Abstract
Purpose
Our aim was to investigate the course of the hearing capacity of the better-hearing ear in single-sided deafness (SSD) and asymmetric hearing loss (AHL) over time, in a multicenter study.
Methods
We included 2086 pure-tone audiograms from 323 patients with SSD and AHL from four hospitals and 156 private practice otorhinolaryngologists. We collected: age, gender, etiology, duration of deafness, treatment with CI, number and monosyllabic speech recognition, numerical rating scale (NRS) of tinnitus intensity, and the tinnitus questionnaire according to Goebel and Hiller. We compared the pure tone audiogram of the better-hearing ear in patients with SSD with age- and gender-controlled hearing thresholds from ISO 7029:2017.
Results
First, individuals with SSD showed a significantly higher hearing threshold from 0.125 to 8 kHz in the better-hearing ear compared to the ISO 7029:2017. The duration of deafness of the poorer-hearing ear showed no relationship with the hearing threshold of the better-hearing ear. The hearing threshold was significantly higher in typically bilaterally presenting etiologies (chronic otitis media, otosclerosis, and congenital hearing loss), except for Menière’s disease. Second, subjects that developed AHL did so in 5.19 ± 5.91 years and showed significant reduction in monosyllabic word and number recognition.
Conclusions
Individuals with SSD show significantly poorer hearing in the better-hearing ear than individuals with NH from the ISO 7029:2017. In clinical practice, we should, therefore, inform our SSD patients that their disease is accompanied by a reduced hearing capacity on the contralateral side, especially in certain etiologies.
Similar content being viewed by others
Introduction
Single-sided deafness (SSD) is defined as severe to profound hearing loss in the poorer-hearing ear and (almost) normal-hearing (NH) in the better-hearing ear.
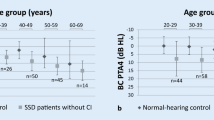
In a previous study we have shown, that the better-hearing ear of subjects with SSD has a significantly higher air-conducted (AC) pure-tone average in the frequencies 0.5, 1, 2, and 4 kHz (AC PTA4) compared with age- and gender-controlled hearing thresholds from ISO 7029:2017 [3].
One possible explanation for the higher AC PTA4 is an increased strain on the last-hearing ear, as persons with SSD tend to turn their better-hearing ear towards sound sources. This idea is supported by high-tone accentuated hearing impairment, such as the hearing impairment seen in persons with presbyacusis. To check this hypothesis, we included hearing thresholds from 0.125 kHz up to 8 kHz in the present study. In addition, we included monosyllabic word recognition and number recognition to evaluate the impact on speech recognition.
In our prior study, treatment with a cochlear implant (CI), duration of deafness, and etiology showed no significant relationship with the hearing ability of the better-hearing ear [3]. It was surprising that etiology showed no significant relationship, considering frequently bilateral occurring diseases, such as otosclerosis [4,5,6,7,8,9,10], Menière’s disease [11,12,13], and enlarged vestibular aqueduct syndrome [14]. We hypothesized that selection bias (only patients requested CI treatment were enrolled) might be a contributing factor. In the present study, we, therefore, acquired hearing results from individuals with SSD and asymmetric hearing loss (AHL) with and without CI from in- and out-patient care to incorporate earlier stages of the disease and to improve the charting of the disease over time.
In the present study, we also included measurements of tinnitus burden. We suspected a relationship between tinnitus burden and hearing capacity, because Mertens et al. [15] described a significant influence of tinnitus in the poorer-hearing ear on speech recognition in background noise in the better-hearing ear in subjects with SSD.
Methods
The present study was performed with approval of the Ethics Commission Freiburg (No. 560-19) and in compliance with national law and the Declaration of Helsinki of 2013 (in the current revised edition) (DRKS00022115).
Study participants
We recruited subjects (over 18 years) with SSD and AHL that presented at one of the participating hospitals: University Hospital Freiburg, Central Army Hospital Koblenz, Medical University Hanover, and University Hospital Marburg.
Subjects with SSD and AHL had severe to profound hearing loss in the poorer-hearing ear and differed in the hearing capacity of the better-hearing ear: SSD had an untreated AC PTA4 ≤ 30 dB HL and AHL an untreated AC PTA4 > 30 dB HL to ≤ 60 dB HL. In SSD the interaural asymmetry was required to be ≥ 30 dB HL [1].
Data acquisition
We searched the databases of all participating hospitals for candidates. After receiving informed consent and releases from confidentiality, we contacted primary doctors of otorhinolaryngology to receive auditory measurements performed before and after consultation at the participating hospitals.
Acquired data
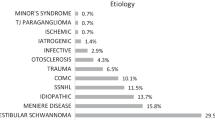
Anamnestic data included age, gender, duration of deafness, treatment with CI, and etiology. We did not acquire data with regard to alternative treatment strategies, such as Contralateral Routing of Signals (CROS) or bone-anchored hearing system (BAHS). In non-CI users we calculated duration of deafness from the anamnestic onset of deafness to the date of measurement. For CI users the duration of deafness preoperatively was defined from the anamnestic onset of deafness to the date of measurement. After CI surgery deafness duration remained the duration between anamnestic onset of deafness and CI surgery. Etiology was arranged into eleven categories: (1) sudden hearing loss (SHL), (2) trauma (cranio-cerebral trauma with contusion labyrinthi, petrous bone fracture), (3) vestibular schwannoma, (4) Menière’s disease, (5) infectious disease (meningitis, mumps, labyrinthitis, influenza, acute otitis, neurolues, scarlet fever, measles) (6) chronic otitis media (OM), (7) congenital hearing loss, (8) otosclerosis, (9) post-ear-surgery (post-op) hearing loss, (10) other (large aquaeductus syndrome, Cogan-1-syndrom, Von Hippel–Lindau-Syndrome, status after radiotherapy, status after brain stem ischemia), and (11) unknown (no routine genetic screening).
If available, we retrospectively included bone-conducted (BC) and AC thresholds of both ears for the frequencies 125 Hz to 8 kHz and monosyllabic word recognition and number recognition using the Freiburg intelligibility test [17] from the participating hospitals and private practice otorhinolaryngologists.
To evaluated tinnitus burden we prospectively collected numerical rating scale (NRS) between 0 and 10 (10 representing the highest tinnitus burden [18]) and the tinnitus questionnaire by Goebel and Hiller [19].
We compared the hearing threshold with hearing thresholds from the ISO 7029:2017, which defines hearing thresholds for female and male “otologically normal persons” between 20 and 80 years. “Otologically normal person” is defined as an adult without symptoms of ear disease, complete obstruction of the auditory canal, excessive noise exposure, contact with ototoxic substances, and hereditary hearing loss. Hearing thresholds for the ISO 7029:2017 were retrieved by presenting a pure tone via a headphone to one ear. To compare subjects with SSD included in the present study we produced a “control group” consisting of hearing thresholds from subjects with same aged and gender derived from the ISO 7029:2017.
Data analysis
Statistical data analysis was performed with Gnu R. The Shapiro–Wilk test showed non-normal distribution, so we applied Wilcoxon signed rank tests and Kruskal–Wallis rank sum tests (Table 1). For correlations, we used Pearson’s correlation analysis.
To compare groups with significant differences in age and/or gender distribution, we employed the AC PTA4 difference as the dependent variable. The AC PTA4 difference is the age- and gender-corrected difference between the individual AC PTA4 of the better-hearing ear of subjects with SSD and hearing thresholds from ISO 7029:2017 (PTA4 better-hearing ear—PTA4 from ISO 7029:2017). AC PTA4 differences > 0 indicate that the AC PTA4 of the subjects with SSD is greater than the AC PTA4 from ISO 7029:2017. If the AC PTA4 difference is = 0 there is no difference between the subjects with SSD and the ISO 7029:2017 control group. We applied the AC PTA4 difference only to compare subjects with SSD, as in subjects with AHL a mild to moderate hearing loss on the better-hearing side is prevalent, and therefore, an age and/or gender correction with the ISO 7029:2017 is not applicable.
We categorized our participants into three groups: (1) AHL in all included measurements, (2) SSD in all included measurements, and (3) hearing threshold of the better-hearing ear deteriorated from SSD to AHL during the study period. To test this categorical variable, we used a Chi-squared test.
Results
We enrolled 323 subjects from which 277 were subjects with SSD and 46 subjects with AHL (Table 2).
SSD
Pure tone-audiometry
From 277 subjects with SSD, we could include 1933 AC pure-tone audiograms and 1572 BC pure-tone audiograms (Table 1). Comparing the AC pure-tone thresholds from subjects with SSD to age- and gender-controlled hearing thresholds from ISO 7029:2017 we saw a significantly higher hearing thresholds in subjects with SSD at each measured frequency (Table 1, Fig. 1).
To check for systemic error, we compared the subjects with SSD from the hospitals Freiburg, Marburg, and Koblenz separately. Each analysis revealed significantly higher thresholds for subjects with SSD in each measured frequency (p < 0.05). A separate analysis of the Hannover group was not possible, because only two patients participated.
To check for the influence of an air–bone gap, we performed separate tests, including only thresholds with an air–bone gap smaller than 10 dB (excluding 0.125 and 8 kHz). We were able to retrieve air–bone gaps from 1572 pure-tone audiograms, because in 1572, a BC pure-tone audiogram was available. 249 subjects showed an air–bone gap smaller than 10 dB in 1332 audiograms. These analyses also revealed significantly higher hearing thresholds at each frequency (p < 0.05).
Duration of deafness
In most subjects with NH (ISO 7029:2017) the hearing threshold increases over the life span. When investigating the effect of duration of deafness we have to correct for this natural increase in hearing threshold. We, therefore, used the age- and gender-corrected AC PTA4 difference (PTA4 better-hearing ear—PTA4 from ISO 7029:2017) to investigate the relationship between deafness duration and hearing capacity of the better hearing ear. We, therefore, derived an age- and gender-corrected AC PTA4 difference correlated with the duration of deafness with hearing performance in the better-hearing ear (Table 1). The AC PTA4 difference showed a significant positive correlation (p < 0.001; cor = 0.08) with the duration of deafness (Fig. 2).
Correlation of air-conducted pure-tone thresholds average difference (AC PTA4 difference = PTA4 better-hearing ear—PTA4 from ISO 7029:2017) with duration of deafness in years in subjects with SSD. The AC PTA4 difference is the difference between the individual AC PTA4 of the better-hearing ear of subjects with SSD and age- and gender-controlled hearing thresholds from ISO 7029:2017. SSD subjects with single-sided deafness
Etiology
Age and gender were significantly different between various etiology groups. As we cannot control number and monosyllabic word recognition for the bias of age and gender, we did not compare number and monosyllabic word recognition between etiology groups. In case of hearing thresholds, we used the age- and gender-corrected AC PTA4 difference (PTA4 better-hearing ear—PTA4 from ISO 7029:2017) to investigate the relationship between etiology and hearing capacity of the better-hearing ear in subjects with SSD. We saw a significant relationship in the Kruskal–Wallis rank sum test between etiology and AC PTA4 difference (Table 1). In the post-hoc analysis we excluded the etiology groups “others” and “unknown”.
Subjects with chronic otitis media (OM) showed the highest AC PTA4 difference of all etiology groups (Fig. 3A). To investigate the impact of conductive hearing impairment, we compared air–bone gaps between etiologies in cases in which BC PTA4 was available. Subjects with chronic OM had a significantly higher PTA4 air–bone gap compared with all other etiologies. (Fig. 3B).
A Comparison of the average difference in air-conducted pure-tone thresholds (AC PTA4 difference = PTA4 better-hearing ear—PTA4 from ISO 7029:2017) in relation to etiology in subjects with SSD. The AC PTA4 difference is the difference between the individual AC PTA4 of the better-hearing ear of subjects with SSD and age- and gender-controlled hearing thresholds from ISO 7029:2017. B Comparison of the average difference in air–bone gap pure-tone thresholds (AC PTA4 air–bone gap = PTA4 better-hearing ear—PTA4 from ISO 7029:2017) in relation to etiology in subjects with SSD. SSD subjects with single-sided deafness, TA pure-tone measurements, SHL sudden hearing loss, Schwannoma vestibularis schwannoma, chronic OM chronic otitis media; level of significance: *** - p < 0.001; - ** p < 0.01; * - p < 0.05
CI user vs. non-CI user
We found no significant difference in age and gender between CI users and non-CI users. We could, therefore, compare number recognition, monosyllabic word recognition, AC PTA4, preoperative and postoperative thresholds without bias of age or gender.
In CI users, preoperative AC pure-tone thresholds of all frequencies from 0.125 to 8 kHz in the better-hearing ear were significantly lower than in non-CI users (Table 1, Fig. 4A). The postoperative AC pure-tone thresholds were significantly lower in CI-users than in no-CI users for the frequencies from 0.125 to 4 kHz and not for 6 kHz and 8 kHz (Table 1, Fig. 4B).
Comparison of air-conducted pure-tone thresholds from 0.125 kHz to 8 kHz between non-CI users with SSD (white) and A preoperative pure-tone audiograms of CI users with SSD (grey) and B postoperative pure-tone audiograms of CI users with SSD (grey). SSD subjects with single-sided deafness; level of significance: *** - p < 0.001; ** - p < 0.01; * - p < 0.05
Preoperative AC PTA4 were available in 692 of 700 AC pure-tone audiograms, as the value for 0.5, 1, 2, or 4 kHz was missing in 8 AC pure-tone audiograms. Preoperative AC PTA4 did not differ significantly between CI users and non-CI users (Table 1). Postoperative AC PTA4 was significantly lower in CI users (Table 1).
With regard to the CI users, we included measurements of number recognition and monosyllabic word recognition of the better-hearing ear performed before and after CI, in the statistical analysis. Wilcoxon signed rank tests revealed no significant difference between CI users and non-CI users (Table 1).
To investigate changes in the better-hearing ear after the CI operation, we compared AC PTA4 results preoperative up to 5 year postoperative. No significant differences between the included appointments were revealed (Table 1).
Tinnitus NRS and tinnitus questionnaire (German adaptation by Goebel and Hiller)
We correlated the (1) NRS and (2) questionnaire results with the AC PTA4 difference. Neither correlation was significant (Table 1).
CI users had a significantly higher NRS than non-CI users (p < 0.05). A significantly lower NRS was found in CI users while using the CI than without using the CI (p < 0.001).
SSD to AHL
The categories (1) AHL in all measurements (n = 46), (2) SSD in all measurements (n = 173), and (3) SSD to AHL (n = 104) did not differ significantly in gender, treatment with CI, or etiology.
Subjects that went from SSD to AHL during the included measurements (Table 2) went from AC PTA4 of 21.12 ± 12.27 dB HL to 35.54 ± 19.66 dB HL. Monosyllabic word recognition went from 88.10% ± 20.40% at 65 dB to 73.79% ± 27.80% at 65 dB (p < 0.001). The 50% correct numeric speech recognition went from 14.52 ± 10.02 dB SPL to 22.80 ± 27.80 dB SPL (p < 0.001).
On average the subjects went from SSD to AHL at 5.19 ± 5.91 years (median: 2.78 years) after the first included measurement (Fig. 5). In cases of fluctuating hearing thresholds in the better-hearing ear we measured the time from SSD to AHL from the first included measurement diagnosed with SSD to the measurement after which all hearing threshold were diagnosed with AHL. In a Kruskal–Wallis rank sum tests the etiology had no relationship with the duration between the diagnosis of SSD and AHL.
Discussion
We found a significant higher hearing threshold in the better hearing-ear of subjects with SSD compared with age- and gender-controlled hearing thresholds from ISO 7029:2017. Subjects that developed AHL did so in 5.19 ± 5.91 years and showed significant reduction in monosyllabic word recognition and numeric speech recognition. Age, gender and treatment with CI were not correlated with developing AHL.
The difference between ISO 7029:2017 and subjects with SSD through all frequencies might be a systematic error. However, this is unlikely, because we included audiograms from 192 subjects performed by 156 private practice otorhinolaryngologists who performed their hearing measurements independently of each other. To confront this possible bias, we analyzed subjects from each participating hospital. We saw a significantly higher hearing threshold in all frequencies for the better-hearing ear of subjects with SSD in each separate analysis. The large number of independent investigators and the separate analyses performed minimize the possibility of a systematic bias substantially, enabling us to be confident in the present results.
The higher hearing threshold in the better-hearing ear of participants with SSD is more pronounced at higher frequencies, but the hearing loss is evident over all frequencies. This result opposes our hypothesis that individuals with SSD strain their last-hearing ear by turning it towards sound sources. This strain could result from additional noise and/or stretching of the cervical vessels resulting in reduced blood flow. This idea is also weakened by the low correlation between AC PTA4 difference (controlled for age) and duration of hearing impairment. If early alteration because of hearing stress on the cochlea caused higher hearing threshold, we would expect a strong correlation with the duration of hearing impairment and/or a correlation to inner ear trauma because of noise exposure. Similarly, AC PTA4 difference of the better-hearing ear did not change significantly in SSD CI users preoperatively to 5 year post-CI. The duration of deafness was not significantly different between subjects with SSD, subjects with AHL and subjects that went from SSD to AHL. In subjects that went from SSD to AHL hearing loss in the better-hearing ear progressed in mean within the first 5 years. Interestingly, the etiology showed no relation with the duration of progression from SSD to AHL.
We choose to investigate CI as a potential factor, because a CI would reduce the turning of the last-hearing ear towards sound sources. Number and monosyllabic word recognition did not differ significantly between CI users and non-CI users, because number and monosyllabic word recognition of the better-hearing ear showed a ceiling effect at 100% correct. To investigate, if hearing thresholds already differed before implantation, we compared preoperative thresholds with thresholds from non-CI users; we only found a significant higher hearing threshold in non-CI users at the frequencies 125 Hz and 8 kHz. Therefore, we have no selection bias in the frequencies from 0.5 to 6 kHz when comparing postoperative hearing thresholds with hearing thresholds from non-CI users. After treatment with CI, we saw significantly lower hearing thresholds in CI users with SSD from 0.5 to 4 kHz. Differences in socio-economic status, personal support system, educational background, noise exposure in the work place and intelligence could contribute to these differences. Due to the retrospective nature of the study, we did not investigate these factors. Interestingly, the lower hearing threshold in CI users is evident over all frequencies with the exception of 6 kHz. This also contradicts our hypothesis.
To investigate this hypothesis further, head movements towards sound sources by individuals with SSD can be monitored, and persons with higher and lower noise exposure can be compared. In addition, hearing loss at frequencies higher than 8 kHz can be investigated in the better-hearing ear of subjects with SSD. The hearing impairment over all frequencies of the better-hearing ear suggests that it might be caused by sympathetic hearing loss. Similar to sympathetic ophthalmia, the hearing loss is caused by damage to the contralateral cochlear resulting in an autoimmune response to the contralateral side [20,21,22].
BC thresholds reflect the hearing capacity of the cochlear and auditory nerve. However, BC thresholds do not reflect the actual hearing capacity in everyday life. In the present study, unlike in our previous study on this subject [3], we compared the AC threshold. We choose to do so for two reasons. (1) We compared our participants with ISO 7029:2017, which only contains AC thresholds. (2) As we included measurements from private practice otorhinolaryngologists, BC thresholds were not regularly available. This choice led to a challenge: conductive hearing impairment causing air–bone gaps higher than 10 dB might influence our results (the reason that we choose BC thresholds in our previous study). We, therefore, excluded all measurements with an air–bone gap ≥ 10 dB and reran the comparison between subjects with SSD and hearing thresholds from ISO 7029:2017 for each frequency. These analyses also revealed a significantly higher hearing thresholds in subjects with SSD in each frequency. Therefore, conductive hearing loss did not contribute to the higher hearing threshold in the better-hearing ear of subjects with SSD. A limitation is, as described above, that air–bone gaps were only available in audiograms with additionally measured BC thresholds.
However, we found that subjects with chronic OM showed the highest AC PTA4 difference, because subjects with chronic OM had the largest air–bone gap in the better-hearing ear compared to other etiologies. The elevated air–bone gap is most likely caused by reduced middle ear ventilation on both sides. The contralateral ear in patients with chronic OM show abnormalities in the otoscopic examination from 50% up to 83.3% [23, 24]. Bilateral chronic OM is seen in 12% of cases [25].
Individuals with congenital SSD had an elevated hearing threshold compared with other etiologies in the present study. Two explanations can be proposed: (1) the neurological influence of congenital SSD and (2) the etiology of congenital SSD. Unilateral hearing in the vulnerable phase before the age of 4 years can lead to central reorganization with long-lasting effects [26,27,28]. In the literature, congenital SSD is reported to be caused by congenital CMV infection in over 20% of children with SSD [28,29,30]. This is relevant, as up to 75% of children with SSD attributable to congenital CMV develop delayed-onset contralateral hearing loss [31]. In addition, alterations in MRI and CT might be more frequent on the contralateral side in individuals with congenital SSD than in NH individuals [32]. Future studies including the systematic evaluation of MRI and CT data would thus be of interest.
Subjects with otosclerosis also revealed higher AC PTA4 differences than other etiologies. A bilateral otosclerosis is seen in 62–80% individuals and usually develops in one ear first [4,5,6,7,8,9,10]. Therefore, our findings are in agreement with the literature.
Surprisingly, the included subjects with Menière’s disease showed no significantly higher hearing thresholds than other etiologies. From the literature we know that Menière’s disease occurs bilaterally in approximately one-third of cases [11,12,13], and that, after 20 years of disease duration, over 40% of subjects develop bilateral Menière’s disease [33, 34]. In our study, only two subjects with Menière’s disease had had a duration of hearing loss longer than 20 years. Eight out of 18 subjects progressed from SSD to AHL during the time span of the included hearing measurements. The reason that we have no significantly increased hearing threshold in subjects with Menière’s disease might be, because we were only able to include two subjects with a longer duration of disease. Perhaps some of the included participants will develop bilateral disease during their lifetime.
We did not compare the recognition of numbers and monosyllabic words between the etiologies, because the various etiological groups differed significantly in age and gender. Since we could not control for age and gender, in contrast to the AC PTA4 difference, the results of the speech recognition tests might possibly be overshadowed by the effect of age or gender.
Similarly, neither NRS of tinnitus burden nor results from the tinnitus questionnaire after Goebel and Hiller [19] showed a significant relationship with the hearing ability of the better-hearing ear in subjects with SSD. This might be, because in contrast to Mertens et al. [15], we were not able to included speech recognition in background noise in our retrospective study design. In future prospective studies, an investigation of the relationship between tinnitus and more challenging hearing measurements, such as speech recognition in background noise or localization of sound sources, would be of interest.
In clinical practice, we should inform our SSD patients that their disease is accompanied by a reduced hearing capacity on the contralateral side, especially in certain etiologies (congenital SSD, otosclerosis and chronic otitis media), and that a longer SSD duration and tinnitus will not worsen their contralateral ear. CI treatment showed no negative relationship with the hearing threshold of the contralateral better-hearing ear.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Vincent C, Arndt S, Firszt JB et al (2015) Identification and evaluation of cochlear implant candidates with asymmetrical hearing loss. In: Audiology and Neurotology. S. Karger AG, pp 87–89
Van De Heyning P, Távora-Vieira D, Mertens G et al (2017) Towards a unified testing framework for single-sided deafness studies: a consensus paper. Audiol Neurotol 21:391–398. https://doi.org/10.1159/000455058
Arndt S, Wesarg T, Stelzig Y et al (2019) Influence of single-sided deafness on the auditory capacity of the better ear. German version. HNO 67:739–749. https://doi.org/10.1007/s00106-019-00730-1
Hueb MM, Goycoolea MV, Paparella MM, Oliveira JA (1991) Otosclerosis: the University of Minnesota temporal bone collection. Otolaryngol Head Neck Surg 105:396–405. https://doi.org/10.1177/019459989110500308
Sabbe A, Verhaert N, Joosen A (2015) Otosclerosis: shift in bone conduction after stapedectomy. B-ENT 11:183–189
Crompton M, Cadge BA, Ziff JL et al (2019) The epidemiology of otosclerosis in a British cohort. Otol Neurotol 40:22–30. https://doi.org/10.1097/MAO.0000000000002047
House HP, Hansen MR, Al Dakhail AAA, House JW (2002) Stapedectomy versus stapedotomy: comparison of results with long-term follow-up. Laryngoscope 112:2046–2050. https://doi.org/10.1097/00005537-200211000-00025
del Bo M, Zaghis A, Ambrosetti U (1987) Some observations concerning 200 stapedectomies: fifteen years postoperatively. Laryngoscope 97:1211–1213. https://doi.org/10.1288/00005537-198710000-00017
Emmett J (1993) Physical examination and clinical evaluation of the patient with otosclerosis. Otolaryngol Clin North Am 26:353–357
Lippy WH, Berenholz LP, Burkey JM (1999) Otosclerosis in the 1960s, 1970s, 1980s, and 1990s. Laryngoscope 109:1307–1309. https://doi.org/10.1097/00005537-199908000-00022
Strupp M, Dlugaiczyk J, Ertl-Wagner BB et al (2020) Vestibular disorders. Dtsch Arztebl Int 117:300–310. https://doi.org/10.3238/ARZTEBL.2020.0300
Chaves AG, Boari L, Lei Munhoz MS (2007) The outcome of patients with Ménières disease. Braz J Otorhinolaryngol 73:346–350. https://doi.org/10.1016/S1808-8694(15)30078-1
Stahle J, Friberg U, Svedberg A (1991) Long-term progression of Meniére’s disease. Acta Otolaryngol Suppl 485:78–83. https://doi.org/10.3109/00016489109128047
Archibald HD, Ascha M, Gupta A et al (2019) Hearing loss in unilateral and bilateral enlarged vestibular aqueduct syndrome. Int J Pediatr Otorhinolaryngol 118:147–151. https://doi.org/10.1016/J.IJPORL.2018.12.023
Mertens G, Punte AK, De Ridder D, Van De Heyning P (2013) Tinnitus in a single-sided deaf ear reduces speech reception in the nontinnitus ear. Otol Neurotol 34:662–666. https://doi.org/10.1097/MAO.0B013E31828779F0
Chadha S, Kamenov K, Cieza A (2021) The world report on hearing, 2021. Bull World Health Organ 99:242. https://doi.org/10.2471/BLT.21.285643
Hahlbrock K (1953) Speech audiometry an new word-test. Arch Ohren Nasen Kehlkopfheilkg 162:394–431
Adamchic I, Langguth B, Hauptmann C, Tass PA (2012) Psychometric evaluation of visual analog scale for the assessment of chronic tinnitus. Am J Audiol. https://doi.org/10.1044/1059-0889(2012/12-0010)
Goebel G, Hiller W (1994) The tinnitus questionnaire. A standard instrument for grading the degree of tinnitus. Results of a multicenter study with the tinnitus questionnaire. HNO 42:166–172
Güttich A (1927) Zur pathologischen Anatomie der sympathischen Labyrinthitis. Passow-Schaefer-Beitr Anat Physiol Pathol Ther Ohres 27:6–9
Ten Gate WJF, Bachor E (2005) Autoimmune-mediated sympathetic hearing loss: a case report. Otol Neurotol 26:161–165. https://doi.org/10.1097/00129492-200503000-00005
Bachor E, Ten Cate WJF, Gloddek B, Ehsani N (2000) Immunohistochemical detection of humoral autoantibodies in patients with hearing loss in the last hearing ear. Laryngorhinootologie 79:131–134. https://doi.org/10.1055/S-2000-287
Ünsal Ö, Türk B, Seyhun N, Turgut S (2018) Contralateral Ear Findings in Chronic Otitis Media. Sisli Etfal Hastan Tip Bul. https://doi.org/10.5350/SEMB.20171129090822
Da Costa SS, Rosito LPS, Dornelles C, Sperling N (2008) The contralateral ear in chronic otitis media: a series of 500 patients. Arch Otolaryngol Head Neck Surg 134:290–293. https://doi.org/10.1001/ARCHOTO.2007.38
Umamaheswaran P, Mohanty S, Manimaran V et al (2020) A comparative study of sequential vs. simultaneous type I tympanoplasty in patients with bilateral chronic otitis media—Mucosal type. J Otol 15:59–61. https://doi.org/10.1016/J.JOTO.2019.12.005
Kitzes LM (1984) Some physiological consequences of neonatal cochlear destruction in the inferior colliculus of the gerbil, Meriones unguiculatus. Brain Res 306:171–178. https://doi.org/10.1016/0006-8993(84)90366-4
Reale RA, Brugge JF, Chan JCK (1987) Maps of auditory cortex in cats reared after unilateral cochlear ablation in the neonatal period. Brain Res 431:281–290. https://doi.org/10.1016/0165-3806(87)90215-X
van Wieringen A, Boudewyns A, Sangen A et al (2019) Unilateral congenital hearing loss in children: challenges and potentials. Hear Res 372:29–41
Usami SI, Kitoh R, Moteki H et al (2017) Etiology of single-sided deafness and asymmetrical hearing loss. Acta Otolaryngol 137:2–7. https://doi.org/10.1080/00016489.2017.1300321
Cushing SL, Gordon KA, Sokolov M et al (2019) Etiology and therapy indication for cochlear implantation in children with single-sided deafness: retrospective analysis. HNO 67:750–759. https://doi.org/10.1007/S00106-019-00729-8
Lanzieri TM, Chung W, Flores M et al (2017) Hearing loss in children with asymptomatic congenital cytomegalovirus infection. Pediatrics. https://doi.org/10.1542/PEDS.2016-2610
van Beeck Calkoen EA, Sanchez Aliaga E, Merkus P et al (2017) High prevalence of abnormalities on CT and MR imaging in children with unilateral sensorineural hearing loss irrespective of age or degree of hearing loss. Int J Pediatr Otorhinolaryngol 97:185–191. https://doi.org/10.1016/J.IJPORL.2017.04.002
Havia M, Kentala E (2004) Progression of symptoms of dizziness in Ménière’s disease. Arch Otolaryngol Head Neck Surg 130:431–435. https://doi.org/10.1001/ARCHOTOL.130.4.431
Friberg U, Stahle J, Svedberg A (1984) The natural course of Meniere’s disease. Acta Otolaryngol Suppl 406:72–77. https://doi.org/10.3109/00016488309123007
Hwi Park Y, Shin SH, Wan Byun S, Yeon Kim J (2016) Age- and gender-related mean hearing threshold in a highly-screened population: the Korean national health and nutrition examination survey 2010–2012. PLoS ONE. https://doi.org/10.1371/journal.pone.0150783
Bahng J, Lee J (2015) Hearing thresholds for a geriatric population composed of Korean males and females. J Audiol Otol 19:91–96. https://doi.org/10.7874/JAO.2015.19.2.91
Kim HJ, Lee HJ, An SY et al (2015) Analysis of the prevalence and associated risk factors of Tinnitus in adults. PLoS ONE. https://doi.org/10.1371/journal.pone.0127578
Kim SH, Lim EJ, Kim HS et al (2010) Sex differences in a cross sectional study of age-related hearing loss in Korean. Clin Exp Otorhinolaryngol 3:27–31. https://doi.org/10.3342/CEO.2010.3.1.27
Corso JF (1963) Age and sex differences in pure-tone thresholds. Survey of hearing levels from 18 to 65 years. Arch Otolaryngol 77:385–405. https://doi.org/10.1001/ARCHOTOL.1963.00750010399008
Baraldi GDS, De Almeida LC, Borges ACDC (2007) Hearing loss in aging. Braz J Otorhinolaryngol 73:64–70. https://doi.org/10.1016/S1808-8694(15)31123-X
Lazard DS, Collette JL, Perrot X (2012) Speech processing: from peripheral to hemispheric asymmetry of the auditory system. Laryngoscope 122:167–173. https://doi.org/10.1002/LARY.22370
Hartvig Jensen J, Angaard Johansen P, Borre S (1989) Unilateral sensorineural hearing loss in children and auditory performance with respect to right/left ear differences. Br J Audiol 23:207–213. https://doi.org/10.3109/03005368909076501
Niedzielski A, Humeniuk E, Błaziak P, Gwizda G (2006) Intellectual efficiency of children with unilateral hearing loss. Int J Pediatr Otorhinolaryngol 70:1529–1532. https://doi.org/10.1016/J.IJPORL.2006.02.011
Wettstein VG, Probst R (2018) Right ear advantage of speech audiometry in single-sided deafness. Otol Neurotol 39:417–421. https://doi.org/10.1097/MAO.0000000000001756
Acknowledgements
We thank the Förderverein Taube Kinder lernen Hören e.V. Freiburg for the financial support of our research work. This work was also supported by the Berta-Ottenstein-Programme for Clinician Scientists, Faculty of Medicine, University of Freiburg.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Speck reports the following: travel cost reimbursement from MedEl, Financial support for research from KIND. E. Gundlach reports no conflict of interest. S. Schmidt reports no conflict of interest. N. Spyckermann reports no conflict of interest. A. Lesinski-Schiedat reports the following: financial support for research, travel cost reimbursement from Advanced Bionics, Cochlear, MedEl, Oticon (alphabetical order). A. Rauch reports no conflict of interest. A. Aschendorff reports the following: advanced Bionics: financial support for research, Medical Advisory Board, travel cost reimbursement; Cochlear: financial support for research, travel cost reimbursement; MED-EL: financial support for research, travel cost reimbursement; Oticon Medical: financial support for research, travel cost reimbursement. K. Thangavelu reports no conflict of interest. K. Reimann reports the following: cochlear: financial support for research, travel cost reimbursement; MED-EL: financial support for research, travel cost reimbursement. S. Arndt reports the following: advanced Bionics: travel cost reimbursement, financial support for research; Cochlear: financial support for research, travel cost reimbursement; MED-EL: financial support for research, travel cost reimbursement; Oticon Medical: financial support for research, travel cost reimbursement.
Ethical statement
The present study was approved by the Ethics Commission Freiburg (No. 560-19).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Speck, I., Gundlach, E., Schmidt, S. et al. Auditory capacity of the better-hearing ear in asymmetric hearing loss. Eur Arch Otorhinolaryngol 281, 2303–2312 (2024). https://doi.org/10.1007/s00405-023-08342-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08342-w