Abstract
Delayed cerebral ischemia (DCI) is an important cause of poor outcome after aneurysmal subarachnoid hemorrhage (SAH). We studied differences in incidence and impact of DCI as defined clinically after coiling and after clipping in the International Subarachnoid Aneurysm Trial. We calculated odds ratios (OR) for DCI for clipping versus coiling with logistic regression analysis. With coiled patients without DCI as the reference group, we calculated ORs for poor outcome at 2 months and 1 year for coiled patients with DCI and for clipped patients without, and with DCI. With these ORs, we calculated relative excess risk due to Interaction (RERI). Clipping increased the risk of DCI compared to coiling in the 2,143 patients OR 1.24, 95% confidence interval (95% CI 1.01–1.51). Coiled patients with DCI, clipped patients without DCI, and clipped patients with DCI all had higher risks of poor outcome than coiled patients without DCI. Clipping and DCI showed no interaction for poor outcome at 2 months: RERI 0.12 (95% CI −1.16 to 1.40) or 1 year: RERI −0.48 (95% CI −1.69 to 0.74). Only for patients treated within 4 days, coiling and DCI was associated with a poorer outcome at 1 year than clipping and DCI (RERI −2.02, 95% CI −3.97 to −0.08). DCI was more common after clipping than after coiling in SAH patients in ISAT. Impact of DCI on poor outcome did not differ between clipped and coiled patients, except for patients treated within 4 days, in whom DCI resulted more often in poor outcome after coiling than after clipping.
Similar content being viewed by others
Background
Aneurysmal subarachnoid hemorrhage still has a poor prognosis: one out of three patients die and one out of five remain dependent for activities of daily life [1]. Delayed cerebral ischemia (DCI) occurs in about one-third to a quarter of the patients and is an important cause of poor outcome after SAH [2]. DCI carries considerable consequences in terms of costs and resumption of employment [3]. Important risk factors for the occurrence of DCI are poor clinical condition at admission, and the amount of blood on the initial CT scan [4].
After aneurysmal SAH, the aneurysm can be occluded endovascularly by coiling or neurosurgically by clipping. The International Subarachnoid Aneurysm Trial (ISAT) has shown that if both treatment options are possible, coiling results in a better clinical outcome than clipping [5]. As DCI is an important determinant of poor outcome, differences in incidence or impact of DCI could partly explain the difference in outcome after clipping and after coiling.
Currently, there are no reliable data on differences in occurrence and impact of DCI after clipping and after coiling. Expert opinions differ largely. Some authors describe that during neurosurgical clipping, the blood clot (and thereby spasmogenic agents) can be removed from the subarachnoid space, which would diminish the risk of symptomatic vasospasm and DCI [6, 7]. Others believe that manipulation of the brain and abluminal vessel walls during surgery increases the risk of vasospasm and DCI [8], when compared to the risk of DCI after coiling.
To determine whether there is a difference in occurrence and impact of DCI after SAH in patients treated by endovascular coiling and those treated with neurosurgical clipping, we studied incidence and impact of DCI as defined clinically after coiling and after clipping in a large randomized controlled trial (ISAT trial) [5].
Methods
Patients
We analyzed the data of patients who had participated in the ISAT trial, a clinical trial that randomized 2,143 patients to either endovascular coiling or neurosurgical clipping of the ruptured aneurysm. The methods of this trial have been described previously [5]. In short, patients were included in the trial if they had a definite subarachnoid hemorrhage within the last 28 days and a demonstrated aneurysm. The aneurysm was judged by both the neurosurgeon and the neuroradiologist to be suitable for treatment, but there was uncertainty regarding which treatment was preferred, and informed consent was obtained. The majority of included patients were in a good clinical condition at admission.
Of the included patients, age, sex, clinical grade on the World Federation of Neurosurgical Surgeons (WFNS) grading scale [9], amount of extravasated blood on the initial CT according to the Fisher scale [10], and the occurrence of DCI was recorded. Age was dichotomized into lower or higher than 55 years. The WFNS scale was dichotomized into good clinical condition (WFNS 1–3) or poor clinical condition (WFNS 4–5). The Fisher scale was dichotomized into Fisher 1–2 and Fisher 3–4. DCI was a clinical diagnosis made by the treating physician. In the ISAT manual, the following definition was given for DCI: clinical grounds of delayed ischemic neurological deficit, not due to operative factors or other factors such as procedural vessel occlusion, hydrocephalus or aneurysmal re-bleeding, and by the clinicians judged to be due to “vasospasm”. The day of DCI or results of imaging studies were not recorded. Clinical outcome was assessed by self-reported questionnaires with the modified Rankin (mRS) score at 2 months and at 1 year [11]. Poor outcome was defined as an mRS of 3 or higher.
Data analysis
To compare the occurrence of DCI after clipping with that after coiling, we calculated the odds ratio (OR) with corresponding 95% confidence interval (95% CI) with logistic regression analysis.
To study whether the impact of DCI on poor outcome is different in clipped patients than in coiled patients, we first calculated ORs with 95% CI for the occurrence of poor outcome for three different groups of patients: coiled patients with DCI, clipped patients without DCI, and clipped patients with DCI, compared to the reference group consisting of coiled patients without DCI. To study whether there was an interaction between treatment modality and the occurrence of DCI, we calculated the “relative excess risk due to interaction (RERI)”, with 95% CI [12]. The RERI is calculated as OR++ − OR+− − OR−+ + 1, with OR++ the odds of clipping and DCI, OR+− that of clipping and no DCI, and OR−+ that of coiling and DCI. If the RERI is >0, this means there is attributive risk of the combination of clipping and DCI; if the RERI is <0, this means an attributive risk for the combination of coiling and DCI.
Because DCI mostly occurs between the 4th and 10th day after the SAH, we performed a sensitivity analysis for the subgroup of patients treated within 4 days after the SAH. All analyses were adjusted for age, sex, clinical condition, and amount of extravasated blood only if they altered the crude OR with more than 5% in bivariate analysis. In all analyses, variables were introduced dichotomously and patients were analyzed according to their original treatment allocation.
Results
Treatment modality and occurrence of DCI
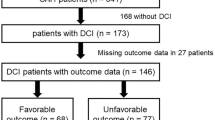
Table 1 shows the baseline characteristics of the 2,143 included patients. Of the 1,070 patients allocated to clipping, data on presence or absence of DCI were known for 1,066 (99.6%) patients. DCI had occurred in 283 (27%) of these patients. Of the 1,073 patients allocated to coiling, data on presence or absence of DCI were known for 1,069 (99.6%). DCI had occurred in 241 (23%) of these patients (Fig. 1). Of the cross-overs, DCI occurred in two of the eight patients (25%) originally allocated to coiling and in 12 of the 39 patients (36%) originally allocated to clipping.
Clipping increased the risk of DCI compared with coiling: OR 1.24 (95% CI 1.01–1.51). The absolute risk difference was 4% (95% CI 0–8%). Adjustment for age, gender, clinical condition on admission, and amount of extravasated blood did not change the OR in bivariate analyses with more than 5%, so no multivariate analysis was performed. When only the 1,373 patients were analyzed who were treated before day 4, the OR for DCI for clipping versus coiling was 1.48 (95% CI 1.15–1.89) and the absolute risk difference 7% (95% CI 3–11%). Adjustment for baseline characteristics did not change the OR.
DCI and outcome in coiled and clipped patients
Data on DCI and outcome at 2 months were known for 1,057 (98.8%) of the clipped patients and for 1,059 (98.7%) of the coiled patients. Coiled patients with DCI, clipped patients without DCI, and clipped patients with DCI, all had a statistically significant higher chance of poor outcome at 2 months when compared to coiled patients without DCI (Table 2).
The RERI for interaction of clipping and DCI was 0.12 (95% CI −1.16 to 1.40) after adjustment for amount of extravasated blood. When only patients treated within 4 days were taken into account, the RERI was −0.19 (95% CI −1.99 to 1.60) after adjustment for age, clinical condition on admission, and amount of extravasated blood.
Data on DCI and outcome at 1 year were known for 1,051 (98.2%) of the clipped patients and for 1,060 (98.8%) of the coiled patients. When we repeated the analyses for the 1-year outcome, a similar pattern emerged (Table 3). The RERI was −0.48 (95% CI −1.69 to 0.74) after adjustment for age, clinical condition on admission, and amount of extravasated blood. When only patients treated within 4 days were taken into account, the adjusted RERI was −2.02 (95% CI −3.97 to −0.08), meaning a significant attributive risk of poor outcome for the combination of coiling and DCI than for the combination of clipping and DCI.
Discussion
This study shows that clinically defined DCI was more common after neurosurgical clipping than after endovascular coiling in SAH patients randomized between one of these treatments. The impact of DCI on poor outcome was not different after clipping than after coiling. The difference in occurrence of DCI between coiling and clipping can, at least partly, explain the difference in outcome between clipped and coiled patients. Our results strengthen the current practice of preference for coiling of a ruptured aneurysm above clipping, if the aneurysm is suitable for both treatment options.
By calculating the RERI for the interaction of clipping and DCI, we found no additional effect on poor outcome, meaning no difference of impact of DCI on outcome between clipping and coiling, except for the subgroup of patients treated within 4 days. In this subgroup, there was no difference of impact of DCI between clipping and coiling for outcome at 2 months, but at 1 year, DCI had a stronger impact on poor outcome after coiling than after clipping. We have two explanations for the results in this pre-specified subgroup analysis. Firstly, even though the study group and numbers of outcome events are very large in this study and the analysis was pre-planned, it can still be a chance finding. Secondly, the recovery from DCI after coiling may be worse than after clipping because of the high frequency of small ischemic lesions after coiling of aneurysms [13, 14]. These lesions may enlarge the affected areas and slow down the clinical recovery.
Several studies have tried to assess the difference in the incidence of DCI between clipping and coiling. One meta-analysis, including nine studies, showed a trend towards less symptomatic vasospasm after coiling than after clipping [15]. However, the included studies had methodological weaknesses. All but one study were non-randomized, and the decision of which technique of aneurysm treatment was used was made on the basis of patient characteristics. As a result, the two treatment groups were not comparable: patients who were treated by coiling were older, more often had a poor clinical prognosis, and were more likely to have an aneurysm in the posterior circulation. Incidence and impact of DCI of these patients can therefore not be attributed to aneurysm treatment modality alone, but was most likely influenced by differences in baseline characteristics between the two patient groups. One published RCT reported more ischemic deficits on MRI at 12 months after treatment in the neurosurgical treated group, but did not report on clinical aspects of DCI [16].
Strong points of our study are that we used data from a large randomized controlled trial where patients were randomized between neurosurgical or endovascular treatment. This enabled us to study differences in DCI between clipped and coiled patients independent of confounding factors. Moreover, we had a very high percentage of follow-up. This makes it highly likely that the differences we found in the occurrence of DCI are really due to the treatment modality.
An important drawback of this study is that the diagnosis of DCI is difficult. We used a clinical definition of DCI and did not take into account angiographic vasospasm or ischemic lesions on CT scan, because unfortunately these data were not recorded in the ISAT. The final diagnosis was left to the discretion of the treating physician. These physicians were not blinded to the allocated treatment. In clipped patients, surgery-related damage might have been diagnosed as DCI, and might have led to differences in diagnosing DCI between different physicians and different hospitals. However, the definition of DCI was clearly described in the ISAT manual and excluded procedural ischemia and should have led to more uniformity. Moreover, as randomization was stratified per hospital, different interpretation of the diagnosis of DCI per hospital should not have led to a bias. Treatment of DCI was also left to the treating physician, but because of randomization stratified per hospital, we think that it is unlikely that DCI will have been treated differently in clipped than in coiled patients. Also, the confidence interval for the risk of DCI for clipping compared with coiling was close to one OR 1.24 (95% CI 1.01–1.51).
Another weak point is that the day of DCI was not recorded. Some patients will have been treated with either coiling or clipping after the DCI episode, and therefore the treatment modality cannot have been an influencing factor. The median day of treatment was on day three after the SAH. For this reason, we performed a sensitivity analysis of all patients who were treated before day four, because mostly, DCI does not occur before day four [8]. These analyses showed even higher ORs for the risk of DCI after clipping compared to coiling, which strengthens the reliability of our results.
In conclusion, DCI was more common after neurosurgical clipping than after endovascular coiling in ISAT patients. DCI did not have more impact on poor outcome in clipped patients than in coiled patients, except for patients treated within 4 days, with an attributive risk of poor outcome at 1 year for the combination coiling and DCI.
References
Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ (2009) Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol 8:635–642
Roos YB, de Haan RJ, Beenen LF, Groen RJ, Albrecht KW, Vermeulen M (2000) Complications and outcome in patients with aneurysmal subarachnoid haemorrhage: a prospective hospital based cohort study in the Netherlands. J Neurol Neurosurg Psychiatry 68:337–341
Rivero-Arias O, Wolstenholme J, Gray A, Molyneux AJ, Kerr RS, Yarnold JA, Sneade M (2009) The costs and prognostic characteristics of ischaemic neurological deficit due to subarachnoid haemorrhage in the United Kingdom: evidence from the MRC International Subarachnoid Aneurysm Trial. J Neurol 79:373–378
Brouwers PJ, Dippel DW, Vermeulen M, Lindsay KW, Hasan D, van Gijn J (1993) Amount of blood on computed tomography as an independent predictor after aneurysm rupture. Stroke 24:809–814
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2,143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274
Taneda M (1982) The significance of early operation in the management of ruptured intracranial aneurysms—an analysis of 251 cases hospitalized within 24 hours after subarachnoid haemorrhage. Acta Neurochir (Wien) 63:201–208
Mizukami M, Kawase T, Usami T, Tazawa T (1982) Prevention of vasospasm by early operation with removal of subarachnoid blood. Neurosurgery 10:301–307
Brilstra EH, Rinkel GJ, Algra A, van Gijn J (2000) Rebleeding, secondary ischemia, and timing of operation in patients with subarachnoid hemorrhage. Neurology 55:1656–1660
(1988) Report of World Federation of Neurological Surgeons Committee on a Universal Subarachnoid Hemorrhage Grading Scale. J Neurosurg 68:985–986
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Hosmer DW, Lemeshow S (1992) Confidence interval estimation of interaction. Epidemiology 3:452–456
Cronqvist M, Wirestam R, Ramgren B, Brandt L, Nilsson O, Saveland H, Holtas S, Larsson EM (2005) Diffusion and perfusion MRI in patients with ruptured and unruptured intracranial aneurysms treated by endovascular coiling: complications, procedural results, MR findings and clinical outcome. Neuroradiology 47:855–873
Soeda A, Sakai N, Murao K, Sakai H, Ihara K, Yamada N, Imakita S, Nagata I (2003) Thromboembolic events associated with Guglielmi detachable coil embolization with use of diffusion-weighted MR imaging. Part II. detection of the microemboli proximal to cerebral aneurysm. AJNR Am J Neuroradiol 24:2035–2038
de Oliveira JG, Beck J, Ulrich C, Rathert J, Raabe A, Seifert V (2007) Comparison between clipping and coiling on the incidence of cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurg Rev 30:22–30
Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M (2000) Outcomes of early endovascular versus surgical treatment of ruptured cerebral aneurysms. A prospective randomized study. Stroke 31:2369–2377
Acknowledgments
This study was partly sponsored by the Netherlands Heart Foundation, Grant number 2005016.
Conflict of interest
The authors declare that they have no disclosures.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dorhout Mees, S.M., Kerr, R.S., Rinkel, G.J.E. et al. Occurrence and impact of delayed cerebral ischemia after coiling and after clipping in the International Subarachnoid Aneurysm Trial (ISAT). J Neurol 259, 679–683 (2012). https://doi.org/10.1007/s00415-011-6243-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6243-2