Abstract
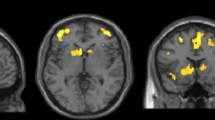
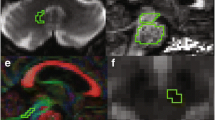
We evaluated MRI measures of gray and white matter damages in 19 patients with progressive supranuclear palsy (PSP), 11 with corticobasal syndrome (CBS), and 14 healthy subjects (HS) to differentiate patients with PSP from those with CBS. We calculated surface-based maps of the cortical volume, cortical thickness, surface area, and voxel level maps of sub-cortical volume, and diffusion tensor imaging parameters using automated scripts implemented in FreeSurfer and FSL toolboxes. No significant differences in cortical volume loss were observed between PSP and CBS. When cortical volume was divided into cortical thickness and surface area, cortical thickness in peri-rolandic brain regions was significantly smaller in CBS than in PSP patients, whereas surface area was significantly smaller in PSP than HS. We also found widespread volume loss in sub-cortical structures in patients with PSP and CBS in comparison to HS. Both patient groups displayed diffusion tensor imaging abnormalities: compared to HS, widespread fractional anisotropy and radial diffusivity changes were observed in PSP, whereas axial and radial diffusivity changes were prominent in CBS. Mini-mental state examination positively correlated with diffusion changes in patients with PSP. In conclusion, cortical thickness, surface area, and diffusion tensor imaging parameters may be sensitive enough to help differentiate patients with PSP from those with CBS.




Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer disease
- ANOVA:
-
Analysis of variance
- AxD:
-
Axial diffusivity
- CBS:
-
Corticobasal syndrome
- CTh:
-
Cortical thickness
- DSM IV-TR:
-
Diagnostic and statistical manual of mental disorders, fourth edition, text revision
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- FAB:
-
Frontal assessment battery
- FTLD:
-
Fronto-temporal lobar degeneration
- GLM:
-
General linear model
- GM:
-
Gray matter
- HAM-D:
-
Hamilton depression scale
- HS:
-
Healthy subjects
- MD:
-
Mean diffusivity
- MDS-UPDRS-III:
-
Movement disorder society-unified Parkinson’s disease rating scale, part III
- MMSE:
-
Mini-mental state evaluation
- PSP:
-
Progressive supranuclear palsy
- RD:
-
Radial diffusivity
- RS:
-
Richardson syndrome
- SA:
-
Surface area
- WM:
-
White matter
References
Josephs KA, Whitwell JL, Dickson DW et al (2008) Voxel-based morphometry in autopsy proven PSP and CBD. Neurobiol Aging 29:280–289
Steele JC, Richardson J, Olszewski J (1964) Progressive supranuclear palsy: a heterogeneous degeneration involving the brain stem, basal ganglia and cerebellum with vertical gaze and pseudobulbar palsy, nuchal dystonia and dementia. Arch Neurol 10:333–359
Colosimo C, Bak TH, Bologna M, Berardelli A (2014) Fifty years of progressive supranuclear palsy. J Neurol Neurosurg Psychiatry 85:938–944
Respondek G, Höglinger GU (2016) The phenotypic spectrum of progressive supranuclear palsy. Parkinsonism Relat Disord 22(Suppl 1):S34–S36
Armstrong MJ, Litvan I, Lang AE et al (2013) Criteria for the diagnosis of corticobasal degeneration. Neurology 80:496–503
Burrell JR, Hodges JR, Rowe JB (2014) Cognition in corticobasal syndrome and progressive supranuclear palsy: a review. Mov Disord Off J Mov Disord Soc 29:684–693
Tsuboi Y, Josephs KA, Boeve BF et al (2005) Increased tau burden in the cortices of progressive supranuclear palsy presenting with corticobasal syndrome. Mov Disord Off J Mov Disord Soc 20:982–988
Ling H, Ling H, de Silva R et al (2014) Characteristics of progressive supranuclear palsy presenting with corticobasal syndrome: a cortical variant. Neuropathol Appl Neurobiol 40:149–163
Tosun D, Duchesne S, Rolland Y et al (2007) 3-D analysis of cortical morphometry in differential diagnosis of Parkinson’s plus syndromes: mapping frontal lobe cortical atrophy in progressive supranuclear palsy patients. Med Image Comput Comput-Assist Interv MICCAI Int Conf Med Image Comput Comput Assist Interv 10:891–899
Worker A, Blain C, Jarosz J et al (2014) Cortical thickness, surface area and volume measures in Parkinson’s disease, multiple system atrophy and progressive supranuclear palsy. PLoS One 9:e114167
Dąbrowska M, Schinwelski M, Sitek EJ et al (2015) The role of neuroimaging in the diagnosis of the atypical parkinsonian syndromes in clinical practice. Neurol Neurochir Pol 49:421–431
Ashburner J, Friston KJ (2000) Voxel-based morphometry—the methods. NeuroImage 11:805–821
Whitwell JL, Jack CR, Boeve BF et al (2010) Imaging correlates of pathology in corticobasal syndrome. Neurology 75:1879–1887
Yu F, Barron DS, Tantiwongkosi B, Fox P (2015) Patterns of gray matter atrophy in atypical parkinsonism syndromes: a VBM meta-analysis. Brain Behav 5:e00329
Bologna M, Piattella MC, Upadhyay N et al (2016) Neuroimaging correlates of blinking abnormalities in patients with progressive supranuclear palsy. Mov Disord Off J Mov Disord Soc 31:138–143
Hutton C, Draganski B, Ashburner J, Weiskopf N (2009) A comparison between voxel-based cortical thickness and voxel-based morphometry in normal aging. NeuroImage 48:371–380
Kim GH, Jeon S, Seo SW et al (2012) Topography of cortical thinning areas associated with hippocampal atrophy (HA) in patients with Alzheimer’s disease (AD). Arch Gerontol Geriatr 54:e122–e129
Van Essen DC (1997) A tension-based theory of morphogenesis and compact wiring in the central nervous system. Nature 385:313–318
Upadhyay N, Suppa A, Piattella MC et al (2016) Gray and white matter structural changes in corticobasal syndrome. Neurobiol Aging 37:82–90
Rizzo G, Martinelli P, Manners D et al (2008) Diffusion-weighted brain imaging study of patients with clinical diagnosis of corticobasal degeneration, progressive supranuclear palsy and Parkinson’s disease. Brain J Neurol 131:2690–2700
Erbetta A, Mandelli ML, Savoiardo M et al (2009) Diffusion tensor imaging shows different topographic involvement of the thalamus in progressive supranuclear palsy and corticobasal degeneration. AJNR Am J Neuroradiol 30:1482–1487
Lodi R (2009) Diffusion-weighted brain imaging study of patients with clinical diagnosis of corticobasal degeneration, progressive supranuclear palsy and Parkinson’s disease. Brain J Neurol 132:e130
Whitwell JL, Schwarz CG, Reid RI et al (2014) Diffusion tensor imaging comparison of progressive supranuclear palsy and corticobasal syndromes. Parkinsonism Relat Disord 20:493–498
Piattella MC, Upadhyay N, Bologna M et al (2015) Neuroimaging evidence of gray and white matter damage and clinical correlates in progressive supranuclear palsy. J Neurol 262:1850–1858
Litvan I, Agid Y, Calne D et al (1996) Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele–Richardson–Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 47:1–9
Angelo Antonini GA (2012) Validation of the Italian version of the Movement Disorder Society-Unified Parkinson’s disease rating scale. Neurol Sci 34:683–690
Golbe LI, Ohman-Strickland PA (2007) A clinical rating scale for progressive supranuclear palsy. Brain 130:1552–1565
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: a frontal assessment battery at bedside. Neurology 55:1621–1626
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6:278–296
Fischl B, Salat DH, Busa E et al (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341–355
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage 9:179–194
Fischl B (2012) FreeSurfer. NeuroImage 62:774–781
Smith SM, Jenkinson M, Johansen-Berg H et al (2006) Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. NeuroImage 31:1487–1505
Smith SM, Nichols TE (2009) Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44:83–98
Barnes J, Ridgway GR, Bartlett J et al (2010) Head size, age and gender adjustment in MRI studies: a necessary nuisance? NeuroImage 53:1244–1255
Kouri N, Murray ME, Hassan A et al (2011) Neuropathological features of corticobasal degeneration presenting as corticobasal syndrome or Richardson syndrome. Brain J Neurol 134:3264–3275
Dickson DW, Bergeron C, Chin SS et al (2002) Office of rare diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 61:935–946
Verstaen A, Eckart JA, Muhtadie L et al (2016) Insular atrophy and diminished disgust reactivity. Emotion (PMID 27148847)
Shi HC, Zhong JG, Pan PL et al (2013) Gray matter atrophy in progressive supranuclear palsy: meta-analysis of voxel-based morphometry studies. Neurol Sci 34:1049–1055
Gerstenecker A, Mast B, Duff K et al (2013) Executive dysfunction is the primary cognitive impairment in progressive supranuclear palsy. Arch Clin Neuropsychol Off J Natl Acad Neuropsychol 28:104–113
Song S-K, Sun S-W, Ju W-K et al (2003) Diffusion tensor imaging detects and differentiates axon and myelin degeneration in mouse optic nerve after retinal ischemia. NeuroImage 20:1714–1722
Höglinger GU, Melhem NM, Dickson DW et al (2011) Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat Genet 43:699–705
Agosta F, Galantucci S, Svetel M et al (2014) Clinical, cognitive, and behavioural correlates of white matter damage in progressive supranuclear palsy. J Neurol 261:913–924
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
The study was approved by our institutional review board and conformed with the Declaration of Helsinki. All participants gave their written informed consent.
Rights and permissions
About this article
Cite this article
Upadhyay, N., Suppa, A., Piattella, M.C. et al. MRI gray and white matter measures in progressive supranuclear palsy and corticobasal syndrome. J Neurol 263, 2022–2031 (2016). https://doi.org/10.1007/s00415-016-8224-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8224-y
Keywords
Profiles
- Neeraj Upadhyay View author profile
- Antonio Suppa View author profile