after week 52 by a mean of + 26.4% (mean + 13.4 cmH2O, p =0.001, d =0.636). In the 6-week non-training interim-period (period B), the values remained stable, and there was no clinically meaningful decline in secondary outcome measures. The increase in MIP did not have any effect on secondary outcome measures like spirometry tests (FVC, FEV1), capillary blood gas analysis, motor function tests, patient’s perceived quality of life or any significant change in dyspnea score.
Conclusions
Frequent IMT improves MIP and thereby stabilizes and decelerates the decline of the diaphragm strength. The gradual increase of inspiratory resistance is well tolerated without any increase of side effects, as long as IMT is supervised and resistance is individually adjusted to the patient’s perceived grade of exhaustion. Although we could not detect a significant impact on secondary outcome measures, IMT should be offered to all LOPD patients, especially to those who demonstrate a progressive decline in respiratory muscle function or are unable to receive ERT.






Similar content being viewed by others
References
Meikle PJ et al (1999) Prevalence of lysosomal storage disorders. JAMA 281(3):249–254
Poorthuis BJ et al (1999) The frequency of lysosomal storage diseases in The Netherlands. Hum Genet 105(1–2):151–156
Filosto M et al (2013) Non-muscle involvement in late-onset glycogenosis II. Acta Myol 32(2):91–94
van der Ploeg AT, Reuser AJ (2008) Pompe’s disease. Lancet 372(9646):1342–1353
Schuller A et al (2012) Toward deconstructing the phenotype of late-onset Pompe disease. Am J Med Gen Part C Semin Med Genet 160C(1):80–88
Boentert M et al (2015) Sleep-related symptoms and sleep-disordered breathing in adult Pompe disease. Eur J Neurol 22(2):369–376 (e27)
Mellies U, Lofaso F (2009) Pompe disease: a neuromuscular disease with respiratory muscle involvement. Respir Med 103(4):477–484
Wenninger S, Schoser B (2015) Behandelbare neuromuskuläre Erkrankungen als wichtige Differentialdiagnose der chronisch-progredienten Dyspnoe im höheren Erwachsenenalter. Der Pneumologe, pp 1–4
Winkel LP et al (2005) The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 252(8):875–884
Gungor D et al (2011) Survival and associated factors in 268 adults with Pompe disease prior to treatment with enzyme replacement therapy. Orphanet J Rare Dis 6:34
Prigent H et al (2012) Supine volume drop and diaphragmatic function in adults with Pompe disease. Eur Respir J 39(6):1545–1546
van der Ploeg AT et al (2010) A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med 362(15):1396–1406
van der Beek NA et al (2011) Rate of progression and predictive factors for pulmonary outcome in children and adults with Pompe disease. Mol Genet Metab 104(1–2):129–136
Schoser B et al (2016) Survival and long-term outcomes in late-onset Pompe disease following alglucosidase alfa treatment: a systematic review and meta-analysis. J Neurol 264(4):621–630. https://doi.org/10.1007/s00415-016-8219-8
Winkel LP et al (2004) Enzyme replacement therapy in late-onset Pompe’s disease: a three-year follow-up. Ann Neurol 55(4):495–502
Koeberl DD, Kishnani PS, Chen YT (2007) Glycogen storage disease types I and II: treatment updates. J Inherit Metab Dis 30(2):159–164
Kishnani PS et al (2007) Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology 68(2):99–109
Toscano A, Schoser B (2013) Enzyme replacement therapy in late-onset Pompe disease: a systematic literature review. J Neurol 260(4):951–959
de Vries JM et al (2012) Effect of enzyme therapy and prognostic factors in 69 adults with Pompe disease: an open-label single-center study. Orphanet J Rare Dis 7:73
Vianello A et al (2013) Enzyme replacement therapy improves respiratory outcomes in patients with late-onset type II glycogenosis and high ventilator dependency. Lung 191(5):537–544
Schoser B et al (2017) Maximum inspiratory pressure as a clinically meaningful trial endpoint for neuromuscular diseases: a comprehensive review of the literature. Orphanet J Rare Dis 12(1):52
Boentert M, Wenninger S, Sansone VA (2017) Respiratory involvement in neuromuscular disorders. Curr Opin Neurol 30(5):529–537
Borge CR et al (2014) Effects of controlled breathing exercises and respiratory muscle training in people with chronic obstructive pulmonary disease: results from evaluating the quality of evidence in systematic reviews. BMC Pulm Med 14:184
Gozal D, Thiriet P (1999) Respiratory muscle training in neuromuscular disease: long-term effects on strength and load perception. Med Sci Sports Exerc 31(11):1522–1527
Vilozni D et al (1994) Computerized respiratory muscle training in children with Duchenne muscular dystrophy. Neuromuscul Disord 4(3):249–255
Rodillo E et al (1989) Respiratory muscle training in Duchenne muscular dystrophy. Arch Dis Child 64(5):736–738
Enright SJ, Unnithan VB (2011) Effect of inspiratory muscle training intensities on pulmonary function and work capacity in people who are healthy: a randomized controlled trial. Phys Ther 91(6):894–905
Enright SJ et al (2006) Effect of high-intensity inspiratory muscle training on lung volumes, diaphragm thickness, and exercise capacity in subjects who are healthy. Phys Ther 86(3):345–354
Leith DE, Bradley M (1976) Ventilatory muscle strength and endurance training. J Appl Physiol 41(4):508–516
Nici L et al (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 173(12):1390–1413
Aslan GK et al (2014) Effects of respiratory muscle training on pulmonary functions in patients with slowly progressive neuromuscular disease: a randomized controlled trial. Clin Rehabil 28(6):573–581
Jones HN et al (2014) Effects of respiratory muscle training (RMT) in children with infantile-onset Pompe disease and respiratory muscle weakness. J Pediatr Rehabil Med 7(3):255–265
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Aggarwal AN, Agarwal R (2007) The new ATS/ERS guidelines for assessing the spirometric severity of restrictive lung disease differ from previous standards. Respirology 12(5):759–762
Criée C et al (2015) Leitlinie zur Spirometrie Leitlinie der Deutschen Atemwegsliga, der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin und der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin zur Spirometrie. Pneumologie 69(3):147–164
Human A et al (2017) Inspiratory muscle training for children and adolescents with neuromuscular diseases: a systematic review. Neuromuscul Disord 27(6):503–517. https://doi.org/10.1016/j.nmd.2017.03.009
Hsiao SF et al (2003) Comparison of effectiveness of pressure threshold and targeted resistance devices for inspiratory muscle training in patients with chronic obstructive pulmonary disease. J Formos Med Assoc 102(4):240–245
Shoemaker MJ, Donker S, Lapoe A (2009) Inspiratory muscle training in patients with chronic obstructive pulmonary disease: the state of the evidence. Cardiopulm Phys Ther J 20(3):5–15
Jones HN et al (2016) Respiratory muscle training (RMT) in late-onset Pompe disease (LOPD): effects of training and detraining. Mol Genet Metab 117(2):120–128
Aslan GK et al (2016) Inspiratory muscle training in late-onset Pompe disease: the effects on pulmonary function tests, quality of life, and sleep quality. Lung 194(4):555–561
Jevnikar M et al (2015) Respiratory muscle training with enzyme replacement therapy improves muscle strength in late—onset Pompe disease. Mol Genet Metab Rep 5:67–71
Regnery C et al (2012) 36 months observational clinical study of 38 adult Pompe disease patients under alglucosidase alfa enzyme replacement therapy. J Inherit Metab Dis 35(5):837–845
Acknowledgements
We thank Vivisol Germany GmbH, Home Care Services, Neufahrn, Germany, for the free of charge provision of the IMT training devices Repsifit S®. We also want to thank the participants for their commitment and performance in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics committee of the Ludwig-Maximilians-University Munich, Germany (vote no. 689/16).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wenninger, S., Greckl, E., Babačić, H. et al. Safety and efficacy of short- and long-term inspiratory muscle training in late-onset Pompe disease (LOPD): a pilot study. J Neurol 266, 133–147 (2019). https://doi.org/10.1007/s00415-018-9112-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9112-4