Abstract
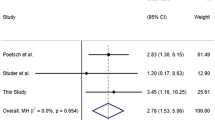
Unclassified sudden infant death (USID) is the sudden and unexpected death of an infant that remains unexplained after thorough case investigation including performance of a complete autopsy and review of the circumstances of death and the clinical history. When the infant is below 1 year of age and with onset of the fatal episode apparently occurring during sleep, this is referred to as sudden infant death syndrome (SIDS). USID and SIDS remain poorly understood despite the identification of several environmental and some genetic risk factors. In this study, we investigated genetic risk factors involved in the autonomous nervous system in 195 Dutch USID/SIDS cases and 846 Dutch, age-matched healthy controls. Twenty-five DNA variants from 11 genes previously implicated in the serotonin household or in the congenital central hypoventilation syndrome, of which some have been associated with SIDS before, were tested. Of all DNA variants considered, only the length variation of the polyalanine repeat in exon 3 of the PHOX2B gene was found to be statistically significantly associated with USID/SIDS in the Dutch population after multiple test correction. Interestingly, our data suggest that contraction of the PHOX2B exon 3 polyalanine repeat that we found in six of 160 SIDS and USID cases and in six of 814 controls serves as a probable genetic risk factor for USID/SIDS at least in the Dutch population. Future studies are needed to confirm this finding and to understand the functional effect of the polyalanine repeat length variation, in particular contraction, in exon 3 of the PHOX2B gene.
Similar content being viewed by others
References
Krous HF, Beckwith JB, Byard RW et al (2004) Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics 114:234–238
Centraal bureau voor statistiek (2012) www.cbs.nl. Accessed Dec 2012
American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome (2011) SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics 128(5):e1341–e1367. doi:10.1542/peds.2011-2285
Engelberts AC, de Jonge GA (1988) Sleeping position and cot death. Lancet 2(8616):899–900
Liebrechts-Akkerman G, Lao O, Liu F et al (2011) Postnatal parental smoking: an important risk factor for SIDS. Eur J Pediatr 170(10):1281–91. doi:10.1007/s00431-011-1433-6
Opdal SH, Rognum TO (2004) The sudden infant death syndrome gene: does it exist? Pediatrics 114(4):e506–12
Rand CM, Patwari PP, Carroll MS, Weese-Mayer DE (2013) Congenital central hypoventilation syndrome and sudden infant death syndrome: disorders of autonomic regulation. Semin Pediatr Neurol 20(1):44–55. doi:10.1016/j.spen.2013.01.005
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Rand CM (2008) Congenital central hypoventilation syndrome (CCHS) and sudden infant death syndrome (SIDS): kindred disorders. Respir Physiol Neurobiol 164(1–2):38–48
Amiel J, Laudier B, Attié-Bitach T et al (2003) Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Gen 33:459–461
Weese-Mayer DE, Berry-Kravis EM, Zhou L et al (2003) Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2B. Am J Med Genet A 123A:267–78
Gaultier C, Amiel J, Dauger S et al (2004) Genetics and early disturbance in breathing control. Ped res 55(5):729–33
Amiel J, Salomon R, Attie R et al (1998) Mutations of the RET-GDNF signaling pathway in Odine’s curse. Am J Hum Genet 62:715–7
Weese-Mayer DE, Berry-Kravis EM, Zhou L et al (2004) Sudden infant death syndrome: case–control frequency differences at gene pertinent to early autonomic nervous system embryologic development. Pediatr Res 56(3):391–5
Weese-Mayer DE, Berry-Kravis EM, Maher BS et al (2003) Sudden infant death syndrome: association with a promotor polymorphism of the serotonin transporter gene. Am J Med Genet A 117A:268–74
Weese-Mayer DE, Zhou L, Berry-Kravis EM et al (2003) Association of serotonin transporter gene with sudden infant death syndrome: a haplotype analysis. Am J Med Genet A 122A:238–45
Narita N, Narita M, Takashima S et al (2001) Serotonin transporter gene variation is a risk factor for sudden infant death syndrome in Japanese population. Pediatrics 107:690–2
Opdal SH, Vege A, Rognum TO (2008) Serotonin transporter gene variation in sudden infant death syndrome. Acta Paediatr 97(7):861–5
Nonnis Marzano F, Maldini M, Filonzi L et al (2008) Genes regulating the serotonin metabolic pathway in the brain stem and their role in the etiopathogenesis of sudden infant death syndrome. Genomics 91(6):485–91
Haas C, Braun J, Bar W, Bartsch C (2009) No association of serotonin transporter gene variation with sudden infant death syndrome (SIDS) in Caucasians. Leg Med (Tokyo). doi:10.1016/j.legalmed.2009.01.051
Paterson DS, Trachtenberg FL, Thompson EG et al (2006) Multiple serotonergic brainstem abnormalities in sudden infant death syndrome. JAMA 296(17):2124–2144
Liebrechts-Akkerman G, de Jonge GA, Bovee JVMG et al (2013) Histological findings in unclassified sudden infant death, including sudden infant death syndrome. Pediatr Dev Pathol 16(3):168–76. doi:10.2350/12-10-1262-OA.1
Jaddoe VW, van Duijn CM, Franco OH et al (2012) The Generation R Study: design and cohort update 2012. Eur J Epidemiol 27(9):739–56. doi:10.1007/s10654-012-9735-1
Sullivan KM, Mannucci A, Kimpton CP, Gill P (1993) A rapid and quantitative DNA sex test: fluorescence-based PCR analysis of X-Y homologous gene amelogenin. Biotechniques 15(4):636–638, 640–1
www.hapmap.org. Accessed 2005
Curtin F, Schulz P (1998) Multiple correlations and Bonferroni’s correction. Biol Psychiatry 44(8):775–7
Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA (2002) Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet 70:425–434
Dubreuil V, Ramanantsoa N, Trochet D et al (2008) A human mutation in Phox2b causes lack of CO2 chemosensitivity, fetal central apnea, and specific loss of parafacial neurons. Proc Natl Aad Sci USA 105(3):1067–72
Lavezzi AM, Weese-Mayer DE, Yu MY et al (2012) Developmental alterations of the respiratory human retrotrapezoid nucleus in sudden unexplained fetal and infant death. Auton Neurosci 170(1–2):12–9. doi:10.1016/j.autneu.2012.06.005
Rand CM, Weese-Mayer DE, Zhou L et al (2006) Sudden infant death syndrome: case–control frequency differences in paired like homeobox (PHOX) 2B gene. Am J Med Genet A 140(15):1687–91
Kijima K, Sasaki A, Niki T et al (2004) Sudden infant death syndrome is not associated with the mutation of PHOX2B gene, a major causative gene of congenital central hypoventilation syndrome. Tohoku J Exp Med 203(1):65–8
Jennings LJ, Yu M, Rand CM et al (2012) Variable human phenotype associated with novel deletions of the PHOX2B gene. Pediatr Pulmonol 47(2):153–61. doi:10.1002/ppul.21527
Dauger S, Pattyn A, Lofaso F et al (2003) Phox2b controls the development of peripheral chemoreceptors and afferent visceral pathways. Development 130(26):6635–42
Durand E, Dauger S, Pattyn A et al (2005) Sleep-disordered breathing in newborn mice heterozygous for the transcription factor Phox2B. Am J Respir Crit Care Med 172:238–243
Klopfleisch R, Weiss AT, Gruber AD (2011) Excavation of a buried treasure—DNA, mRNA, miRNA and protein analysis in formalin fixed, paraffin embedded tissues. Histol Histopathol 26(6):797–810
Vallone PM, Butler JM (2004) Autodimer: a screening tool for primer-dimer and hairpin structures. Biotechniques 37(2):226–31
Acknowledgments
We are grateful to all participants of the study as well as to the LWW for having collected and provided relevant information. We thank the following colleagues for having provided tissue material and record information to this study: R.R. de Krijger, Erasmus Medisch Centrum, Rotterdam; J.V.M.G. Bovee, Leids Universitair Medisch Centrum, Leiden; L.C.D. Wijnaendts, Vrije Universiteit, Amsterdam; P.G.J. Nikkels, Academisch Ziekenhuis Utrecht, Utrecht; A.H. Mulder, Ziekenhuis Rijnstate, Arnhem; R. Boorsma, Laboratorium voor de Volksgezondheid Friesland, Leeuwarden; J.C. van der Linde, Jeroen Bosch Ziekenhuis, Den Bosch; P. Blok, Ziekenhuis Leyenburg, the Hague; C. van der Hulsbergen, Academisch Ziekenhuis Nijmegen St Radboud, Nijmegen; A. Timmer, Universitair Medisch Centrum Groningen, Groningen; S.J.F. Schoots, St. Samenwerkende Ziekenhuizen Oost Groningen, Wintschoten; F.J. ten Kate, Academisch Medisch Centrum, Amsterdam; A. Maes, Nederlands Forensisch Instituut, the Hague; P. Westenend, Pathologisch Laboratorium voor Dordrecht en Omstreken, Dordrecht; W.S. Kwee, St. Jansgasthuis and Laurentius Ziekenhuis, Roermond and Weert; D. Willebrand, Streeklaboratorium voor de Volksgezondheid, Haarlem; R.N. Breeuwsma, Medisch Centrum Alkmaar, Alkmaar; M. Brinkhuis, Laboratorium voor Pathologie Oost Nederland, Enschede; N. Vandevijver, Atrium, Heerlen; Nijhuis, Onze Lieve Vrouwe Gasthuis, Amsterdam; M. Baldewijns, Academisch Ziekenhuis Maastricht, Maastricht; C.M. van Dijk, Groene Hart Ziekenhuis, Gouda; E. de Ruijter, Amphia Ziekenhuis, Breda; J.A. Ruizeveld de Winter, Pathan, Rotterdam; I. van Lijnschoten, Stichting PAMM, Eindhoven; R.F.M. Schapers, St. Pathologisch Laboratorium Noord-Limburg, Venlo; C. Wauters, Canisius-Wilhelmina Ziekenhuis, Nijmegen; C.A. Seldenrijk, St. Antonius Ziekenhuis, Nieuwegein; E.C.M. Ooms, Haaglanden, the Hague; H. Beerman, Medisch Centrum Rotterdam Zuid, Rotterdam; J.G. Smits, Streeklaboratorium Zeeland, Middelburg; R. Dutrieux, Zaans Medisch Centrum, Zaandam; A.M. Croonen, Lab Klinische Pathologie Centraal Brabant, Tilburg; E.M. van der Loo, Reinier de Graafziekenhuis, Delft; J.W. Arends, Deventer Ziekenhuizen, Deventer; and W.A. van Houten, Laboratorium voor Pathologie St. Sazinon, Hoogeveen. We also like to thank Arwin Ralf, Kaye Ballantyne and Ying Choi for their support in DNA analyses. This study was supported by the Erasmus University Medical Center Rotterdam and in part by funding provided by the Netherlands Forensic Institute. The Generation R Study gratefully acknowledges the contribution of children and parents, general practitioners, hospitals, midwives and pharmacies in Rotterdam. The Generation R Study is made possible by financial support from the Erasmus Medical Center, Rotterdam, the Erasmus University Rotterdam, the Netherlands Organization for Health Research and Development (ZonMw), the Netherlands Organisation for Scientific Research (NWO), the Ministry of Health, Welfare and Sport of the Netherlands.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 120 kb)
Rights and permissions
About this article
Cite this article
Liebrechts-Akkerman, G., Liu, F., Lao, O. et al. PHOX2B polyalanine repeat length is associated with sudden infant death syndrome and unclassified sudden infant death in the Dutch population. Int J Legal Med 128, 621–629 (2014). https://doi.org/10.1007/s00414-013-0962-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-013-0962-0