Abstract
Purpose
We compared respiratory mechanics between the positive end-expiratory pressure of minimal respiratory system elastance (PEEPminErs) and three levels of PEEP during low-tidal-volume (6 mL/kg) ventilation in rats.
Methods
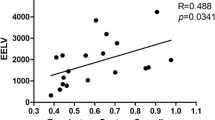
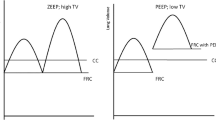
Twenty-four rats were anesthetized, paralyzed, and mechanically ventilated. Airway pressure (Paw), flow (F), and volume (V) were fitted by a linear single compartment model (LSCM) Paw(t) = Ers × V(t) + Rrs × F(t) + PEEP or a volume- and flow-dependent SCM (VFDSCM) Paw(t) = (E1 + E2 × V(t)) × V(t) + (K1 + K2 × |F(t)|) × F(t) + PEEP, where Ers and Rrs are respiratory system elastance and resistance, respectively; E1 and E2× V are volume-independent and volume-dependent Ers, respectively; and K1 and K2 × F are flow-independent and flow-dependent Rrs, respectively. Animals were ventilated for 1 h at PEEP 0 cmH2O (ZEEP); PEEPminErs; 2 cmH2O above PEEPminErs (PEEPminErs+2); or 4 cmH2O above PEEPminErs (PEEPminErs+4). Alveolar tidal recruitment/derecruitment and overdistension were assessed by the index %E2 = 100 × [(E2 × VT)/(E1 + |E2| × VT)], and alveolar stability by the slope of Ers(t).
Results
%E2 varied between 0 and 30% at PEEPminErs in most respiratory cycles. Alveolar Tidal recruitment/derecruitment (%E2 < 0) and overdistension (%E2 > 30) were predominant in the absence of PEEP and in PEEP levels higher than PEEPminErs, respectively. The slope of Ers(t) was different from zero in all groups besides PEEPminErs+4.
Conclusions
PEEPminErs presented the best compromise between alveolar tidal recruitment/derecruitment and overdistension, during 1 h of low-VT mechanical ventilation.




Similar content being viewed by others
References
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31(10):1327–1335. https://doi.org/10.1007/s00134-005-2761-7
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28(5):596–608. https://doi.org/10.1152/jappl.1970.28.5.596
Bregeon F, Roch A, Delpierre S, Ghigo E, Autillo-Touati A, Kajikawa O, Martin TR, Pugin J, Portugal H, Auffray JP, Jammes Y (2002) Conventional mechanical ventilation of healthy lungs induced pro-inflammatory cytokine gene transcription. Respir Physiol Neurobiol 132(2):191–203
dos Santos CC, Slutsky AS (2006) The contribution of biophysical lung injury to the development of biotrauma. Annu Rev Physiol 68:585–618. https://doi.org/10.1146/annurev.physiol.68.072304.113443
Michelet P, D’Journo XB, Roch A, Doddoli C, Marin V, Papazian L, Decamps I, Bregeon F, Thomas P, Auffray JP (2006) Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 105(5):911–919
Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, van der Poll T, Vroom MB, Hollmann M, Schultz MJ (2008) Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 108(1):46–54. https://doi.org/10.1097/01.anes.0000296068.80921.10
Neumann P, Rothen HU, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G (1999) Positive end-expiratory pressure prevents atelectasis during general anaesthesia even in the presence of a high inspired oxygen concentration. Acta Anaesthesiol Scand 43(3):295–301
Tusman G, Bohm SH, Vazquez de Anda GF, do Campo JL, Lachmann B (1999) ‘Alveolar recruitment strategy’ improves arterial oxygenation during general anaesthesia. Br J Anaesth 82(1):8–13
D’Antini D, Huhle R, Herrmann J, Sulemanji DS, Oto J, Raimondo P, Mirabella L, Hemmes SNT, Schultz MJ, Pelosi P, Kaczka DW, Vidal Melo MF, Gama de Abreu M, Cinnella G, European Society of A., The PVN (2018) Respiratory system mechanics during low versus high positive end-expiratory pressure in open abdominal surgery: a substudy of PROVHILO randomized controlled trial. Anesth Analg 126(1):143–149. https://doi.org/10.1213/ANE.0000000000002192
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S, Group IS (2013) A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 369(5):428–437. https://doi.org/10.1056/NEJMoa1301082
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, Moine P, Vidal Melo MF, Repine JE (2015) Perioperative lung protective ventilation in obese patients. BMC Anesthesiol 15(1):56. https://doi.org/10.1186/s12871-015-0032-x
Carvalho AR, Jandre FC, Pino AV, Bozza FA, Salluh JI, Rodrigues R, Soares JH, Giannella-Neto A (2006) Effects of descending positive end-expiratory pressure on lung mechanics and aeration in healthy anaesthetized piglets. Crit Care 10(4):R122. https://doi.org/10.1186/cc5030
Carvalho AR, Spieth PM, Pelosi P, Vidal Melo MF, Koch T, Jandre FC, Giannella-Neto A, de Abreu MG (2008) Ability of dynamic airway pressure curve profile and elastance for positive end-expiratory pressure titration. Intensive Care Med 34(12):2291–2299. https://doi.org/10.1007/s00134-008-1301-7
Slutsky AS, Ranieri VM (2013) Ventilator-induced lung injury. N Engl J Med 369(22):2126–2136. https://doi.org/10.1056/NEJMra1208707
Suter PM, Fairley B, Isenberg MD (1975) Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 292(6):284–289. https://doi.org/10.1056/NEJM197502062920604
Carvalho AR, Jandre FC, Pino AV, Bozza FA, Salluh J, Rodrigues R, Ascoli FO, Giannella-Neto A (2007) Positive end-expiratory pressure at minimal respiratory elastance represents the best compromise between mechanical stress and lung aeration in oleic acid induced lung injury. Crit Care 11(4):R86. https://doi.org/10.1186/cc6093
Kano SH, Lanteri CJ, Duncan AW, Sly PD (1994) Influence of nonlinearities on estimates of respiratory mechanics using multilinear regression-analysis. J Appl Physiol 77(3):1185–1197
Bersten AD (1998) Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J 12(3):526–532
Rohrer F (1915) Der Strömungswiderstand in den menschlichen Atemwegen und der Einfluss der unregelmässigen Verzweigung des Bronchialsystems auf den Atmungsverlauf in verschiedenen Lungenbezirken. Pflügers Archiv Eur J Physiol 162(5–5):225–299
Carvalho AR, Pacheco SA, de Souza Rocha PV, Bergamini BC, Paula LF, Jandre FC, Giannella-Neto A (2013) Detection of tidal recruitment/overdistension in lung-healthy mechanically ventilated patients under general anesthesia. Anesth Analg 116(3):677–684. https://doi.org/10.1213/ANE.0b013e318254230b
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70
Carvalho AR, Bergamini BC, Carvalho NS, Cagido VR, Neto AC, Jandre FC, Zin WA, Giannella-Neto A (2013) Volume-independent elastance: a useful parameter for open-lung positive end-expiratory pressure adjustment. Anesth Analg 116(3):627–633. https://doi.org/10.1213/ANE.0b013e31824a95ca
Stenqvist O (2003) Practical assessment of respiratory mechanics. Br J Anaesth 91(1):92–105
Brismar B, Hedenstierna G, Lundquist H, Strandberg A, Svensson L, Tokics L (1985) Pulmonary densities during anesthesia with muscular relaxation–a proposal of atelectasis. Anesthesiology 62(4):422–428
Hedenstierna G (2012) Oxygen and anesthesia: what lung do we deliver to the post-operative ward? Acta Anaesth Scand 56(6):675–685
Muscedere JG, Mullen JB, Gan K, Slutsky AS (1994) Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 149(5):1327–1334. https://doi.org/10.1164/ajrccm.149.5.8173774
Hauber HP, Karp D, Goldmann T, Vollmer E, Zabel P (2010) Effect of low tidal volume ventilation on lung function and inflammation in mice. BMC Pulm Med 10:21. https://doi.org/10.1186/1471-2466-10-21
Jaber S, Coisel Y, Chanques G, Futier E, Constantin JM, Michelet P, Beaussier M, Lefrant JY, Allaouchiche B, Capdevila X, Marret E (2012) A multicentre observational study of intra-operative ventilatory management during general anaesthesia: tidal volumes and relation to body weight. Anaesthesia 67(9):999–1008. https://doi.org/10.1111/j.1365-2044.2012.07218.x
Neumann P, Rothen HU, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G (1999) Positive end-expiratory pressure prevents atelectasis during general anaesthesia even in the presence of a high inspired oxygen concentration. Acta Anaesthesiol Scand 43(3):295–301
Pintado MC, de Pablo R, Trascasa M, Milicua JM, Rogero S, Daguerre M, Cambronero JA, Arribas I, Sanchez-Garcia M (2013) Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respir Care 58(9):1416–1423. https://doi.org/10.4187/respcare.02068
Amini R, Herrmann J, Kaczka DW (2017) Intratidal overdistention and derecruitment in the injured lung: a simulation study. IEEE Trans Biomed Eng 64(3):681–689. https://doi.org/10.1109/TBME.2016.2572678
Mead J, Collier C (1959) Relation of volume history of lungs to respiratory mechanics in anesthetized dogs. J Appl Physiol 14(5):669–678
Thammanomai A, Hamakawa H, Bartolak-Suki E, Suki B (2013) Combined effects of ventilation mode and positive end-expiratory pressure on mechanics, gas exchange and the epithelium in mice with acute lung injury. PloS ONE 8(1):e53934. https://doi.org/10.1371/journal.pone.0053934
Camilo LM, Avila MB, Cruz LF, Ribeiro GC, Spieth PM, Reske AA, Amato M, Giannella-Neto A, Zin WA, Carvalho AR (2014) Positive end-expiratory pressure and variable ventilation in lung-healthy rats under general anesthesia. PloS ONE 9(11):e110817. https://doi.org/10.1371/journal.pone.0110817
Pecchiari M, Monaco A, Koutsoukou A, Della Valle P, Gentile G, D’Angelo E (2014) Effects of various modes of mechanical ventilation in normal rats. Anesthesiology 120(4):943–950. https://doi.org/10.1097/ALN.0000000000000075
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial I, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, Guimaraes HP, Romano ER, Regenga MM, Taniguchi LNT, Teixeira C, Pinheiro de Oliveira R, Machado FR, Diaz-Quijano FA, Filho MSA, Maia IS, Caser EB, Filho WO, Borges MC, Martins PA, Matsui M, Ospina-Tascon GA, Giancursi TS, Giraldo-Ramirez ND, Vieira SRR, Assef M, Hasan MS, Szczeklik W, Rios F, Amato MBP, Berwanger O, Ribeiro de Carvalho CR (2017) Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 318 (14):1335–1345. https://doi.org/10.1001/jama.2017.14171
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372(8):747–755. https://doi.org/10.1056/NEJMsa1410639
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, Gajic O, El-Tahan MR, Ghamdi AAA, Günay E, Jaber S, Kokulu S, Kozian A, Licker M, Lin W-Q, Maslow AD, Memtsoudis SG, Miranda DR, Moine P, Ng T, Paparella D, Ranieri VM, Scavonetto F, Schilling T, Selmo G, Severgnini P, Sprung J, Sundar S, Talmor D, Treschan T, Unzueta C, Weingarten TN, Wolthuis EK, Wrigge H, Amato MBP, Costa ELV, de Abreu MG, Pelosi P, Schultz MJ (2016) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 4(4):272–280. https://doi.org/10.1016/s2213-2600(16)00057-6
Jandre FC, Modesto FC, Carvalho AR, Giannella-Neto A (2008) The endotracheal tube biases the estimates of pulmonary recruitment and overdistension. Med Biol Eng Comput 46(1):69–73. https://doi.org/10.1007/s11517-007-0227-5
Webb HH, Tierney DF (1974) Experimental pulmonary-edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 110(5):556–565
Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M (1987) Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation. An experimental study. Am Rev Respir Dis 135(2):312–315. https://doi.org/10.1164/arrd.1987.135.2.312
Parker JC, Hernandez LA, Longenecker GL, Peevy K, Johnson W (1990) Lung edema caused by high peak inspiratory pressures in dogs. Role of increased microvascular filtration pressure and permeability. Am Rev Respir Dis 142(2):321–328. https://doi.org/10.1164/ajrccm/142.2.321
Rothen HU, Sporre B, Engberg G, Wegenius G, Hogman M, Hedenstierna G (1995) Influence of gas composition on recurrence of atelectasis after a reexpansion maneuver during general anesthesia. Anesthesiology 82(4):832–842
Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, Eccher G, Gattinoni L (1999) Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 91(5):1221–1231
Zin WA, Martins MA, Silva PR, Sakae RS, Carvalho AL, Saldiva PH (1989) Effects of abdominal opening on respiratory system mechanics in ventilated rats. J Appl Physiol 66(6):2496–2501. https://doi.org/10.1152/jappl.1989.66.6.2496
Funding
This study was supported by grants from the Brazilian Council for Scientific and Technology Development (CNPq)—140047/2008-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in compliance with the “Principles of Laboratory Animal Care” formulated by the National Society for Medical Research and the “Guiding Principles in the Care and Use of Animals” approved by the Council of the American Physiological Society, USA. The present study was approved by the Institutional Animal Care and Use Committee (CEUA CCS, IBCCF-019).
Rights and permissions
About this article
Cite this article
Soares, J.H.N., Carvalho, A.R., Bergamini, B.C. et al. Alveolar Tidal recruitment/derecruitment and Overdistension During Four Levels of End-Expiratory Pressure with Protective Tidal Volume During Anesthesia in a Murine Lung-Healthy Model. Lung 196, 335–342 (2018). https://doi.org/10.1007/s00408-018-0096-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0096-8