Abstract
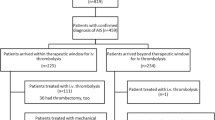
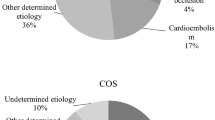
Despite the potential immediate access to diagnosis and care, in-hospital stroke (IHS) is associated with delay in diagnosis, lower rates of reperfusion treatment, and unfavorable outcome. Endovascular reperfusion therapy has shown promising results in recent trials for community-onset strokes (COS) and is limited by less contraindications than systemic thrombolysis. Thus, endovascular approaches may offer additional acute treatment options for IHS. We performed a retrospective, observational monocentric analysis of patients with acute ischemic stroke between January 2010 and December 2014. Out of 3506 acute ischemic strokes, 331 (9.4 %) were IHS. In-hospital mortality (31.4 vs. 8.0 %) and duration of stay after stroke (19.5 vs. 12.1 days) were higher in IHS than in COS. Most IHS occurred in cardiologic and cardiosurgical patients after catheterization or surgery. In 111 cases (33.5 %) the time of onset could not be established as a result of sedation or delayed referral resulting in delayed symptom recognition. 52 IHS (15.7 %) and 828 COS (26.0 %, p < 0.001) patients received any kind of reperfusion therapy, of which 59.6 % (IHS) and 12.1 % (COS) comprised isolated endovascular interventions (p < 0.001). Intra-hospital delays (time to brain imaging, systemic thrombolysis, and angiography) were longer and outcome parameters (mRS d90, in-hospital mortality, length of stay) were worse in IHS, whereas rates of procedural complications and intracranial hemorrhages were similar in both groups. The overall rate of reperfusion treatment is lower in IHS compared to COS, as IHS patients are less likely to be eligible for systemic thrombolysis. Interventional stroke treatment is a safe and feasible therapeutic option for patients who are not eligible for systemic thrombolysis and should be anticipated whenever IHS is diagnosed.

Similar content being viewed by others
References
Cumbler E, Wald H, Bhatt DL et al (2014) Quality of care and outcomes for in-hospital ischemic stroke:findings from the National Get With The Guidelines-Stroke. Stroke 45(1):231–238. doi:10.1161/STROKEAHA.113.003617
Dulli D, Samaniego EA (2007) Inpatient and community ischemic strokes in a university hospital. Neuroepidemiology 28(2):86–92. doi:10.1159/000098551
Saltman AP, Silver FL, Fang J et al (2015) Care and outcomes of patients with in-hospital stroke. JAMA Neurol. doi:10.1001/jamaneurol.2015.0284
The ATLANTIS, ECASS, and NINDS rt-PA Study Group Investigators (2004) Association of outcome with early stroke treatment:pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. The Lancet 363(9411):768–774. doi:10.1016/S0140-6736(04)15692-4
Manawadu D, Choyi J, Kalra L (2014) The impact of early specialist management on outcomes of patients with in-hospital stroke. PLoS ONE 9(8):e104758. doi:10.1371/journal.pone.0104758
Alvaro LC, Timiraos J, Sadaba F (2008) In-hospital stroke:clinical profile and expectations for treatment (Accidentes cerebrovasculares intrahospitalarios:perfil clinico y expectativas terapeuticas). Neurologia 23(1):4–9
Frank B, Grotta JC, Alexandrov AV et al (2013) Thrombolysis in stroke despite contraindications or warnings? Stroke 44(3):727–733. doi:10.1161/STROKEAHA.112.674622
Sacks D, Black CM, Cognard C et al (2013) Multisociety Consensus Quality Improvement Guidelines for Intraarterial Catheter-directed Treatment of Acute Ischemic Stroke, from the American Society of Neuroradiology, Canadian Interventional Radiology Association, Cardiovascular and Interventional Radiological Society of Europe, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, European Society of Minimally Invasive Neurological Therapy, and Society of Vascular and Interventional Neurology. AJNR Am J Neuroradiol 34(4):E0
Berkhemer OA, Fransen, Puck SS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372(1):11–20. doi:10.1056/NEJMoa1411587
Goyal M, Demchuk AM, Menon BK et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030. doi:10.1056/NEJMoa1414905
Campbell Bruce C V, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372(11):1009–1018. doi:10.1056/NEJMoa1414792
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372(24):2285–2295. doi:10.1056/NEJMoa1415061
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372(24):2296–2306. doi:10.1056/NEJMoa1503780
Brott T, Adams HP, Olinger CP et al (1989) Measurements of acute cerebral infarction:a clinical examination scale. Stroke 20(7):864–870. doi:10.1161/01.STR.20.7.864
van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607. doi:10.1161/01.STR.19.5.604
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24(1):35–41. doi:10.1161/01.STR.24.1.35
Bruno A, Akinwuntan AE, Lin C et al (2011) Simplified modified rankin scale questionnaire:reproducibility over the telephone and validation with quality of life. Stroke 42(8):2276–2279. doi:10.1161/STROKEAHA.111.613273
Larrue V, von Kummer R, Muller A et al (2001) Risk Factors for Severe Hemorrhagic Transformation in Ischemic Stroke Patients Treated With Recombinant Tissue Plasminogen Activator: a Secondary Analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32(2):438–441. doi:10.1161/01.STR.32.2.438
Kelley RE, Kovacs AG (1986) Mechanism of in-hospital cerebral ischemia. Stroke 17(3):430–433. doi:10.1161/01.STR.17.3.430
Lerner DJ, Kannel WB (1986) Patterns of coronary heart disease morbidity and mortality in the sexes:a 26-year follow-up of the Framingham population. Am Heart J 111(2):383–390
Towfighi A, Zheng L, Ovbiagele B (2009) Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med 169(19):1762–1766. doi:10.1001/archinternmed.2009.318
Jauch EC, Saver JL, Adams HP et al (2013) Guidelines for the early management of patients with acute ischemic stroke:a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44(3):870–947
Rodríguez Campello A, Cuadrado Godia E, Giralt Steinhauer E et al (2014) Detección de ictus intrahospitalario:evaluación de resultados de un programa de formación y entrenamiento a personal médico y de enfermería (Detecting in-hospital stroke: Assessment of results from a training programme for medical personnel). Neurologia. doi:10.1016/j.nrl.2014.06.003
Cumbler E, Zaemisch R, Graves A et al (2012) Improving stroke alert response time:applying quality improvement methodology to the inpatient neurologic emergency. J Hosp Med 7(2):137–141
Cumbler E, Anderson T, Neumann R et al (2010) Stroke alert program improves recognition and evaluation time of in-hospital ischemic stroke. J Stroke Cerebrovasc Dis 19(6):494–496. doi:10.1016/j.jstrokecerebrovasdis.2009.09.007
Hamon M, Baron J, Viader F et al (2008) Periprocedural stroke and cardiac catheterization. Circulation 118(6):678–683. doi:10.1161/CIRCULATIONAHA.108.784504
Ballotta E, Saladini M, Gruppo M et al (2010) Predictors of electroencephalographic changes needing shunting during carotid endarterectomy. Ann Vasc Surg 24(8):1045–1052. doi:10.1016/j.avsg.2010.06.005
Wang X, Ji B, Yang B et al (2012) Real-time continuous neuromonitoring combines transcranial cerebral Doppler with near-infrared spectroscopy cerebral oxygen saturation during total aortic arch replacement procedure:a pilot study. ASAIO J 58(2):122–126. doi:10.1097/MAT.0b013e318241abd3
Herman ST, Abend NS, Bleck TP et al (2015) Consensus statement on continuous EEG in critically ill adults and children, part I:indications. J Clin Neurophysiol 32(2):87–95. doi:10.1097/WNP.0000000000000166
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. M. Wiesmann reports grants and personal fees from Stryker Neurovascular, grants and personal fees from SilkRoad Medical, Grants from Covidien, grants from Microvention, grants and personal fees from Bracco, grants and personal fees from Siemens, grants from AB Medica, grants from Acandis, grants from Codman Neurovascular, grants from Penumbra, Grants from Phenox, grants from Abbott, grants from St. Jude, from B. Braun, outside the submitted work. All other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schürmann, K., Nikoubashman, O., Falkenburger, B. et al. Risk profile and treatment options of acute ischemic in-hospital stroke. J Neurol 263, 550–557 (2016). https://doi.org/10.1007/s00415-015-8010-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-8010-2